Abstract
Purpose
To test the hypothesis that an automated post-processing workflow reduces trauma panscan exam completion times and variability.
Methods
One-hundred-fifty consecutive trauma panscans performed between June 2018 and December 2019 were included, half before and half after implementation of an automated software-driven post-processing workflow. Acquisition and reconstruction timestamps were used to calculate total examination time (first acquisition to last reformation), setup time (between the non-contrast and contrast-enhanced acquisitions), and reconstruction time (for the contrast-enhanced reconstructions and reformations). The performing technologist was recorded and accounted for in analyses using linear mixed models to assess differences between the pre- and post-intervention groups.
Results
Exam, setup, and recon times were (mean ± standard deviation) 33.5 ± 4.6, 9.2 ± 2.4, and 23.6 ± 4.7 min before and 27.8 ± 1.5, 8.9 ± 1.4, and 18.9 ± 1.7 min after intervention. These reductions of 5.7 and 4.7 min in the mean exam and recon times were statistically significant (p < 0.001) while the setup time was not (p = 0.49). The reductions in standard deviation were statistically significant for exam and recon times (p < 0.0001) but not for setup time (p = 0.13). All automated panscans were completed within 36 min, versus 65% with the traditional workflow.
Conclusion
Automation of image reconstruction workflow significantly decreased mean exam and reconstruction times as well as variability between exams, thus facilitating a consistently rapid imaging assessment, and potentially reducing delays in critical management decisions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The golden hour concept refers to the first hour after a major traumatic injury in which early definitive treatment is most likely to improve clinical outcome [1, 2]. Within this critical early window, rapid assessment and triage of the injured patient are necessary to guide initial management decisions and treatment plans. Diagnostic imaging plays a crucial role in expediting this process by defining the nature and severity of the injuries [3].
Imaging of trauma patients typically includes a computed tomography (CT) trauma panscan of the head, cervical spine, chest, abdomen, pelvis, and thoracic and lumbar spine, with additional scan regions and contrast phases added as relevant. Trauma panscan protocols vary in their incorporation of arterial phase imaging, single pass or anatomically segmented acquisition, single or split bolus techniques, and use of dual-energy CT [3,4,5,6,7]. Considerations in protocol design include scan time, artifacts, radiation dose, and patient positioning [8,9,10].
In order to most rapidly guide patients with severe injuries to emergent surgery or intervention, trauma CT workflow must be optimized to expedite image availability and review. Trauma CT is one of the most challenging and time-sensitive processes in the ED but is also an inherently time-consuming multi-step process of image acquisition and post-processing often yielding 20–40 reconstructed image series comprising 2000–4000 images of multiple anatomic regions in multiple imaging planes.
Trauma panscan image acquisition requires coordination between multiple team members, including emergency medicine and trauma surgery physicians, nurses, radiologists, and technologists. Technologists must prepare the patient for the exam, which includes positioning the patient, confirming suitable IV placement, setting up the power injector, and appropriate CT protocol selection and configuration for multi-part exam acquisition. Image post-processing is also time-intensive as it requires technologists to manually prescribe image reconstructions and to align multiplanar reformations to the patient’s anatomy, which is made more challenging with monitored trauma patients who are difficult to position or have severe injuries limiting their mobility. This alignment step is critical for high-quality diagnostic images and ease of interpretation and must be performed individually for each image series within each of the scanned body regions.
Investigators creating trauma CT protocols for use in mass casualty incidents have primarily relied upon rapid preliminary interpretations from axial images alone, with one study incorporating partially automated reconstructions to decrease the burden on technologists [11, 12]. However, in the more usual trauma imaging scenario in which system resources have not been overwhelmed, multiplanar reformations remain critical components.
Recently, developed scanner technologies that allow for automated anatomic alignment of image reformations hold promise in streamlining the trauma panscan post-processing workflow. These software-driven workflow tools can replace the repetitive manual steps required to create image reformations in a traditional technologist-driven workflow. To this end, the purpose of this study was to test the hypothesis that an automated post-processing workflow reduces trauma panscan exam completion times and variability.
Materials and methods
This HIPAA-compliant study was approved by the institutional review board with waiver of informed consent for retrospective medical record review.
Setting
All CT examinations were performed at a level 1 trauma center with over 70,000 patients visits per year. A dedicated emergency radiology division provides 24/7 attending coverage, along with residents and emergency radiology fellows. Live review of trauma scans is performed at the scanner console for immediate communication of the most critical results, with full interpretations performed once all images are available in PACS.
Cohort
The final cohort included 150 trauma panscans performed between June 2018 and December 2019. Seventy-five consecutive scans were included immediately prior to implementation of the automated software-driven workflow. Following workflow implementation, a 6-month training period allowed technologists to acclimate to the new workflow, after which an additional 75 consecutive scans were included. The cohort was identified by PACS search for trauma panscans, with exclusions delineated in the flow diagram of Fig. 1: (1) incomplete exams lacking any of the component body regions of a panscan, as might occur if the patient had undergone partial imaging at an outside institution; (2) exams containing additional scan parts beyond the baseline panscan, and these exclusions ensured that all scans contained identical component parts; (3) exams performed immediately before or after a CT angiogram or another trauma, to prevent confounding in timestamp interpretation from residual reconstruction jobs pending between patients; (4) Non-contrast scans, as this impacts scan acquisition timing; (5) exams in the post-intervention cohort in which the technologist interfered with the automated reconstruction workflow, identified by series time stamps deviating from the programmed sequence. Additional consecutive scans were added until the final number included was 75 in the pre- and post-intervention groups. All scans in both groups were performed on the same ER scanner (Flash, Siemens, Forchheim Germany).
Total number of exams in the traditional cohort (left) and automated cohort (right). Examinations were excluded if they were incomplete (a body part was missing), contained additional scan parts beyond the routine panscan, were immediately preceded or followed by an examination with high image count (i.e., CTA or trauma panscan) or were performed without contrast. Examinations in the automated workflow cohort were also excluded if the technologist interrupted the prescribed automated workflow sequence
Image acquisition and post-processing workflow
Traditional manual post-processing workflow
For the purposes of this study, the standard trauma panscan is defined as non-contrast CT of the head and cervical spine, followed by contrast-enhanced CTA of the chest and abdomen, and a portal venous phase of the abdomen and pelvis, including reconstruction of dedicated thoracic and lumbar spine images. The solid abdominal organs are included in both the CTA and portal venous phases to allow characterization of vascular injuries. The top of Fig. 2 outlines the acquisition and post-processing sequence of the manual workflow: technologists begin with a lateral planning projection radiograph of the head and neck, from which they prescribe scan ranges and field of view for the head and cervical spine CT, and perform these acquisitions. For initial preliminary review at the scanner, the head CT is reconstructed in the axial plane and the cervical spine CT in axial and sagittal planes. Head dual-energy CT source images are sent to a freestanding server (Syngo.via, Siemens, Forchheim Germany) for automated dual energy post-processing.
Sequence of events during a routine trauma panscan using the traditional workflow (top) and automated workflow (bottom). Exam time is defined as the time from the first image acquisition to the last image reconstruction (blue box). Setup time is defined as the interval between the non-contrast and contrast-enhanced portions of the examination (red box). Reconstruction time is defined as the time from the first contrast-enhanced image acquisition to the last image reconstruction (green box). Note the differences in head and c-spine acquisition order between manual and automated workflows. The “Recon” boxes indicate the order in which the reconstruction jobs were started
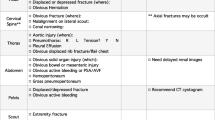
Following head and c-spine acquisition, there is a pause in the scanning process denoted the “setup time,” during which a radiologist performs a preliminary review at the scanner for major injuries and to assess the need for additional scanning (rescanning to resolve motion artifacts, or addition of a neck CTA for injuries that increase likelihood of blunt cerebrovascular injury). At the same time, the technologist initiates the remaining head and c-spine reconstruction jobs, connects the IV contrast power injector, and positions the patient for the subsequent scans. Image reconstructions are detailed in Table 1.
After the setup time, frontal and lateral planning projection radiographs of the torso are performed, from which the technologist prescribes the chest and abdomen CTA and the portal venous phase abdomen and pelvis scans. Following acquisition, these images are reconstructed in the axial plane for preliminary review, from which the radiologist assesses major injuries and determines the need for delayed imaging (most commonly to exclude urine leak from renal injury) or a CT cystogram with retrograde filling via Foley catheter for suspected bladder injury. The technologist manually prescribes and initiates the remainder of the reconstructions and reformations. These include thin images of the chest and dual-energy source images of the abdomen and pelvis that are sent to Syngo.via for automated rib cage unfolding and DECT post-processing, respectively. Thoracic and lumbar spine reformations are made from the chest and abdominopelvic acquisitions. Bone algorithm thoracic spine images include the ribs in the coronal plane and the sternum in the sagittal plane. Bone algorithm coronal lumbar spine images include the hips. Axial bone algorithm cervical, thoracic, and lumbar spine reconstructions are coned-in for better resolution. Other image reconstructions are detailed in Table 1.
Automated software-driven post-processing workflow
The study intervention was incorporation of a software-driven post-processing workflow that performs fully automated reformations with anatomy alignment on the scanner console (Fast Planning, Siemens, Forchheim, Germany). Head CT double oblique axial images are aligned to the skull base, with orthogonal coronal and sagittal reformations. In the torso, coronal and sagittal reformations are automatically aligned to the anatomy. At present, the software only performs reconstruction jobs that include the entire scanned field of view. Coned-in axial reconstructions of the spine must be performed manually. Cervical spine multiplanar reformations must also be performed manually, since the thin overlapping axial reconstructions used in the background to create the reformats have inadequate pixel resolution when the 512 × 512 matrix is spread over a full shoulder-to-shoulder field of view.
The bottom of Fig. 2 delineates the acquisition and post-processing workflow sequence of the automated workflow. The cervical spine acquisition was moved to the beginning so that the manually performed axial and sagittal cervical spine images are started before the head CT acquisition, avoiding the need to wait for all of the head CT automated reconstructions to complete. Head CT acquisition and automated reconstructions proceed next and typically complete during the setup time, avoiding downstream workflow bottlenecks. The remaining manual cervical spine reconstructions and the coned-in axial thoracic and lumbar spine reconstructions are prescribed while the automated torso reconstruction jobs are underway and are completed last, when CPU resources become available.
Technologists were instructed not to stop any of the automated reconstruction jobs, either to change the order of the jobs or to manually adjust anatomic alignment or field of view. During this training period, radiologists confirmed that the automatically aligned reformations were adequate in coverage and alignment, prior to proceeding with the post-intervention assessment phase.
Data collection
Patient demographic information was collected, including age and gender. The performing technologist was recorded for each scan. Overall Imaging turnaround (defined as exam order to report finalization) consists of two separable components: the technical component from exam order to exam completion, and the interpretive component from exam completion to report finalization. The focus of this study was on determining availability of imaging to the radiologist, so data collection focused purely on timestamps within the technical portion of the process. Digital Imaging and Communications in Medicine (DICOM) tags were recorded to identify image acquisition and series creation time stamps. The image acquisition time (DICOM tag 0008,0032) is the time during which the x-ray tube is turned on during scan acquisition and was recorded from the first image in the axial series for each scan part. The series time (DICOM tag 0008,0031) is the timestamp at which the final image in each series is created.
Recorded data included first image acquisition time and last series creation time for each acquired body region. For the chest and abdominopelvic scans, the last series creation times were for the thoracic and lumbar spine reformats, respectively. These timestamps were used to calculate the following intervals: exam time was defined as the total examination duration and was calculated as the difference between the first image acquisition time and the last series creation time. Setup time was defined as the interval between the non-contrast and contrast-enhanced acquisitions and was calculated by subtracting the last non-contrast acquisition time from the first image acquisition time of the contrast-enhanced chest and abdomen CTA. Reconstruction time (recon time) was defined as the amount of time required for the torso acquisitions and remaining reformats to be created after the setup time and was calculated by subtracting the first image acquisition time of the chest and abdomen CTA from the last series creation time.
Statistical analysis
Patient demographic information is presented using summary statistics and was compared using two-independent-sample t-tests (patient age) or Pearson’s chi-squared tests (patient gender). Exam time, setup time, and recon time were compared between the pre- and post-intervention groups using three separate normal linear mixed models with time period as the only predictor, a random intercept for technologist, and Kenward-Roger denominator degrees of freedom. This modeling approach was used to account for the correlation among times introduced by the presence of multiple procedures from the same technologists within and across time periods. The random intercept and the residual term were allowed to have heteroscedastic variance stratified by the time period. Model assumptions were assessed using marginal and conditional residuals and likelihood displacement. It was determined that, while a mild right skew was present in the time data, it had a limited influence on model results and assumptions, so all data were analyzed on their raw scale and presented using means. Levene’s test was used to compare the standard deviation of exam, setup, and recon times between time periods. For this analysis, if a technologist had more than one observation in the dataset, these observations were collapsed into a single observation by taking their mean so that each technologist contributed a single observation to this analysis. This was done to allow for a valid application of Levene’s test, and because the standard deviation of times between technologists was of primary interest rather than a measurement of variability that also included within-technologist variability. All models were refit adjusting for age and gender to determine if these potential confounders influenced estimated model parameters. No evidence of an age or gender effect was found, so only unadjusted results with age and gender removed from the models are presented for the purpose of parsimony. All hypothesis testing was two-tailed and p values less than 0.05 were considered statistically significant. Analyses were performed using SAS 9.4 (SAS Institute, Cary NC).
Results
Table 2 summarizes demographic information for the pre- and post-intervention cohorts.
Seventeen unique CT technologists performed the traditional cohort exams, while 30 unique technologists performed the automated reconstruction cohort exams. The mean number of procedures per technologist was 4.4 (range 1–12) in the traditional cohort and 2.9 (range 1–13) in the automated cohort.
Figure 3 shows the time points of all patients in both workflows. The variability in the order of the recon time stamps of the traditional manual workflow stems from variable practices in the order in which technologists complete the many reconstruction jobs. The automated workflow standardizes the sequence in which the reconstruction jobs are performed and eliminates the long outlier time points observed in the manual workflow.
As shown in Table 2 and Fig. 4, the mean exam, setup, and recon times using the traditional workflow were 33.5, 9.2, and 23.6 min compared to 27.8, 8.9, and 18.9 min using the automated workflow (p < 0.001, p = 0.49, and p < 0.001). Therefore, the automated cohort had a mean exam time 5.7 min less than the traditional cohort (95% CI −8.1 to −3.1); the mean set-up time was not statistically significantly different; the mean recon time was 4.7 min less in the automated cohort (95% CI −6.9 to −2.5).
Boxplot showing displaying the setup time, recon time, and exam time for the traditional and automated workflow. Each datapoint is represented by a round circle with the x representing the mean for each dataset. Each box consists of the 25th to the 75th percentile at its lower and upper margins, respectively, and represents the interquartile range. The horizontal line through each box represents the 50th percentile. The lower and upper whiskers represent the minimum and maximum values sans outliers, respectively, which are represented by datapoints above the upper whisker line
After mean-collapsing, the scans from the same technologist, the standard deviation of exam time decreased from 4.6 min in the traditional workflow to 1.5 min automated (Levene’s test p value <0.0001). The set-up time standard deviation decreased from 2.4 to 1.4 min but was not statistically significant (p = 0.13). The recon time standard deviation decreased from 4.7 to 1.7 min (p < 0.0001).
Figure 5 shows the proportion of exams completed within a designated duration. All automated exams were completed within 36 min using the automated workflow, compared to 65% with the traditional workflow.
Discussion
This study evaluated the impact on exam durations of transitioning trauma panscans to an automated reconstruction workflow and demonstrated a statistically significant decrease in both the mean exam times and the standard deviation of these exam times, thus achieving both a faster and more reproducible trauma panscan workflow.
The automated workflow reduced the mean exam completion time by 5.7 min, largely attributable to a 4.7-min decrease in mean torso image reconstruction time. There was no significant change in the setup time between the non-contrast and contrast-enhanced acquisitions, an expected finding as this interval includes workflow steps that are not inherently rate limited by image reconstructions.
The automated workflow also reduced variability in exam completion times, achieving statistically significant reductions in the exam time standard deviation from 4.6 to 1.5 min, largely driven by reduced variability in the torso reconstruction times. Variability in setup times did not change significantly.
The clinical impact of these results depends largely on practice model, specifically, whether a radiologist is present to check images live at the scanner. In the common scenario in which there is no radiologist present to review images in real-time at the scanner, faster image availability on PACS ties directly to faster identification and communication of critical findings. For those practices that station a Radiologist live at the scanner for trauma panscan review, preliminary communication of major injuries typically occurs in real-time, with further characterization and additional findings identified during full image review on PACS. In this practice model, a decrease in exam completion time may not speed communication of the findings most critical for immediate patient management, though it is not uncommon that additional clinically impactful findings are identified during PACS review of the complete image set. It is also important to emphasize that, while mean exam completion times only modestly improved from post-processing automation, the large decrease in variability eliminates the outlier delays that trigger the most consternation from the trauma surgery and emergency medicine teams during this inherently time-sensitive situation.
An unexpected challenge was early resistance from some of the more experienced technologists who had honed their own workflows to achieve exam times rivaling the most rapid automated exam times. However, these practices were not reproducible across the entire technologist group. This reluctance was overcome with time and by reinforcing the patient care goals of reproducible, high quality, and rapid scan output regardless of the experience level of the technologist operating the scanner.
The automated workflow script was not always followed, in part due to technologists being used to the traditional workflow of tweaking each prescribed reconstruction box, even by a few millimeters or a few degrees. Our radiologists were also accustomed to asking for additional reformats during preliminary review of the trauma, prompting technologists to pause the automated reconstructions to comply. A training period was thus required, during which both technologists and radiologists were trained not to interfere with the automated workflow. Nonetheless, there were a number of exams that needed to be excluded because of deviations from the automated workflow. For unclear reasons, other exclusions were more common in the post-intervention cohort, despite inclusion of a consecutive cohort. Specifically, exclusions are for incomplete examinations, additional scan parts, scans immediately preceding or following another high image count exam, and non-contrast exams. While the underlying causes of these exclusions are unclear, it is not expected to impact the measured workflow.
Our study has some limitations: it investigated a single institution trauma panscan protocol, so results are dependent on the particular contents of our protocol, and by the technology and processing power available on our specific ED CT scanner. The current version of the scanner software does not allow for creation of image reconstructions or reformations coned down to less than the full acquired field of view; when this becomes available, it would eliminate the need for any manual reconstruction tasks. An additional limitation was that the contributing technologists varied between the workflow groups. There were more unique technologists scanning on average fewer patients in the automated cohort. While confounding could theoretically remain if the either cohort’s technologist group as a whole were inherently faster or slower, there were too few exams performed by each technologist to perform a within-technologist analysis.
In conclusion, this study demonstrated that an automated CT reconstruction workflow for trauma panscans significantly reduces examination durations and variability, enabling rapid and reproducible delivery of images to radiologists and the trauma team. As time is of the essence in the evaluation of trauma patients, this intervention may have a meaningful clinical impact by facilitating a consistently rapid imaging assessment and potentially reducing delays in critical management decisions.
References
Blow O, Magliore L, Claridge J et al (1999) The golden hour and the silver day: detection and correction of occult hypoperfusion within 24 hours improves outcome from major trauma. J Trauma Acute Care Surg:2–12
Howard JT, Kotwal RS, Santos-lazada AR et al (2017) Reexamination of a battlefield trauma golden hour policy. J Trauma Acute Care Surg 84:11–18
Novelline RA, Rhea JT, Rao PM, Stuk JL (1999) Helical CT in emergency. Radiology 213:321–339
Soto JA, Anderson SW (2012) Multidetector CT of blunt abdominal trauma. Radiology 265:678–693
Hinzpeter R, Boehm T, Boll D et al (2017) Imaging algorithms and CT protocols in trauma patients: survey of Swiss emergency centers. Eur Radiol 27:1922–1928
Nguyen D, Platon A, Shanmuganathan K et al (2009) Evaluation of a single-pass continuous whole-body 16-MDCT protocol for patients with polytrauma. Am J Roentgenol 192:3–10
Wortman JR, Uyeda JW, Fulwadhva UP, Sodickson AD (2018) Dual-energy CT for abdominal and pelvic trauma. RadioGraphics:586–602
Sodickson AD (2012) Strategies for reducing radiation exposure in multi-detector row CT. Radiol Clin N Am 50:1–14
Gunn ML, Kool DR, Lehnert BE (2015) Improving outcomes in the patient with polytrauma. Radiol Clin N Am 53:639–656
Jeavons C, Hacking C, Beenen LF, Gunn ML (2018) A review of split-bolus single-pass CT in the assessment of trauma patients. Emerg Radiol 25:367–374
Korner M, Krotz M, Kanz K et al (2006) Development of an accelerated MSCT protocol (triage MSCT) for mass casualty incidents: comparison to MSCT for single-trauma patients. Emerg Radiol 12:203–209
Mueck F, Wirth K, Muggenthaler M et al (2016) Radiological mass casualty incident (MCI) workflow analysis: single-Centre data of a mid-scale exercise. Br J Radiol 89:1–6
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yu, H., Bay, C.P., Czajkowski, B. et al. Automated CT reformations reduce time and variability in trauma panscan exam completion. Emerg Radiol 29, 461–469 (2022). https://doi.org/10.1007/s10140-022-02031-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-022-02031-7