Abstract
The purpose of this study is to emphasize the imaging features of complications of gallstones beyond the cystic duct on ultrasound (US), enhanced and nonenhanced computed tomography (CECT and NECT), magnetic resonance imaging (MRI), magnetic resonance cholangiopancreatography (MRCP), and endoscopic retrograde cholangiopancreatography (ERCP). This article includes a brief overview of gallstone imaging and emerging trends in the detection of gallstones. This review article will highlight complications of gallstones, including choledocholithiasis, gallstone pancreatitis, acute cholangitis, Mirizzi syndrome, cholecystobiliary and cholecystoenteric fistulas, and gallstone ileus. Imaging findings and limitations of US, CT, MRI, and ERCP will be discussed. The review article will also briefly discuss the management of each disease. The presence of gallstones beyond the level of the cystic duct can lead to a spectrum of diseases, and emergency radiologists play a critical role in disease management by providing a timely diagnosis. Documenting the location of a gallstone within the common bile duct (CBD) in symptomatic cholelithiasis and the presence of acute interstitial edematous pancreatitis and/or ascending cholangitis plays a pivotal role in disease management. Establishing the presence of ectopic gallstones and biliary-enteric fistulae has a significant role in directing patient management.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Both acute and chronic gallbladder pathologies are commonly encountered in the emergency department (ED). Obstruction of the cystic duct by a gallstone accounts for most cases of acute cholecystitis and can lead to further complications including ischemia, hemorrhage, and/or transmural necrosis of the gallbladder wall. Apart from causing cholecystitis and cholecystitis-related complications, gallstones are also implicated in additional acute pathologies. Although a prior episode of acute, acute-on-chronic, or chronic cholecystitis is the precursor for most of the gallstone-related acute pathologies, the migration of gallstones beyond the cystic duct into the biliary tract, formation of biliary-enteric fistulae, passage of gallstones into the bowel, and rarely bowel perforation can cause challenging clinical and radiological scenarios in the emergent setting.
Our review article delineates the spectrum of diseases related to acute pathologies caused by the presence of gallstones beyond the gallbladder and cystic duct. We discuss the recent advances of imaging in the identification of gallstones. The critical disease entities due to gallstones beyond the cystic duct are choledocholithiasis, Mirizzi’s syndrome, cholecystobiliary and cholecystoenteric fistulas, gallstone pancreatitis, ascending cholangitis, and gallstone ileus/coleus. Ascending cholangitis and gallstone ileus are associated with significant morbidity and mortality when not diagnosed promptly and often warrant radiological evaluation [1, 2]. Radiological evaluation also plays a critical role in identifying ectopic gallstones and associated pathologies and related complications. Ultrasound (US) is the preferred imaging modality in cases of right upper quadrant (RUQ) pain and in demonstrating gallstones within the gallbladder. However, for acute entities related to gallstones beyond the cystic duct, the presenting clinical symptom determines the initial imaging modality. CECT is the most utilized imaging modality when abdominal pain is diffuse and when patients present with symptoms of bowel obstruction or peritonitis.
We describe clinical signs and symptoms, illustrate pertinent imaging findings, and address the implication of the imaging findings in the management of the patients presenting with acute pathologies secondary to the presence of gallstones beyond the vesicular infundibulum.
Overview of cholelithiasis
Cholelithiasis is the general term for gallstone formation, composed of cholesterol or bilirubin and calcium salts, at any location in the biliary tree. Cholecystolithiasis refers to stones in the gallbladder, and choledocholithiasis refers to stones in the common bile duct. The prevalence of gallstones ranges from 5 to 25% with greater prevalence in Western countries and older-aged women [3]. Nearly 80% of gallstones are “silent” and found incidentally on imaging when patients are worked up for another reason [4]. The risk of cholelithiasis becoming symptomatic and requiring treatment is 10% at 5 years [5]. When symptomatic, patients experience characteristic episodic, severe, or crampy right upper quadrant pain with other features including nausea, vomiting, or pain radiating to the back [6]. Biliary colic is defined as abdominal pain related to gallstones that obstruct the cystic duct or common bile duct. Meals, especially with high-fat content, stimulate the release of cholecystokinin, which causes gallbladder contraction. Gallstones can obstruct the cystic duct during contraction, causing signature intermittent postprandial RUQ pain. Patients with uncomplicated biliary colic generally have vital signs within normal limits and typically present with RUQ pain. Patients may also present with jaundice if the stone obstructs the common bile duct.
US accuracy in diagnosing cholelithiasis has been reported to be over 95%, proving to be an efficient tool to visualize gallstones [7]. Characteristic US findings of gallstones include a reflective echo from the gallstone’s anterior surface and posterior acoustic shadowing, differentiating it from non-shadowing structures like sludge, polyp, hemorrhage, or tumor [8]. Another specific sign of cholecystolithiasis is the “wall-echo-shadow sign,” or the “WES” triad, which represents the gallbladder wall, the stone’s echogenicity, and the acoustic shadow seen on the ultrasound [9].
Multidetector computed tomography (MDCT) is frequently utilized in the emergency department for diagnosing cholecystitis and complications while ruling out alternative diagnoses. Both CT and US have high specificity (93% and 95%, respectively) in identifying stones within the gallbladder; however, CT has lower sensitivity compared to US (81% vs. more than 95%, respectively) [10, 11]. Calcified (high calcium, low cholesterol) gallstones can easily be seen on CT, while noncalcified (low calcium, high cholesterol) gallstones are less visible because they are iso-dense to the surrounding bile [10]. Noncalcified stones can carry nitrogen gas, giving the “Mercedes-Benz sign” on MDCT [12]. Recent technological advances in dual-energy CT, including iodine-selective postprocessing techniques and virtual monochromatic imaging, help improve the efficiency of CT in detecting gallstones that are iso-dense to bile on conventional 120-kVp CT images [10, 13]. Dual-energy CT acquisition with virtual monochromatic imaging postprocessing both at low (around 40 keV) and high (around 190 keV) monoenergetic levels are performed to overcome the limitation of conventional CT imaging [10]. The energy-dependent X-ray attenuation curve of cholesterol-containing stones (which are usually radiolucent) is different from that of bile, and this phenomenon makes them distinctly identified on lower and higher keV virtual monochromatic images [14]. In a recent retrospective analysis, Bae et al. demonstrated a comparable efficacy in detection of gallstones and CBD stones by virtual non-contrast (VNC) images derived from dual-source DECT to true non-contrast (TNC) CT images [15]. One of the significant roles of DECT in evaluation of biliary stones is enabling the differentiation between the enhancing bile duct wall and hyperdense biliary stones such as gallbladder and /or CBD stones [15].
Magnetic resonance imaging (MRI)/magnetic resonance cholangiopancreaticography (MRCP) has high sensitivity of 90–94% and specificity of 95–99% in detecting gallstones [16]. On T2-weighted MR images and sequences, gallstones are hypointense surrounded by hyperintense bile. MR also has an added advantage in differentiating cholesterol stones and pigmented stones, as on T1-weighted images they appear hypointense and typically hyperintense, respectively. MRCP is limited in demonstrating gallstones smaller than 3 mm, with sensitivity of detecting these small gallstones decreasing to 64% [17].
Treatment for gallstones is generally for symptomatic patients and includes a low-fat diet, pain control, anti-emetics, and possibly outpatient laparoscopic cholecystectomy, depending on patient presentation. However, if symptoms are acute or suggest complication, alternative diagnostic and treatment modalities must be considered [18].
Choledocholithiasis
The presence of choledocholithiasis, stones in the common bile duct (CBD), is one of the most common abnormalities of the biliary tract. Gallstones are usually asymptomatic, but 10–15% of symptomatic patients with gallstones and biliary colic are estimated to have choledocholithiasis, with a reported incidence of 5.1/1000 patients in a community setting in 2006 [19, 20]. Furthermore, 10 to 20% of patients who undergo cholecystectomy can present with choledocholithiasis [21]. Extensive discussion on post cholecystectomy choledocholithiasis is beyond the scope of this article. However, identifying CBD stones in acute cholecystitis preoperatively is vital given the increasing use of laparoscopic approach compared to open cholecystectomy.
Contrary to gallbladder stones, a significant proportion of CBD stones cause symptoms such as RUQ pain, nausea, and vomiting [22]. Symptoms of choledocholithiasis arise when a stone obstructs the CBD and are mostly determined by the size of the stone. Smaller stones less than 5 mm in size can be clinically silent or cause transient pain and eventually pass into the duodenum via the ampulla of Vater [10]. Stones larger than 5 mm are less likely to pass and may obstruct the CBD. Patient presentation is similar to biliary colic and includes intermittent RUQ pain generally associated with nausea and vomiting, often lasting for several hours [23]. Patients have also reported episodes of jaundice that are associated with abdominal pain, and elevated bilirubin levels higher than 4 mg/dL [24].
The CBD caliber and location of stones in the CBD both play a significant role in the detection of choledocholithiasis in the ED, especially on the US. In one study, the estimated normal diameter of the CBD by ultrasound is 3.6 ± 0.26 mm for patients in the 60–85 age range, and 4.0 ± 0.25 mm for patients older than 85 years of age, which was below the accepted upper range of normal, 6–7 mm [25]. For choledocholithiasis, the sensitivity of ultrasound is very low and reported to be 22% [26]. Factors that decrease sensitivity include bowel gas artifact that may obscure an ampullary stone in the distal duct. A significant amount of bile may also be needed to differentiate the duct wall from adjacent structures (Fig. 1a and b) [26]. Hepatobiliary iminodiacetic acid is not usually indicated in the evaluation of choledocholithiasis. However, when performed to exclude underlying acute cholecystitis, normal flow into the bowel mitigates the likelihood of obstruction of the CBD (Fig. 1c).
CBD stones and no obstruction. 30-year-old female with recurrent episodes of biliary colic and normal serum bilirubin. Transverse US image of RUQ (a) shows stone in the gallbladder (arrow) and also stone with acoustic shadowing within the CBD (arrowhead). Longitudinal US image of RUQ (b) illustrates multiple gallstones along the CBD (arrowheads). HIDA scan (c) shows visualization of gallbladder and normal flow of radiotracer into small bowel without CBD obstruction
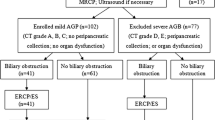
Advantages of CT imaging in the evaluation of choledocholithiasis include thin slices and multiplanar reconstructions, which improve detection of the attenuation differences between gallstones and the surrounding bile and soft tissue (Fig. 2a and c) [27]. MDCT has a reported sensitivity of 69–87% and specificity of 83–92% [10]. CT also aids in diagnosing the simultaneous occurrence of acute cholecystitis with choledocholithiasis (Fig. 2b) with one study demonstrating greater sensitivity of CT over US when detecting acute cholecystitis in patients who presented with additional pathologic findings like choledocholithiasis (85% vs. 68%, respectively, p = 0.043) [28]. Most modern emergency radiology departments utilize MDCT; unenhanced and contrast-enhanced MDCT can diagnose choledocholithiasis with an accuracy of 84–88% [29]. CT evaluation also helps in recognizing intrahepatic biliary ductal dilatation which suggests possible biliary obstruction secondary to choledocholithiasis (Fig. 2d). MRCP is an additional diagnostic tool in evaluating choledocholithiasis, with sensitivity and specificity up to 85% and 93%, respectively [30]. Generally, if US is unable to detect choledocholithiasis and clinical suspicion remains high, patients are treated with endoscopic retrograde cholangiopancreatography (ERCP), due to its high diagnostic and therapeutic capabilities [23]. Identification of CBD stones prior to cholecystectomy helps in preoperative assessment of patients and can determine who may benefit from ERCP prior to surgery and the optimal approach for cholecystectomy [21].
Distal CBD stone and acute cholecystitis. 81-year-old female with diffuse abdominal pain. Coronal CECT image (a) shows likely obstructing gallstone in distal CBD (arrowhead) and upstream dilatation of CBD (arrows). Axial CECT image (b) demonstrates distended gallbladder with enhancing wall (arrow) and trace pericholecystic stranding (arrowhead), representing acute cholecystitis (proven pathologically). Axial CECT image more caudally (c) shows additional dependent hyperdense stones in distal CBD (arrowhead). Axial CECT image more cranially (d) shows central intrahepatic biliary ductal dilatation (arrowheads), indicating the CBD obstruction
ERCP is considered the gold standard (sensitivity 83% and specificity 99%) for diagnosing choledocholithiasis, although drawbacks include an 8–12% operator-dependent complication rate including pancreatitis, bleeding, cholangitis, and perforation [31, 32]. ERCP is performed for treatment of choledocholithiasis by injecting contrast under fluoroscopy to visualize the obstruction, performing a sphincterotomy, and using papillary balloon dilation to aid in endoscopically removing the stone [22]. If endoscopy fails, alternative therapeutic measures include percutaneous treatment performed by interventional radiology (IR). Percutaneous treatment may be indicated for patients who have failed previous therapy, demonstrate heavy stone burden, and are not candidates for surgery or ERCP. Examples of percutaneous treatment include placement of a T-tube, cholecystostomy tube, and more recently, placement of a transhepatic tube that allows biliary stones to be extracted or expelled into the bowel [33]. A recent study investigated the safety and efficacy of percutaneous transcholecystic removal of common bile duct stones in 114 patients with choledocholithiasis and demonstrated a success rate of 84.2% with no major complications [34].
Gallstone pancreatitis
Gallstone/biliary pancreatitis is the second most common acute manifestation of gallstones after acute cholecystitis [35]. The incidence of interstitial edematous pancreatitis (IEP) ranges from 5 to 80 per 100,000 people [36]. Gallstones are the most common etiology of IEP across various populations, accounting for 40–60% of IEP diagnoses [37]. Men have an increased risk of developing acute gallstone pancreatitis; however, more women develop gallstones, so gallstone pancreatitis is more commonly observed in women [35].
Although not fully understood, the theorized pathophysiology of IEP from gallstones involves gallstone obstruction of the ampulla and reflux of bile into the pancreatic duct, resulting in increased pancreatic ductal pressure and unregulated pancreatic enzyme activity [16].
The classic clinical presentation of IEP is epigastric pain with radiation to the back with laboratory values demonstrating elevated serum amylase and serum lipase levels. Accurate diagnosis of IEP secondary to gallstones is important because it indicates intervention is needed for management/clearance of the obstructing calculus and preventing recurrence of pancreatitis. Coexistence of acute cholecystitis and IEP is rare but well documented in the literature [35]. Studies show that 30 to 50% of patients develop recurrent IEP after discharge, often with a more severe disease course on recurrence [37]. Imaging plays an important role in confirming the clinical diagnosis of IEP, determining the etiology, excluding alternative causes, demonstrating complications, and grading disease extent and severity.
Trans-abdominal US is the most common initial imaging modality for patients presenting with symptoms of IEP, given the underlying etiology of 50% of cases is gallstone disease. Trans-abdominal US can detect gallstones with over a 90% sensitivity in uncomplicated cases [38]. However, sensitivity drops to 67–78% in the setting of IEP secondary to gallstones, secondary to difficulty visualizing the retroperitoneal pancreas, bowel gas artifact, and when imaging patients with a large body habitus [39]. IEP is identified as an enlarged hypoechoic pancreas along with peripancreatic fluid (Fig. 3a–c). Diameter of the CBD is an important parameter for diagnosis, with studies showing a distended CBD of 9 mm or more almost always associated with the presence of gallstones [37]. Trans-abdominal US demonstrating a distended CBD with classic clinical manifestations is highly suggestive of a clinical diagnosis of IEP from gallstones. Pereira et al. observed that US findings alone cannot be used accurately to diagnose acute cholecystitis in the setting of IEP presumably due to accompanying local changes in pancreatitis including peritoneal free fluid and gallbladder wall edema, which alter the regular anatomy [35].
Gallstone pancreatitis. 41-year-old male with diffuse epigastric pain. US image of mid abdomen (a) shows diffuse hypoechoic pancreas (P) suggesting edematous pancreatitis. US image of GB (b) demonstrates multiple dependent gallstones (arrowheads). Axial CECT image (c) shows dependent calcified gallstones and interstitial edema of the pancreas with peripancreatic fluid (arrows). Coronal CECT image (d) shows tiny impacted gallstone in ampulla of Vater/sphincter of Oddi (arrowhead). ERCP image (e) outlines the biliary tract; sphincterotomy was performed
Contrast-enhanced CT is considered the gold standard for the diagnosis and staging of acute pancreatitis (both interstitial edematous and necrotizing pancreatitis). The pancreas may enhance uniformly in mild acute IEP, with the presence of increased attenuation in adjacent fat, referred to as “stranding” (Fig. 3c). CT may aid in localization of CBD stones with a sensitivity as high as 80% (Fig. 3d) [40]. Patient with persistent obstruction (more than 48 h) of the ampulla of Vater due to choledocholithiasis and biliary obstruction usually benefit from early ERCP (24 to 72 h) followed by sphincterotomy and extraction of biliary stones (Fig. 3e) [41]. Fluid and stranding are also commonly visualized along the mesentery, mesocolon, hepatoduodenal ligament, and in the peritoneal space (Fig. 4a and b). Pancreatic parenchymal necrosis and fluid collections are considered the most important imaging findings in necrotizing pancreatitis due to their prognostic relevance and indication for intervention. Nonenhancement of any portion of the gland is considered “necrosis.” CT is considered 100% specific for necrosis if over 30% of the gland is non-enhancing [42].
Coexistent acute cholecystitis and IEP. 52-year-old-female with diffuse abdominal pain. Axial CECT (a) shows distended gallbladder, gallbladder wall enhancement, and pericholecystic fluid (large arrow), represents acute cholecystitis. Also note dependent gallstone (small arrow). The pancreas is edematous (arrowhead) with peripancreatic fluid and inflammatory stranding (*) representing IEP. Coronal CECT image (b) shows a gallstone in proximal common bile duct (arrow). Note scattered fluid in the abdominal cavity (*)
Acute IEP can be treated with conservative management. However, if imaging suggests a gallstone etiology of the acute pancreatitis, accepted protocol suggests performing a laparoscopic cholecystectomy, as these patients run a 30–50% risk of recurrence within weeks of the first episode [43]. Simultaneous occurrence of acute cholecystitis and IEP (Fig. 4a and b) suggests the need for early administration of antibiotics, affects the choice of antibiotic, and indicates the need for early cholecystectomy [35, 44]. ERCP with biliary sphincterotomy and extraction of biliary stones is warranted as an urgent/emergent biliary drainage procedure in patients with gallstone pancreatitis complicated by persistent choledocholithiasis and biliary obstruction and particularly in patients presenting with acute cholangitis [41].
Acute cholangitis (ascending cholangitis) due to gallstones
Acute cholangitis is a potentially life-threatening emergency caused by acute inflammation and infection of the biliary system, usually secondary to partial or complete obstruction of bile ducts. Approximately 0.2% of cases of choledocholithiasis are at risk of acute cholangitis [45]. Obstruction of the CBD due to gallstones remains the leading cause of acute cholangitis accounting for up to 80% of cases [46]. Other causes of acute cholangitis include instrumentation of the biliary tree, stricture, malignant disease, and sclerosing cholangitis [46]. Bile is a sterile fluid, and continuous antegrade flow toward the duodenum, the protective effect of the sphincter of Oddi, the presence of bacteriostatic biliary salts, and the very low bacterial burden of the proximal jejunum and duodenum, generally protect against secondary infection of bile. Therefore, development of acute cholangitis requires stagnation of bile, increased intra-biliary pressure, and secondary bacterial contamination [1].
Known risk factors of cholangitis in patients with gallstones include patient age > 70 years, neurological disease, diabetes mellitus, and periampullary diverticula [1, 46]. Charcot’s triad was initially described in 1887 which constitutes intermittent fever, RUQ pain, and jaundice (“hepatic fever” as by Dr. Jean-Martin Charcot) [1]. In 1959, Reynold added two additional features, lethargy/mental confusion and shock, thus referring to Reynold’s pentad [47]. Despite historic description of clinical symptoms of acute cholangitis, clinical diagnosis is challenging as Charcot’s triad exhibits a high specificity and very low sensitivity. Charcot’s triad occurs in fewer than 75% of patients and blood cultures are positive in only 20 to 30% of cases [46]. Patients may be asymptomatic or present with pain, particularly in the elderly population, causing a delay in diagnosis or potentially misdiagnosis. Complications of acute cholangitis develop rapidly and include sepsis, hepatic abscesses, portal vein thrombosis, and bile peritonitis.
Imaging findings of acute cholangitis include both biliary and parenchymal pathologic changes (Fig. 5a and b). Biliary findings include ductal dilatation in the setting of obstruction. Cross-sectional imaging with CT or MR is also useful for identifying the underlying cause of obstruction (Fig. 5a and b). Intrahepatic biliary ductal dilatation may involve a segment of the biliary tree or diffuse involvement of the entire biliary tree. Extrahepatic biliary ductal dilatation and CBD wall thickening and enhancement are recognized imaging findings in a majority of patients (Fig. 5a) [46]. Bader et al. reported enhancement of intrahepatic bile duct walls in 92% of cases on MRI [48]. Parenchymal findings are secondary to extension of the inflammatory process to the periportal tissues and adjacent hepatic tissue. Parenchymal changes are better demonstrated by MRI and include increased T2-weighted signal in a peribiliary distribution. Liver abscesses occur in 24% of cases of acute cholangitis (Fig. 5b) [48]. Biliary sepsis and liver abscess indicate increased permeability of the acutely inflamed biliary epithelium.
Ascending cholangitis. Coronal CT image (a) shows hyperdense gallstones within the contracted gallbladder (large arrow) and another hyperdense gallstone in the distal CBD (arrowhead) causing upstream dilatation of CBD with enhancing walls (small arrows). Large-sized simple cyst noted in the right kidney (RC). Axial CT image (b) shows dilated intrahepatic bile ducts with irregular wall thickening (arrowheads) and well-circumscribed hypodense collection in anterior central hepatic region with enhancing rim (arrow) suggestive of liver abscess
Acute cholangitis is a critical condition and patients should be resuscitated first. The disease is a manifestation of infection and obstruction of the biliary system and the management needs to address both aspects. Intravenous fluids and antibiotics should be started as early as possible. Biliary drainage is equally important as biliary secretion of antibiotics is impaired due to high biliary ductal pressure in cholangitis. In cases of ascending cholangitis secondary to gallstones, sphincterotomy and stone extraction with or without trans-papillary biliary stent placement are recommended [49]. Concurrent acute bacterial cholangitis with acute cholecystitis is also reported and considered a gastrointestinal emergency that warrants immediate treatment initiation [50].
Mirizzi syndrome, cholecystobiliary and cholecystoenteric fistulas, and gallstone ileus
Mirizzi syndrome is characterized by extrinsic compression of the CBD due to a gallstone in the gallbladder neck, infundibulum, or cystic duct with surrounding inflammation and concurrent cholangitis [51]. Persistent obstruction can lead to recurrent inflammation, eventual mural thinning with necrosis and fibrosis, fusion to the adjacent CBD, and the formation of pressure ulcers leading to fistulous communications with the common bile or hepatic ducts, bowel, or rarely adjacent viscera [51,52,53,54,55]. Anatomic variants such as low cystic duct insertion, cystic duct in a parallel course with the CBD, and short cystic duct can predispose to this condition [52, 56, 57]. A 1963 study by Dietrich demonstrated a low insertion resulting in a parallel course in 18% of patients [58, 59].
The reported incidence of Mirizzi syndrome ranges from less than 1 to 5.7%, with higher incidence in developing countries [51, 52, 54]. Mirizzi syndrome typically occurs after long-standing gallstone disease with a mean duration of 29.6 years in one study with an average patient age of 59; over two-thirds of the cases in this series were in women [54]. Mirizzi syndrome has been associated with gallbladder cancer, possibly due to chronic inflammation and biliary stasis with the first report identifying cancer in 27.8% of Mirizzi syndrome patients [60].
In the most current Mirizzi classification system, type I refers to extrinsic compression of the common bile duct by an impacted gallstone, types II–IV refer to a cholecystocholedochal fistula secondary to an eroded gallstone involving one-third, two-thirds, and the entire circumference of the common bile duct, respectively, and type V refers to any type in the presence of cholecystoenteric fistula without (Va) or with (Vb) gallstone ileus [54, 61]. An additional study confirmed the association of Mirizzi syndrome and the development of cholecystoenteric fistula suggesting this is a disease spectrum rather than separate entities [54]. A simplified classification scheme has been suggested by Beltran based on earlier work by Solis-Caxaj and further linked to surgical approach [52]. Type 1 is external compression of the bile ducts only and treated with open or laparoscopic total or subtotal cholecystectomy. Type II includes the presence of a cholecystobiliary fistula with treatment being open total or subtotal cholecystectomy when less than 50% of the bile duct is involved (IIa) and open subtotal colectomy with bilioenteric diversion if greater than 50% of the bile duct diameter is involved (IIb). Type 3 includes a cholecystoenteric fistula with (IIIa) or without (IIIb) gallstone ileus and is treated with closure of the fistula or treatment of the gallstone ileus and the gallbladder according to primary subtype [52, 62].
Mirizzi syndrome remains a difficult clinical and imaging diagnosis to make but is important for surgical planning given the risk of intraoperative bile duct injury. In a case series by Shirah et al., US demonstrated gallstones in 100% of patients but only detected Mirizzi syndrome in 20.3% of patients, while ERCP and CT were diagnostic for Mirizzi syndrome in 26.6% and 21.9% of patients, respectively [63]. Mirizzi syndrome was only diagnosed at the time of surgery in 53.1% of patients [63]. While all patients diagnosed with US or intraoperatively were Csendes type 1, the patients initially diagnosed by US had shorter hospital stays, decreased morbidity, and had no conversions to open procedures [63]. Furthermore, a case series by Tan et al. demonstrated intraoperative bile duct injuries in 4 out of 24 patients (16.7%), all of whom did not have a preoperative diagnosis [64].
Sonographic findings may demonstrate an atrophic gallbladder and obstructing gallstone in the gallbladder neck or cystic duct causing extrinsic compression of the common hepatic duct, dilatation of the ducts proximal to the obstruction, and normal caliber CBD distal to the obstruction. While CT can identify the location and cause of the obstruction as well as assess the gallbladder wall and periductal inflammation, it is most useful in excluding an obstructing mass in the porta hepatis as the cause of biliary ductal dilatation (Fig. 6a) [52]. MRI/MRCP demonstrates similar findings and identifies the associated inflammation (Fig. 6b–d) [51]. MRI/MRCP is also useful in the exclusion of malignancy as well as identifying the presence of a cholecystobiliary fistula (Fig. 6d) [65]. ERCP is considered the gold standard for diagnosis and can easily demonstrate extrinsic compression by the impacted gallstones, visualize dilated proximal ducts and extrahepatic bile ducts, and accurately identify fistulae [66]. ERCP is also therapeutic with options including biliary drainage, stone removal, and stent placement often performed concurrently, although the procedure is invasive and has known complications [52]. In a 2018 literature review by Chen et al., a combination of two or more modalities were frequently used for diagnosis [66].
Mirizzi syndrome. Coronal CECT image (a) shows heterogeneously dense gallstone in the porta hepatis region (arrow) with air in the adjacent extrahepatic bile duct and in intrahepatic bile ducts (arrowheads). Coronal T2-weighted MR image (b) shows hypointense gallstone causing mass effect on hepatic duct (arrow). Coronal MRCP image (c) depicts narrowing of common hepatic and common bile duct (arrow) with upstream intrahepatic biliary ductal dilatation (arrowheads). Coronal delayed post contrast MR image (d) shows duodenal wall adherent to gallbladder wall (arrow), choledochoduodenal fistula was identified at surgery
Choledochoenteric fistulae allow passage of stones into the gastrointestinal (GI) tract and usually involve the duodenum (Fig. 7a and b) but the colon, stomach, and other portions of adjacent small bowel can be affected. Symptoms can be intermittent with jaundice and right upper quadrant pain absent in 1/3 of patients [56]. CT is instrumental in diagnosing biliary-enteric fistulas (Fig. 7a and b and Fig. 9b). Cholecystocolonic fistulas are usually secondary to cholecystitis, but they are very infrequent and typically form between the gallbladder and the hepatic flexure of the colon due to their proximity (Fig. 8a–d) [67]. MRI and MRCP are used extensively in the evaluation of biliary disease, particularly as newer techniques evolve with one series comparing MRI and MDCT demonstrating 100% identification of cholecystoenteric fistulae and small bowel obstructions with MRI [68].
Cholecystoenteric fistula. Axial CECT image (a) shows large pocket of air within the contracted gallbladder (arrow) and fistulous tract (arrowhead) communicating with the first part of the duodenum (D). Coronal CECT image (b) shows fistulous communication between gallbladder and duodenum (arrowheads) with minimal stranding in the porta hepatis. No gallstones were identified in the gallbladder; an ectopic gallstone was present in the distal ileum (not shown) causing bowel obstruction
Cholecystocolonic fistula: 65-year-old female presents with recurrent right upper quadrant pain. Axial CECT (a) image shows contracted gallbladder with wall enhancement and pericholecystic inflammatory stranding (arrow). Coronal CECT image (b) shows close proximity of hepatic flexure to the inferior pole of the gallbladder wall. Exam is limited due to motion and streak artifact from residual contrast in adjacent colon. Axial T2 Fat Sat image of upper abdomen (c) reveals gallbladder wall thickening with hyperintense pericholecystic fluid (arrow) as well as intraluminal gallstones (arrowhead). Coronal post contrast T1WI (d) shows gallbladder wall adherent hepatic flexure (arrow) raising possibility of choelcystocolonic fistula. Chronic cholecystitis and cholecystocolic (hepatic flexure) fistula were identified during surgery and subsequently open partial cholecystectomy with closure of cholecystocolonic fistula was performed
The passage of larger gallstones into the GI tract via fistulae can lead to gallstone ileus. However, some authors argue the term gallstone “ileus” is a misnomer as the bowel obstruction is mechanical rather than an adynamic ileus as the name suggests [2]. Stones less than 2–2.5 cm usually pass through the bowel whereas stones > 5 cm are more likely to become impacted and result in mechanical small bowel obstruction [56]. The most common sites of impaction include the terminal ileum and ileocecal valve [56, 69, 70]. More than 50% of cases are due to choledochoduodenal fistulas; however, cholecystocolonic and cholecystogastric fistulas can also result in bowel obstruction secondary to gallstones. Rare variations such as an inspissated mass formed by smaller gallstones causing bowel obstruction, mechanical large bowel obstruction caused by gallstones (gallstone coleus), and gastric outlet obstruction due to impacted gallstone in duodenum (Bouveret’s syndrome) have all been reported [71]. Historically, gallstone ileus was responsible for 1 to 5% of mechanical small bowel obstructions; however, in one study, the proportion of gallstone ileus causing mechanical bowel obstruction was less than 1% [72]. Overall, 0.3 to 0.5% of cholelithiasis patients develop gallstone ileus and 2 to 3% (when associated with cholecystitis episodes) develop biliary-enteric fistulas [73, 74]. The average age of presentation of gallstone ileus is 74 years and patients usually present with signs and symptoms of bowel obstruction, commonly preceded by biliary complaints [2, 71]. Late presentation from the onset of symptoms (average 4–8 days) and median delay between admission and surgical intervention of 2–37 days are the key challenges in the management of gallstone ileus patients [2, 72].
Abdominal radiographs are often the first-line imaging investigation when bowel obstruction is suspected and the sensitivity of abdominal radiographs for the diagnosis of gallstone ileus is between 40 and 70% [75] and may demonstrate Rigler’s triad, which includes air within the biliary tree (pneumobilia), evidence of small bowel obstruction, and ectopic radio-opaque gallstones [2]. On abdominal films, all three criteria of Rigler’s triad are observed only in 14–53% of cases of biliary ileus [76]. Rigler’s tetrad includes a change in location of the previously identified gallstone and Rigler’s pentad includes a dual air-fluid level in the right upper quadrant [2, 77]. Though sonography is often used in the evaluation of gallbladder pathology, it remains of limited use for bowel obstruction.
CT is universally accepted as the study of choice in bowel obstruction and in gallstone ileus. Yu et al. first described the CT diagnostic signs of gallstone ileus which include signs of small bowel obstruction, ectopic gallstone, and abnormal gallbladder (Fig. 9a–d) [78]. Although a frank fistulous communication between biliary tract and bowel can be occult, our experience suggests inflammation in the porta hepatis region in the setting of bowel obstruction related to gallstones should raise concern for occult biliary-enteric fistula. However, gallstone ileus in patients with no biliary-enteric fistula or gallbladder also has been reported [79]. Furthermore, CT has the advantage of determining the exact site of obstruction to guide surgical management, the size of the stone, resultant bowel wall edema, inflammation (Fig. 9b and c), and ischemia, can assess the biliary system, and identify other causes of pain [2, 68]. The radiologist should search for additional stones within the gallbladder lumen as well as dilated small bowel proximal to the location of the obstructing ectopic gallstone in order to identify and prevent recurrence of gallstone ileus. Contrast-enhanced CT has a sensitivity of 90–93%, specificity of 100%, and accuracy of 99% [2, 78] for gallstone ileus. Gallstones causing large bowel obstruction are a less frequent phenomenon and imaging demonstrates large bowel dilatation, with small bowel caliber depending on the competency of the ileocecal valve (Fig. 10a–c).
Rigler’s triad: small bowel obstruction. CT topogram (a) shows gaseous distention of small bowel loops (*). Axial CECT image (b) demonstrates a thick-walled contracted gallbladder containing air (arrow) and fistulous tract connecting gallbladder lumen with duodenal lumen representing cholecystoduodenal fistula. Coronal CECT images (c and d) show dilated small bowel loops (* in c), pneumobilia (arrowhead in c) and gallstone (arrow in d) obstructing the ileal loops. Rigler’s triad includes gas in the biliary tract, small bowel obstruction, and ectopic gallstone
Gallstone coleus. CT topogram (a) shows significantly dilated and gas distended large bowel (*) representing large bowel obstruction. Coronal CECT image (b) shows dilated large bowel loops in the periphery of the abdominal cavity and contracted gallbladder with wall thickening and containing a gallstone (arrow). Sagittal CECT image (c) shows impacted gallstone in the sigmoid colon (arrow) with decompressed distal segment of large bowel (arrowheads)
There are many therapeutic options for treatment of bowel obstruction due to impacted ectopic gallstones. Shock wave lithotripsy, endoscopic EHL (electrohydraulic lithotripsy), and endoscopic mechanical lithotripsy have been successful in treating the impacted gallstone but may be limited by availability and ability to reach the stone endoscopically; enterolithotomy remains the most commonly performed operative method with ongoing debate if the biliary repair should be performed simultaneously or in a delayed manner [79]. Spontaneous fistula closure is not uncommon eliminating the need for fistula closure and recurrence of gallstone ileus after enterolithotomy is around 5 to 9% [79].
Conclusion
Gallstones cause various complications in addition to acute cholecystitis, ranging from biliary colic to infectious processes and bowel obstruction. Given emergency radiologists have an important role in providing a timely diagnosis, they should be familiar with the multimodality imaging findings and modality limitations in diagnosing complications of gallstones beyond the cystic duct to facilitate appropriate treatment and management. While US is generally considered first-line imaging for RUQ pain and the evaluation of gallstones and acute cholecystitis, it is limited in ability to detect common duct stones. MRCP and ERCP have been shown to have higher sensitivity for detection of CBD stones and biliary-enteric fistulae, with ERCP having the advantage of also being therapeutic. While CT is not as sensitive for the detection of gallstones, it is often the first imaging performed in the ED setting and can diagnose or suggest CBD stones due to biliary ductal dilatation and can demonstrate acute interstitial edematous pancreatitis and bowel obstruction from ectopic gallstone. Mirizzi syndrome remains a difficult diagnosis to make preoperatively and requires extra vigilance by the radiologist to suggest the diagnosis or recommend further imaging.
Data availability
Not applicable.
Code availability
Not applicable.
References
Zimmer V, Lammert F (2015) Acute bacterial cholangitis. Viszeralmedizin 31(3):166–172. https://doi.org/10.1159/000430965
Chang L et al (2018) Clinical and radiological diagnosis of gallstone ileus: a mini review. Emerg Radiol 25(2):189–196. https://doi.org/10.1007/s10140-017-1568-5
Kratzer W, Mason RA, Kächele V (1999) Prevalence of gallstones in sonographic surveys worldwide. J Clin Ultrasound 27(1):1–7
Sakorafas GH, Milingos D, Peros G (2007) Asymptomatic cholelithiasis: is cholecystectomy really needed? A critical reappraisal 15 years after the introduction of laparoscopic cholecystectomy. Dig Dis Sci 52(5):1313–1325
Gracie WA, Ransohoff DF (1982) The natural history of silent gallstones: the innocent gallstone is not a myth. N Engl J Med 307(13):798–800
Ruhl CE, Everhart JE (2011) Gallstone disease is associated with increased mortality in the United States. Gastroenterology 140(2):508–516
McIntosh DM, Penney HF (1980) Gray-scale ultrasonography as a screening procedure in the detection of gallbladder disease. Radiology 136(3):725–727. https://doi.org/10.1148/radiology.136.3.7403554
Bortoff GA et al (2000) Gallbladder stones: imaging and intervention. Radiographics 20(3):751–766. https://doi.org/10.1148/radiographics.20.3.g00ma16751
MacDonald FR, Cooperberg PL, Cohen MM (1981) The WES triad — a specific sonographic sign of gallstones in the contracted gallbladder. Gastrointest Radiol 6(1):39–41. https://doi.org/10.1007/BF01890219
Ratanaprasatporn L et al (2018) Multimodality imaging, including dual-energy CT, in the evaluation of gallbladder disease. Radiographics 38(1):75–89. https://doi.org/10.1148/rg.2018170076
Patel NB, Oto A, Thomas S (2013) Multidetector CT of emergent biliary pathologic conditions. Radiographics 33(7):1867–1888. https://doi.org/10.1148/rg.337125038
Gore RM et al (2010) Gallbladder imaging. Gastroenterol Clin North Am 39(2):265–287. https://doi.org/10.1016/j.gtc.2010.02.009
Uyeda JW, Richardson IJ, Sodickson AD (2017) Making the invisible visible: improving conspicuity of noncalcified gallstones using dual-energy CT. Abdom Radiol (NY) 42(12):2933–2939. https://doi.org/10.1007/s00261-017-1229-x
Yang CB et al (2017) Clinical application of dual-energy spectral computed tomography in detecting cholesterol gallstones from surrounding bile. Acad Radiol 24(4):478–482. https://doi.org/10.1016/j.acra.2016.10.006
Bae JS et al. (2019) Utilization of virtual non-contrast images derived from dual-energy CT in evaluation of biliary stone disease: virtual non-contrast image can replace true non-contrast image regarding biliary stone detection. Eur J Radiol 116: 34–40. https://www.sciencedirect.com/science/article/pii/S0720048X19301408. Accessed 2 Nov 2021
Murphy MC et al (2020) Gallstones top to toe: what the radiologist needs to know. Insights Imaging 11(1):13. https://doi.org/10.1186/s13244-019-0825-4
Mendler MH et al (1998) Value of MR cholangiography in the diagnosis of obstructive diseases of the biliary tree: a study of 58 cases. Am J Gastroenterol 93(12):2482–2490
Gutt C, Schläfer S, Lammert F (2020) The treatment of gallstone disease. Dtsch Arztebl Int 117(9):148–158
Tazuma S (2006) Epidemiology, pathogenesis, and classification of biliary stones (common bile duct and intrahepatic). Best Pract Res Clin Gastroenterol 20(6):1075–1083. https://doi.org/10.1016/j.bpg.2006.05.009
Perveze Z, Krishnamurthy C, Duckworth CW (2008) The incidence of choledocholithiasis in a community setting. Gastrointest Endosc 67(5):AB297. https://doi.org/10.1016/j.gie.2008.03.863
Dasari BV et al (2013) Surgical versus endoscopic treatment of bile duct stones. Cochrane Database Syst Rev 12:CD003327. https://doi.org/10.1002/14651858.cd003327.pub4
Molvar C, Glaenzer B (2016) Choledocholithiasis: evaluation, treatment, and outcomes. Semin Intervent Radiol 33(4):268–276
Condon FJ (2019) Choledocholithiasis and cholangitis: incidence, initial management, and surgical management. In: Lim R (ed) Multidisciplinary approaches to common surgical problems. Springer International Publishing, Cham, pp 161–166
Abraham S et al (2014) Surgical and nonsurgical management of gallstones. Am Fam Physician 89(10):795–802
Perret RS, Sloop GD, Borne JA (2000) Common bile duct measurements in an elderly population. J Ultrasound Med 19(11):727–730. https://doi.org/10.7863/jum.2000.19.11.727
Einstein DM et al (1984) The insensitivity of sonography in the detection of choledocholithiasis. Am J Roentgenol 142(4):725–728. https://doi.org/10.2214/ajr.142.4.725
Veronica B et al (2019) Imaging of biliary colic and cholecystitis. In: Cova MA, Stacul F (eds) Pain imaging: a clinical-radiological approach to pain diagnosis. Springer International Publishing, Cham, pp 229–245
Wertz JR et al (2018) Comparing the diagnostic accuracy of ultrasound and CT in evaluating acute cholecystitis. AJR Am J Roentgenol 211(2):W92-w97
Anderson SW et al (2006) Accuracy of MDCT in the diagnosis of choledocholithiasis. Am J Roentgenol 187(1):174–180. https://doi.org/10.2214/AJR.05.0459
Verma D et al (2006) EUS vs MRCP for detection of choledocholithiasis. Gastrointest Endosc 64(2):248–254
Makmun D, Fauzi A, Shatri H (2017) Sensitivity and specificity of magnetic resonance cholangiopancreatography versus endoscopic ultrasonography against endoscopic retrograde cholangiopancreatography in diagnosing choledocholithiasis: the Indonesian experience. Clin Endosc 50(5):486–490
Gurusamy KS et al (2015) Endoscopic retrograde cholangiopancreatography versus intraoperative cholangiography for diagnosis of common bile duct stones. Cochrane Database Syst Rev 2015(2):Cd010339
Kint JF et al (2015) Percutaneous treatment of common bile duct stones: results and complications in 110 consecutive patients. Dig Surg 32(1):9–15
Jung GS et al (2019) Percutaneous transcholecystic removal of common bile duct stones: case series in 114 patients. Radiology 290(1):238–243
Pereira J et al (2017) Accuracy of ultrasound in the diagnosis of acute cholecystitis with coexistent acute pancreatitis. Eur J Trauma Emerg Surg 43(1):79–83. https://doi.org/10.1007/s00068-015-0619-4
Koo BC, Chinogureyi A, Shaw AS (2010) Imaging acute pancreatitis. Br J Radiol 83(986):104–112. https://doi.org/10.1259/bjr/13359269
Surlin V, Saftoiu A, Dumitrescu D (2014) Imaging tests for accurate diagnosis of acute biliary pancreatitis. World J Gastroenterol 20(44):16544–16549. https://doi.org/10.3748/wjg.v20.i44.16544
Neoptolemos JP et al (2005) The urgent diagnosis of gallstones in acute pancreatitis: a prospective study of three methods. Br J Surg 71(3):230–233. https://doi.org/10.1002/bjs.1800710324
Shah AP, Mourad MM, Bramhall SR (2018) Acute pancreatitis: current perspectives on diagnosis and management. J Inflamm Res 11:77–85. https://doi.org/10.2147/jir.s135751
Baron RL et al (1983) Computed tomographic features of biliary obstruction. AJR Am J Roentgenol 140(6):1173–1178
Vege SS et al (2018) Initial medical treatment of acute pancreatitis: American Gastroenterological Association Institute technical review. Gastroenterology 154(4):1103–1139. https://doi.org/10.1053/j.gastro.2018.01.031
O’Connor OJ, McWilliams S, Maher MM (2011) Imaging of acute pancreatitis. AJR Am J Roentgenol 197(2):W221–W225. https://doi.org/10.2214/ajr.10.4338
Alexakis N, Neoptolemos JP (2005) Algorithm for the diagnosis and treatment of acute biliary pancreatitis. Scand J Surg 94(2):124–129. https://doi.org/10.1177/145749690509400208
Perera M et al (2013) A case of concomitant perforated acute cholecystitis and pancreatitis. Case Rep Surg 2013:263046. https://doi.org/10.1155/2013/263046
Friedman GD (1993) Natural history of asymptomatic and symptomatic gallstones. Am J Surg 165(4):399–404
Catalano OA et al (2009) Biliary infections: spectrum of imaging findings and management. Radiographics 29(7):2059–2080. https://doi.org/10.1148/rg.297095051
Reynolds BM, Dargan EL (1959) Acute obstructive cholangitis; a distinct clinical syndrome. Ann Surg 150(2):299–303. https://doi.org/10.1097/00000658-195908000-00013
Bader TR et al (2001) MR imaging findings of infectious cholangitis. Magn Reson Imaging 19(6):781–788. https://doi.org/10.1016/s0730-725x(01)00401-5
Ahmed M (2018) Acute cholangitis - an update. World J Gastrointest Pathophysiol 9(1):1–7. https://doi.org/10.4291/wjgp.v9.i1.1
Lee JG (2009) Diagnosis and management of acute cholangitis. Nat Rev Gastroenterol Hepatol 6(9):533–541. https://doi.org/10.1038/nrgastro.2009.126
Lai EC, Lau WY (2006) Mirizzi syndrome: history, present and future development. ANZ J Surg 76(4):251–257. https://doi.org/10.1111/j.1445-2197.2006.03690.x
Beltran MA (2012) Mirizzi syndrome: history, current knowledge and proposal of a simplified classification. World J Gastroenterol 18(34):4639–4650. https://doi.org/10.3748/wjg.v18.i34.4639
Beltran MA, Csendes A (2005) Mirizzi syndrome and gallstone ileus: an unusual presentation of gallstone disease. J Gastrointest Surg 9(5):686–689. https://doi.org/10.1016/j.gassur.2004.09.058
Beltran MA, Csendes A, Cruces KS (2008) The relationship of Mirizzi syndrome and cholecystoenteric fistula: validation of a modified classification. World J Surg 32(10):2237–2243. https://doi.org/10.1007/s00268-008-9660-3
Csendes A et al (1989) Mirizzi syndrome and cholecystobiliary fistula: a unifying classification. Br J Surg 76(11):1139–1143. https://doi.org/10.1002/bjs.1800761110
Abou-Saif A, Al-Kawas FH (2002) Complications of gallstone disease: Mirizzi syndrome, cholecystocholedochal fistula, and gallstone ileus. Am J Gastroenterol 97(2):249–254. https://doi.org/10.1111/j.1572-0241.2002.05451.x
Lubbers EJ (1983) Mirizzi syndrome. World J Surg 7(6):780–785. https://doi.org/10.1007/bf01655221
Montefusco P, Spier N, Geiss AC (1983) Another facet of Mirizzi’s syndrome. Arch Surg 118(10):1221–1223. https://doi.org/10.1001/archsurg.1983.01390100083021
Dietrich KF (1963) Stenosis of the hepatic duct in lithiasis of the gallbladder neck and cystic duct (Mirizzi syndrome). Bruns Beitr Klin Chir 206:9–22
Redaelli CA et al (1997) High coincidence of Mirizzi syndrome and gallbladder carcinoma. Surgery 121(1):58–63
Beltrán MA (2012) Mirizzi syndrome: history, current knowledge and proposal of a simplified classification. World J Gastroenterol 18(34):4639–4650
Solis-Caxaj CA (2009) Mirizzi syndrome: diagnosis, treatment and a plea for a simplified classification. World J Surg 33(8):1783–1784. https://doi.org/10.1007/s00268-009-9929-1
Shirah BH, Shirah HA, Albeladi KB (2017) Mirizzi syndrome: necessity for safe approach in dealing with diagnostic and treatment challenges. Ann Hepatobiliary Pancreat Surg 21(3):122–130. https://doi.org/10.14701/ahbps.2017.21.3.122
Tan KY et al (2004) Mirizzi syndrome: noteworthy aspects of a retrospective study in one centre. ANZ J Surg 74(10):833–837. https://doi.org/10.1111/j.1445-1433.2004.03184.x
Choi BW et al (2000) Radiologic findings of Mirizzi syndrome with emphasis on MRI. Yonsei Med J 41(1):144–146. https://doi.org/10.3349/ymj.2000.41.1.144
Chen H et al (2018) Current trends in the management of Mirizzi Syndrome: a review of literature. Medicine (Baltimore) 97(4):e9691. https://doi.org/10.1097/md.0000000000009691
Balent E, Plackett TP, Lin-Hurtubise K (2012) Cholecystocolonic fistula. Hawaii J Med Public Health 71(6):155–157
Liang X et al (2015) Comparative analysis of MDCT and MRI in diagnosing chronic gallstone perforation and ileus. Eur J Radiol 84(10):1835–1842. https://doi.org/10.1016/j.ejrad.2015.06.009
Oskam J, Heitbrink M, EeftinckSchattenkerk M (1993) Intermittent gallstone ileus following endoscopic biliary sphincterotomy. A case report. Acta Chir Belg 93(2):43–5
Foss H, Summers J (1942) Intestinal obstruction from gallstones. Ann Surg 115:721
Masannat Y, Masannat Y, Shatnawei A (2006) Gallstone ileus: a review. Mt Sinai J Med 73(8):1132–1134
Halabi WJ et al (2014) Surgery for gallstone ileus: a nationwide comparison of trends and outcomes. Ann Surg 259(2):329–335. https://doi.org/10.1097/sla.0b013e31827eefed
Alemi F, Seiser N, Ayloo S (2019) Gallstone disease: cholecystitis, Mirizzi syndrome, Bouveret syndrome, gallstone ileus. Surg Clin North Am 99(2):231–244. https://doi.org/10.1016/j.suc.2018.12.006
Lassandro F et al (2005) Role of helical CT in diagnosis of gallstone ileus and related conditions. AJR Am J Roentgenol 185(5):1159–1165. https://doi.org/10.2214/ajr.04.1371
Prasad RM, Weimer KM, Baskara A (2017) Gallstone ileus presenting as intussusception: a case report. Int J Surg Case Rep 30:37–39. https://doi.org/10.1016/j.ijscr.2016.11.036
Ayantunde AA, Agrawal A (2007) Gallstone ileus: diagnosis and management. World J Surg 31(6):1292–1297. https://doi.org/10.1007/s00268-007-9011-9
Beuran M, Ivanov I, Venter MD (2010) Gallstone ileus–clinical and therapeutic aspects. J Med Life 3(4):365–371
Yu CY et al (2005) Value of CT in the diagnosis and management of gallstone ileus. World J Gastroenterol 11(14):2142–2147. https://doi.org/10.3748/wjg.v11.i14.2142
Jakubauskas M, et al. (2019) Gallstone ileus: management and clinical outcomes. Medicina (Kaunas) 55(9). https://doi.org/10.3390/medicina55090598
Author information
Authors and Affiliations
Contributions
Dr. Kiran Maddu, Dr. Carrie Hoff, and Dr. Arie Neymotin contributed to the study conception. All authors contributed to the design. Material preparation, including images, was performed by Dr. Maddu, Dr. Hoff, and Dr. Neymotin. The first draft of the manuscript was written by Andrew Tran, Karunesh Polireddy, Dr. Kiran Maddu, Dr. Carrie Hoff, and Dr. Arie Neymotin. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Alterations to figures (to anonymize any patient identifiers) do not distort meaning.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tran, A., Hoff, C., Polireddy, K. et al. Beyond acute cholecystitis—gallstone-related complications and what the emergency radiologist should know. Emerg Radiol 29, 173–186 (2022). https://doi.org/10.1007/s10140-021-01999-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-021-01999-y