Abstract
Injury to the spinal cord results in disruption of neurons, cell membranes, axons, myelin, and endothelial cells. The aim of this study was to demonstrate the protective effect of magnesium sulfate on the blood-spinal cord barrier after acute spinal cord injury (SCI). This experiment was conducted in two parts. In the first, rats were injected intravenously with Evans blue 2 h after SCI. The laminectomy-only group had no trauma. Contusion injury (50 g-cm) was applied to the trauma and treatment groups. Magnesium sulfate (600 mg/kg) was given to the treatment group immediately after injury. For the second part, clinical evaluations were performed 24 h post surgery. Then, following Evans blue injection, spinal cord samples were obtained from the laminectomy-only, trauma, and treatment groups. For the control group, nontraumatized spinal cord samples were taken after Evans blue injection following clinical examination. Laminectomy did not affect the spinal cord Evans blue content in 2-h and 24-h groups. The trauma increased tissue Evans blue content, and 24-h samples showed more remarkable tissue Evans blue content, suggesting secondary injury. Application of 600 mg/kg of magnesium resulted in lower Evans blue content in the spinal cord than with injury. Remarkable clinical neuroprotection was observed in the treatment groups. Magnesium sulfate showed vaso- and neuroprotective properties after contusion injury to the rat spinal cord. The authors also demonstrated secondary injury of the blood-spinal cord barrier with the Evans blue clearance technique for the first time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary injury is initial mechanical damage to the spinal cord that results in disruption of neural and vascular structures, whereas secondary injury is progressive cell injury that collectively damages intact, neighboring tissue. It has been postulated that one of the most important factors precipitating post-traumatic neuronal degeneration is local vascular damage of the spinal cord microcirculation [1, 2, 3]. Decreased spinal cord microvascular patency and blood flow result in spinal cord ischemia beginning minutes after severe contusion or compression injury [4]. Severe vasospasm develops, and ruptured sulcal venules with numerous leukocytes in the vicinity of these vessels are observed up to 24 h after the injury (SCI) [5]. Blood-spinal cord barrier disruption and the inflammatory response expose neurons to blood cells and molecules that can be more damaging to intact and injured neighboring structures [6]. The histological effects include early hemorrhagic necrosis leading to major infarction at the injury site [3].
Although primary injury cannot be avoided, secondary injury may be prevented by pharmacological interventions. Magnesium is a well known neuroprotective agent in experimental brain injury and spinal cord ischemia [7, 8, 9, 10, 11]. It prevents glutamate toxicity by N-methyl-D-aspartate receptor blockage in neural structures [12]. Magnesium deficiency enhances free radical-induced intracellular oxidation and cytotoxicity in endothelial cells [13]. Glutamate accumulation and free radical generation in the abdominal aorta has been blamed for tissue damage after ischemia/reperfusion injury [14]. Magnesium also reverses experimentally delayed cerebral vasospasm after subarachnoid hemorrhage [15] and has a beneficial effect in eclampsia by preventing vascular changes resulting from vasoconstriction [16]. These data suggest a potential role of magnesium in the prevention of spinal cord vascular and neuronal injury.
Evans blue has been used extensively as an indicator of vascular permeability in heart, liver, pancreas, kidney, diaphragm, trachea, and lung parenchyma [17, 18, 19]. Blood-spinal cord barrier damage and increased microvascular permeability have been shown in syringomyelia, spinal cord transection, ischemia, and edema by photospectrometric and morphologic methods [20, 21, 22, 23]. Blood-brain damage and drug effects have also been quantified according to the extravasation of Evans blue in subarachnoid hemorrhage [24].
Restoration of vascular changes and prevention of blood-spinal cord barrier damage result in prevention of secondary neural injury to the spinal cord. The objective of the current study was to demonstrate the vasoprotective and neuroprotective effects of magnesium in the spinal cord after contusion injury. Tissue Evans blue content was used as an indicator of the blood-spinal cord barrier. Clinical evaluations were also performed to demonstrate the neuroprotective effect of magnesium after SCI.
Methods
Experimental groups
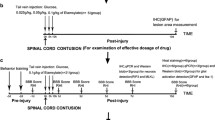
Sprague-Dawley rats were randomly allocated into seven groups of six rats each. The study was conducted in two parts. In the first part, the animals were killed after Evans blue application 2 h post trauma. The groups were divided as follows: controls in which 1-cm spinal cord samples were obtained immediately after laminectomy, a laminectomy-only group in which 1-cm noninjured spinal cord samples were obtained 2 h after laminectomy, a trauma group in which 1-cm spinal cord samples were obtained 2 h post trauma, and a treatment group in which 600 mg/kg single doses of magnesium sulfate (Biofarma, Istanbul, Turkey) were introduced immediately after induction of SCI and samples of which were obtained 2 h after the trauma.
In the second part of the experiment, animals were killed 24 h post trauma and divided into laminectomy-only, trauma, and treatment groups. Spinal cord samples were taken after 10 min of perfusion with Evans blue following clinical examinations. The control group from the first part was also used as a control in the second part. Clinical evaluations of the rats were performed only in the second part of the study.
Surgical procedure
Female Sprague-Dawley rats weighing 220–270 g were used. The surgical procedure was performed under general anesthesia induced intramuscularly by 10 mg/kg of xylasine (Bayer, Istanbul, Turkey) and 60 mg/kg of ketamine hydrochloride (Parke Davis, Istanbul, Turkey). The rats were placed in a prone position. Following T6–10 midline skin incision, paravertebral muscles were dissected. The T7–9 spinous processes were removed, and laminectomy was performed. The meninges were left intact. Spinal cord contusion injury, produced by the weight drop method of Allen [25], was 50 g-cm. After the surgical and traumatic interventions, the surgical wounds were closed in layers with silk sutures.
Application of Evans blue and sample preparation
For control groups, the rats were anesthetized with the combination of ketamine and xylasine, as described above, and Evans blue (Merck, Darmstadt, Germany) was introduced. Animals on which surgery had been performed previously were reanesthetized. Evans blue was introduced to the rats 2 h after operations for the first part and 24 h after operations for the second part.
The jugular veins were dissected after longitudinal cervical skin incision. Evans blue was dissolved in 0.9% NaCl at a concentration of 2 g/100 cc, and 50 mg/kg of this was given to each rat. A 27-gauge dental needle was used to introduce the Evans blue through the jugular veins. Intracardiac perfusion was performed with 75 cc of saline solution at minute 10 of Evans blue administration. Then the animals were placed in a prone position. The skin was opened and the dura incised longitudinally above the laminectomized spinal cord. Spinal cord samples were taken from the operated spinal cord areas. It was ensured that precisely the same size of spinal cord tissue samples, 1 cm each, was taken to avoid fluctuation in the ratio of traumatized to nontraumatized spinal cord segments. The tissue samples were kept at −20°C until spectrophotometric evaluation.
Determination of spinal cord Evans blue content
The tissues were weighed and their dye content was extracted in formamide at room temperature for 18 h. The absorbance of extracted dye was measured at 620 nm using a spectrophotometer. Dye content was expressed in terms of μg dye per g wet tissue. A standard curve was estimated, and the absorbance of 1 μg dye corresponded to 0.062. The corrections were made as follows. Tissue dye content was first corrected to show the absorbance of each sample for 1 g of wet tissue (absorbance of dye per g wet tissue). For the second correction, these values were converted into μg dye per g wet tissue. The observers performing spectrophotometric evaluation were blinded.
Functional evaluation
Behavioral evaluation was applied to the rats in the 24-h groups. Hind limb functions were assessed by the inclined plane (IP) technique of Rivlin and Tator [26], by the Basso, Beattie, and Bresnahan (BBB) scoring system described by Basso et al. [27], and by a modified Tarlov scale [28]. The BBB scale includes 21 different levels of movements of the hind limbs. Average BBB scores of both legs were examined. The Tarlov scale presents 5 as a maximum score. Observers performed the evaluations in a blinded fashion.
Statistical analysis
The Mann-Whitney U test was used to compare tissue Evans blue content between control and laminectomy, control and trauma, trauma and treatment, and control and treatment groups for 2 h and 24 h. It was also used for comparison of clinical results of all groups. Comparison of spinal cord tissue Evans blue contents was performed with Wilcoxon's signed rank test. The data were expressed as means ± standard deviation. Probability values lower than 0.05 were considered statistically significant.
Results
Results are shown in Table 1. There was no difference between control and laminectomy groups for all variables in 2-h and 24-h groups (P>0.05). There was a significant difference between control and trauma groups for tissue Evans blue content at 2 h and 24 h (P<0.01) and for clinical findings at 24 h (P<0.01). Trauma significantly raised spinal cord Evans blue content and significantly lowered clinical results. There was also a significant difference between trauma and treatment groups in tissue Evans blue content at 2 h and 24 h (P<0.01) and clinical findings of the 24-h groups (IP P<0.01, BBB P<0.05, Tarlov P<0.05). Magnesium treatment prevented high Evans blue content of the spinal cord and worsening of clinical results. There was significant difference between control and treatment groups in tissue Evans blue content at 2 h and 24 h (P<0.01) and clinical findings of the 24-h groups (IP P<0.05, BBB P<0.01, Tarlov P<0.01). Tissue Evans blue content increased with time following SCI. There was a significant difference between 2-h and 24-h trauma groups (P<0.05). This progressive vascular damage indicated secondary injury.
Discussion
Laminectomy did not increase spinal cord blood-spinal cord barrier permeability at either time interval or affect clinical findings at 24-h evaluation. We have previously shown that laminectomy did not damage ultrastructure, and that finding correlates well with the present study [29]. Although laminectomy has been shown to reduce spinal cord blood flow, the degree of this reduction has been shown insufficient to affect adversely the spinal cord energy metabolism [30, 31]. We conclude that laminectomy has no injurious effect on spinal cord histology, energy metabolism, clinical functions, or blood-spinal cord barrier perfusion in experimental studies.
Trauma increased spinal cord Evans blue content at both time intervals. Moreover, the difference in this content between the 2-h and 24-h trauma groups demonstrated progression of blood-spinal cord damage with time, which proves the theory of secondary vascular injury in SCI (Fig. 1). Magnesium treatment decreased blood-spinal cord barrier damage at 2 h and 24 h after contusion injury, and spinal cord Evans blue content did not increase with time in treatment groups. These findings prove that magnesium sulfate exerts a vasoprotective effect on spinal cord vasculature after injury. These results of spinal cord Evans blue content are also supported by clinical findings, which are also better in groups treated with magnesium.
Graph showing the spinal cord tissue Evans blue contents in control, laminectomy, trauma, and treatment groups for 2 h (white bars) and 24 h (gray bars). Secondary injury was seen to differ significantly (P<0.05) between 2-h and 24-h results of trauma groups (represented with asterisks). Bars show spinal cord tissue Evans blue contents in μg dye per g wet tissue, and vertical lines show standard deviations of the mean
Magnesium may prevent blood-spinal cord leakage by antagonism of glutamate in the endothelium. Delbarre et al. showed that ischemia-reperfusion insult caused a significant increase in the amount of glutamate and free radical formation in the aorta of gerbils [14]. They suggested that a simultaneous increase in glutamate and free radical formation might be similar to that observed in nervous tissues. The oxidative inactivation in glutamine synthetase by oxidative events might be one reason for increased glutamate [32].
It was proposed that the first target of free radicals during ischemia is the vascular system, especially endothelium [14]. Magnesium is believed to decrease lipid peroxidation by-products by an indirect action which may be glutamate antagonism [1, 8]. Dickens et al. demonstrated that endothelial cells grown in low magnesium were more susceptible to oxygen radical-mediated lipid peroxidation [13]. These data imply that magnesium plays a key role in mediating free radical and glutamate injury in vascular structures after SCI. Our results support this hypothesis by demonstrating protection of the blood-spinal cord barrier with magnesium given exogenously. It is also possible that magnesium exerts additional vasoprotection by decreasing free radical generation through glutamate antagonism in neural structures in the vicinity of vascular structures.
Magnesium may also cause dilatation of vessels supplying the spinal cord by stimulating endothelial prostacyclin release [33]. Ram et al. showed that magnesium dilates normal cerebral arteries as well as those with delayed spasm secondary to subarachnoid hemorrhage [15]. In this study, topical application of magnesium resulted in more vascular dilatation than the intravenous route. Concerning the study by Simpson et al., who showed the neuroprotective effect of magnesium via intrathecal administration in spinal cord ischemia, both routes may be used in treating SCI [10]. Sadeh et al. also suggested that magnesium, which has a beneficial effect in eclampsia, relieves cortical, periventricular, basal ganglia, and pons hemorrhages resulting from vasoconstriction [16]. They proposed that the mechanism underlying the action of magnesium on vasospasm may be attributed to magnesium's calcium antagonism.
Calcium plays an essential role in arterial tone and vasospasm [34]. Mg2+ is a bivalent anion resembling Ca2+ and therefore a competitive antagonist of the latter. Magnesium results in neuromuscular synapse blockage and skeletal muscle paralysis via competition with calcium in the presynaptic membrane. Mg2+ and Ca2+ also have opposite effects on vascular tone. An increase in calcium concentration results in vasospasm of isolated cerebral arteries, and this effect is alleviated by increasing the magnesium concentration [35, 36]. Magnesium also antagonizes Ca2+ at the N-methyl-D-aspartate subtype of glutamate receptor site and decreases calcium influx into smooth muscle cells [37]. Although the present study did not concentrate on spinal cord blood flow, we presume that magnesium may increase blood flow via its vasodilative effect. Studies are needed to demonstrate this effect in future SCI experiments.
A variety of reports demonstrate the effectiveness of magnesium treatment in experimental spinal cord ischemia [8, 9, 10]. However, until now, only one showed the beneficial effect of magnesium by improved electrophysiological results and decreased lipid peroxidation by-products after SCI [38]. Suzer et al. showed the beneficial effect of magnesium in compression SCI, and the results in our contusion injury model correlate well with their results.
In vivo studies demonstrating the effects of magnesium on spinal cord ischemia and injury are outlined in Table 2. According to this information, we conclude that all experiments showed obvious clinical, histopathologic, electrophysiologic (somatosensory evoked potentials), and biochemical (malondialdehyde) neuroprotection with magnesium treatment. This finding correlates well with the present study. The reason why 100 mg/kg of magnesium improved histologic, clinical, and electrophysiologic findings in ischemic spinal cord injury may be found in the injury model used. Contusion or compression injuries may cause more severe tissue damage and require more magnesium concentration in injured cord segments. Differences in species are also an important factor, and ischemic injuries were performed in rabbits and contusion-compression injuries in rats. Magnesium was administered 10 to 30 min before ischemic injury, but it was given after injury in traumatic SCI models. This may be another factor influencing dosing regimens. It is not possible to conclude whether the route of magnesium application influences the neuroprotective effect of the drug. However, the studies in which 100 mg/kg of magnesium was found to be effective used the intravenous route. We conclude that, although magnesium is very effective at 600 mg/kg, pharmacokinetic and dose-response studies should be performed to determine the most effective dosing regimen in human.
In summary, we conclude that
-
1.
Laminectomy has no injurious effect on the blood-spinal cord barrier in experimental SCI
-
2.
Blood-spinal cord barrier damage increases after injury with time, which indicates secondary injury; in this experimental setting, the secondary injury of vascular structures and blood-spinal cord damage were demonstrated by Evans blue for the first time
-
3.
Magnesium sulfate at the dose of 600 mg/kg protects the blood-spinal cord barrier and neural structures of the spinal cord from secondary injury.
Coupled with our results, the fact that magnesium sulfate is a well-known drug approved for the treatment of many clinical conditions and experimental neurotrauma models suggests that magnesium may have a role in the treatment of SCI in humans.
References
Dumont RJ, Okonkwo DO, Verma S, Hurlbert RJ, Boulos PT, Ellegala DB, Dumont AS (2001) Acute spinal cord injury, part I: pathophysiologic mechanisms. Clin Neuropharmacol 24:254–264
Mautes AEM, Weinzierl MR, Donovan F, Noble LJ (2000) Vascular events after spinal cord injury. Phys Ther 80:673–687
Tator CH, Fehlings MG (1991) Review of the secondary injury theory of acute spinal cord trauma with emphasis on vascular mechanisms. J Neurosurg 75:15–26
Hall ED, Wolf DL (1986) A pharmacological analysis of the pathophysiological mechanisms of posttraumatic spinal cord ischemia. J Neurosurg 64:951–961
Anthes DL, Theriault E, Tator CH (1996) Ultrastructural evidence for arterial vasospasm after spinal cord trauma. Neurosurgery 39:804–814
Schlosshauer B (1993) The blood-brain barrier: morphology, molecules, and neurothelin. Bioassay 15:341–346
Heat DL, Vink R (1999) Optimization of magnesium therapy after severe diffuse axonal injury in rats. J Pharmacol Exper Ther 288:1311–1316
Lang-Lazdunski L, Hearteaux C, Dupont H, Widmann C, Lazdunski M (2000) Prevention of ischemic spinal cord injury: comparative effects of magnesium sulphate and riluzole. J Vasc Surg 32:179–189
Robertson CS, Foltz R, Grossman G, Goodman JC (1986) Protection against experimental ischemic spinal cord injury. J Neurosurg 64:633–642
Simpson JA, Eide TR, Schiff GA, Clagnaz JF, Hossain I, Tverskoy A, Koski G (1994) Intrathecal magnesium sulphate protects the spinal cord from ischemic injury during aortic cross-clamping. Anesthesiology 81:1493–1499
Ustun ME, Gurbilek M, Ak A, Vatansev H, Duman A (2001) Effects of magnesium sulphate on tissue lactate and malondialdehyde levels in experimental head trauma. Intensive Care Med 27:264–268
Muir KW, Less KR (1995) A randomized, double blind, placebo controlled pilot trial of intravenous magnesium sulphate in acute stroke. Stroke 26:1183–1188
Dickens BF, Weglicki WB, Li YS, Mak IT (1992) Magnesium deficiency in vitro enhances free radical induced intracellular oxidation and cytotoxicity in endothelial cells. FEBS Lett 311:187–191
Delbarre B, Floyd RA, Delbarre G, Calinon F (1992) Glutamate accumulation and increased hydroxyl free radical formation in the abdominal aorta and heart of gerbil after ischemia/reperfusion insult. Free Rad Biol Med 13:31–34
Ram Z, Sadeh M, Shacked I, Sahar I, Hadani M (1991) Magnesium sulphate reverses experimental delayed cerebral vasospasm after subarachnoid hemorrhage in rats. Stroke 22:922–927
Sadeh M (1989) Action of magnesium sulphate in the treatment of preeclampsia-eclampsia. Stroke 20:1273–1275
Arakawa H, Kawikova I, Lofdahl CG, Lotval J (1992) Bradykinin-induced airway responses in guinea pig: effects of inhibition of cyclooxygenase and thromboxane synthetase. Eur J Pharmacol 229:131–136
Lehoux S, Plante GE, Sirois MG, Sirois P, D'Orleans-Juste P (1992) Phosphoramidon blocks big-endothelin-1 but not endothelin-1 enhancement of vascular permeability in the rat. Br J Pharmacol 107:996–1000
Martin CAE, Advenier C (1993) Effects of cromacalim on bradykinin, histamine and substance P-induced airway microvascular leakage in the guinea pig. Eur J Pharmacol 239:119–126
Kashiwaguchi S, Masaki K, Ikata T (1989) Experimental studies on permeability of tracers into the spinal cord. Paraplegia 27:372–381
Noble LJ, Maxwell DS (1983) Blood-spinal cord barrier response to transaction. Exp Neurol 79:188–199
Orendacova J, Marsala M, Marsala J (1991) The blood-brain barrier permeability in graded postischemic spinal cord reoxygenation in rabbits. Neurosci Lett 28:143–146
Wisselink W, Patetsios P, Panetta T, Ramirez JA, Rodino W, Kirwin JD, Zikra BA (1998) Medium molecular weight pentastarch reduces reperfusion injury by decreasing capillary leak in an animal model of spinal cord ischemia. J Vasc Surg 27:109–116
Smith SL, Scherch HM, Hall ED (1996) Protective effects of tirilazad mesylate and metabolite U-89678 against blood-brain barrier damage after subarachnoid hemorrhage and lipid peroxidative neuronal injury. J Neurosurg 84:229–233
Allen AR (1911) Surgery of experimental lesion of spinal cord equivalent to crush injury of fracture dislocation of spinal column. A preliminary report. JAMA 57:878–880
Rivlin AS, Tator CH (1978) Effect of duration of acute spinal cord compression in a new acute cord injury model in the rat. Surg Neurol 10:39–43
Basso DM, Beattie MS, Bresnahan JC (1996) Graded histological and locomotor outcomes after spinal cord contusion using the NYU weight-drop device versus transection. Exp Neurol 139:244–256
Gale K, Kerasidis H, Wrathall JR (1985) Spinal cord contusion in the rat: behavioral analysis of functional neurologic impairment. Exp Neurol 88:123–134
Kaptanoglu E, Caner HH, Surucu SH, Akbiyik F (1999) Effect of mexiletine on lipid peroxidation and early ultrastructural findings in experimental spinal cord injury. J Neurosurg (Spine 2) 91:200–204
Anderson DK, Means ED, Waters TR (1980) Spinal cord energy metabolism in normal and postlaminectomy cats. J Neurosurg 52:387–391
Anderson DK, Nicolosi GR, Means ED, Hartley E (1978) Effects of laminectomy on spinal cord blood flow. J Neurosurg 48:232–238
Oliver CN, Starke-Reed PE, Stadtman ER, Liu GJ, Carney JM, Floyd RA (1990) Oxidative damage to brain proteins, loss of glutamate synthase activity, and production of free radicals during ischemia/reperfusion induced injury to gerbil brain. Proc Natl Acad Sci U S A 87:5144–5147
Nadler JL, Goodson S, Rude RK (1987) Evidence that prostacyclin mediates the vascular action of magnesium in humans. Hypertension 9:379–783
Hubschmann OR, Nathanson DC (1985) The role of calcium and cellular membrane dysfunction in experimental trauma and subarachnoid hemorrhage. J Neurosurg 62:698–703
Altura BT, Altura BM (1982) The role of magnesium in etiology of strokes and cerebrovasospasm. Magnesium 1:277–291
Miura K (1988) Changes in Mg++ concentration of CSF after subarachnoid hemorrhage and Mg++ effects on the contractions of bovine cerebral artery. No Shinkei Geka 16:1251–1259
Rothman SM, Olney JW (1987) Excitotoxicity and the NMDA receptor. Trends Neurol Sci 10:299–302
Suzer T, Coskun E, Islakel H, Tahta K (1999) Neuroprotective effect of magnesium on lipid peroxidation and axonal function after experimental spinal cord injury. Spinal Cord 37:480–484
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kaptanoglu, E., Beskonakli, E., Solaroglu, I. et al. Magnesium sulfate treatment in experimental spinal cord injury: emphasis on vascular changes and early clinical results. Neurosurg Rev 26, 283–287 (2003). https://doi.org/10.1007/s10143-003-0272-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-003-0272-y