Abstract
Purpose
To determine the diagnostic accuracy and time savings of an abbreviated magnetic resonance cholangiopancreatography (A-MRCP) protocol for detecting choledocholithiasis in patients visiting the emergency department (ED) for suspected biliary obstruction.
Methods and materials
This retrospective study evaluated adult patients (ages 18+ years) visiting an academic Level 1 trauma center between January 1, 2016, and December 31, 2017, who were imaged with MRCP for suspected biliary obstruction. Patients were scanned with either a four-sequence A-MRCP protocol or a conventional eight-sequence MRCP (C-MRCP) protocol. Image acquisition and MRI room time were compared. The radiology report was used to determine whether a study was limited by motion or prematurely aborted, as well as for the presence of pertinent biliary findings. Diagnostic accuracy of A-MRCP studies were compared with any available endoscopic retrograde cholangiopancreatography (ERCP) report within 30 days.
Results
One hundred sixteen patients met inclusion criteria; 85 were scanned with the A-MRCP protocol (45.9% male, mean 57.4 years) and 31 with the C-MRCP protocol (38.7% male, mean 58.3 years). Mean image acquisition time and MRI room time for the A-MRCP protocol were significantly lower compared to those for the C-MRCP protocol (16 and 34 min vs. 42 and 61 min, both p < 0.0001). Choledocholithiasis was seen in 23.5% of A-MRCP cases and 19.4% of C-MRCP cases. Non-biliary findings were common in both cohorts, comprising 56.5% of A-MRCP cases and 41.9% of C-MRCP cases. 44.7% of A-MRCP patients received subsequent (diagnostic or therapeutic) ERCP (mean follow-up time 3 days), in which A-MRCP accurately identified choledocholithiasis in 86.8% of cases, with sensitivity of 85%, specificity of 88.9%, positive predictive value (PPV) of 89.5%, and negative predictive value (NPV) of 84.2%. In comparison, 38.7% of C-MRCP patients underwent ERCP (mean follow-up of 2.3 days) with an accuracy of 91.7%, sensitivity of 80%, specificity of 100%, PPV of 100%, and NPV of 87.5%. Only 4.7% of A-MRCP exams demonstrated motion artifact vs. 12.9% of C-MRCP exams. One study was prematurely aborted due to patient discomfort in the A-MRCP cohort while no studies were terminated in the C-MRCP cohort.
Conclusion
An abbreviated MRCP protocol to evaluate for choledocholithiasis provides significant time savings and reduced motion artifact over the conventional MRCP protocol while providing similar diagnostic accuracy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Gallstone and gallstone-related disease affects 10–15% of Americans or up to 20 million people, with associated health care costs reaching $6.2 billion [1]. Between 5 and 10% of patients presenting with symptomatic cholelithiasis will also have concomitant choledocholithiasis [1]. Delayed diagnosis of a common bile duct stone can lead to recurrent symptoms, pancreatitis, or even cholangitis. Transabdominal ultrasound is the initial imaging modality in the workup of biliary colic and right upper quadrant pain due to its wide availability and high sensitivity for detecting gallbladder stones [2]. However, the ability to detect common bile duct stones with ultrasound is limited, with sensitivities ranging between 22 and 55% [3].
Other tests with better diagnostic accuracy for evaluating choledocholithiasis include endoscopic ultrasound (EUS) and endoscopic retrograde cholangiopancreatography (ERCP), both with sensitivities ranging from 93 to 97% and specificities of 77–96% [4]. The additional benefit of ERCP is that it also allows for therapeutic treatment. Unfortunately, both these procedures require sedation and may not be readily available depending on local resources and personnel. In addition, ERCP has associated risks including pancreatitis (1.3–6.7%), infection (0.6–5.0%), hemorrhage (0.3–2.0%), and perforation (0.1–1.1%) [1, 4].
Magnetic resonance cholangiopancreatography (MRCP) is an alternative non-invasive imaging modality which has a comparable diagnostic profile to EUS and ERCP with sensitivities ranging from 85 to 92% and specificities of 93–97% [1, 5,6,7]. MRCP utilizes a heavily T2-weighted sequence to increase the relative contrast of the biliary and pancreatic ducts. The American Society of Gastrointestinal Endoscopy (ASGE) recommends that MRCP be performed on patients with intermediate probability (10–50%) for choledocholithiasis in the setting of symptomatic cholelithiasis [1, 8]. A recent study of patients awaiting cholecystectomy found that 6.7% had choledocholithiasis with the majority having normal caliber common bile ducts [9]. The authors therefore advocated for routine MRCP in such patients. The advantage of an abbreviated MRCP protocol performed in the acute setting can help reduce the time delay to surgery.
MRCP has become the preferred diagnostic imaging modality for the workup of biliary obstruction. MRCP performed in the emergency department (ED) has the potential to identify the cause of biliary obstruction and allow for faster triaging of patients who may require treatment with ERCP. However, limitations of MRCP include patient intolerance due to long scan times and decreased access in the acute setting. Patients presenting to the ED are often quite ill and shorter MRI scan times can help to reduce patient discomfort and optimize diagnostic image quality [8]. Therefore, the purpose of this study was to determine the diagnostic accuracy and time savings of an abbreviated MRCP (A-MRCP) protocol in diagnosing choledocholithiasis in ED patients with suspected biliary obstruction.
Method and materials
Patient selection
This Health Insurance Portability and Accountability Act-compliant retrospective study received Institutional Review Board approval with a waiver for informed patient consent. The radiology databases were queried for patients ages 18+ years visiting a quaternary care, urban academic Level 1 trauma center between January 1, 2016, and December 31, 2017, and who received an MRCP exam while a patient in the ED.
MRI imaging technique
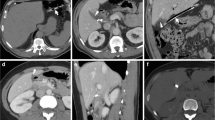
All MRCP studies were performed on a single 1.5-T MRI scanner (General Electric, Chicago, IL) located within the ED. This study included patients who were scanned with either a non-contrast abbreviated MRCP scan (A-MRCP), consisting of a localizer plus four sequences, or a conventional contrast-enhanced MRCP (C-MRCP) protocol, consisting of a localizer plus eight sequences (Table 1). The A-MRCP protocol consists of a coronal fast spin echo sequence, an axial gradient echo with fat saturation, and 2D/3D MRCP sequences (Figs. 1 & 2). The C-MRCP protocol comprises the aforementioned sequences, with the addition of post-gadolinium and diffusion-weighted sequences. Determination of whether a patient received the A-MRCP or C-MRCP protocol was at the discretion of the radiologist at the time the exam who ordered based on the clinical indication.
Data sources and collection
Data on image acquisition time, MRI room time, and patient demographics including age and gender were obtained from the radiology databases. Image acquisition time was determined from the beginning of the first localizer image to the last image of the final sequence based on the timestamps labeled on the study images. For the A-MRCP cohort, any recent prior imaging studies were documented, specifically ultrasound, CT, or both.
Whether a MRCP exam was prematurely aborted or limited by patient motion artifact was determined from the radiology report on PACS. All A-MRCP studies were interpreted by board-certified ED radiologists with background fellowship training in neuroradiology, MSK, and abdomen. Radiological findings for A-MRCP exams were also determined based on the radiology report, including findings of choledocholithiasis, biliary duct dilatation, and cholecystitis. Other non-biliary findings were documented based on the radiology report. Follow-up MRCP examinations up to 90 days were documented in the A-MRCP group based on follow-up studies in PACS.
Outcome measures
The primary outcome of this study is to determine the accuracy of the A-MRCP protocol in relation to ERCP, considered the gold standard in this study. Accuracy was assessed by sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) calculations. Time savings in image acquisition and MRI room time of the A-MRCP protocol versus C-MRCP were another primary outcome. The secondary outcome of the study was to determine the frequency of suboptimal and prema turely aborted exams in both comparison groups. Another secondary outcome was to determine the frequency of non-biliary imaging findings on the A-MRCP exam.
Statistical analysis
Patient demographics were summarized with descriptive statistics and compared between the two protocols. Comparison of image acquisition and MRI room times between the two protocols were evaluated using the Mann-Whitney test due to the non-normality of the residual distribution. A p value of < 0.05 was determined to be statistically significant. Sensitivity, PPV, and NPV were calculated for patients who received follow-up ERCP.
Results
Patient cohort
A total of 116 patients met study inclusion criteria. Of these, 85 patients were imaged with the A-MRCP protocol (45.9% male, mean age 57.4 years) and 31 (38.7% male, mean age 58.3 years) with the C-MRCP protocol (Table 2). Of the A-MRCP group, recent prior imaging with ultrasound was noted in 46 patients (54.1%), CT in 15 patients (17.6%), and a combination of US/CT in 10 patients (11.8%). No prior imaging was obtained in 14 cases (16.5%).
Coronal single-shot fast spin echo (a) and 3D MRCP (b) sequences from the non-contrast abbreviated (A-MRCP) protocol demonstrate significant intra- and extrahepatic biliary duct dilatation with a filling defect seen in the distal common bile duct, compatible with choledocholithiasis. Correlation with ERCP is shown in c
Accuracy of the A-MRCP protocol
Choledocholithiasis was diagnosed in 20 A-MRCP cases (23.5%) and 6 C-MRCP cases (19.4%). Pertinent biliary findings from all MRCP exams are summarized in Table 3. Of the A-MRCP patients, 38 (44.7%) received a subsequent ERCP with a mean follow-up time of 3 days vs. 12 (38.7%) of the C-MRCP patients with a mean follow-up of 2.3 days. Using ERCP as the gold standard, the A-MRCP protocol correctly identified choledocholithiasis in 86.8% of cases with 17 true positive and 17 true negative cases, with 1 false positive and 3 false negative cases. This corresponds to a sensitivity of 85%, specificity of 88.9%, PPV of 89.5%, and NPV of 84.2%. Based on C-MRCP cases that went to ERCP, there were 4 true positive cases, 7 true negative cases, and 1 false negative case, yielding a diagnostic accuracy of 91.7%, sensitivity of 80%, specificity of 100%, PPV of 100%, NPV of 87.5%.
Time savings
The image acquisition time for the A-MRCP protocol was significantly shorter (mean 16 min, range 7–42), compared to that for the C-MRCP protocol (mean 42 min, range 29–65) (p < 0.0001), with a mean time savings of 26 min. The mean MRI room time for the A-MRCP protocol was 34 min, significantly lower than that for the C-MRCP protocol of 61 min (p < 0.0001).
Aborted and suboptimal exams
Of the 85 A-MRCP exams, only 1 study was prematurely aborted due to patient discomfort (1.2%) and 4 scans were limited by motion artifact (4.7%). Of the 31 C-MRCP scans, no studies were prematurely aborted and 4 were limited by motion artifact (12.9%).
Discussion
Although MRCP is an ideal imaging modality for the workup of biliary obstruction, few studies have evaluated its effectiveness in the ED setting [10]. Specifically, there is a lack of reported studies evaluating the diagnostic utility and time savings of an abbreviated MRCP protocol in the acute care setting. There are several conclusions that can be drawn from the results of our study.
The A-MRCP protocol demonstrated similar diagnostic accuracy compared to ERCP for the detection of common bile duct stones in our study. In addition, there were significant time savings of the A-MRCP protocol over the conventional contrast-enhanced C-MRCP protocol, with 27 minutes saved on average, or 44% faster. This is likely attributable to the lack of sequences and lack of gadolinium contrast which would be more suitable for the workup of liver or pancreatic lesions rather than choledocholithiasis. In a previous study examining the performance of a non-contrast MRCP protocol vs. contrast-enhanced MRCP protocol for evaluating biliary obstruction in the inpatient setting, both protocols resulted in high accuracy for detecting choledocholithiasis without significant differences in sensitivity or specificity [7]. An abbreviated MRCP protocol to evaluate for suspected choledocholithiasis can theoretically aid in faster triaging and management for patients in the ED setting. In addition, MRCP avoids the unnecessary invasiveness-related complications and cost of ERCP and is ideal in patients who are not optimal candidates for such a procedure [11].
Imaging ED patients involves additional factors which can contribute to suboptimal image quality, including patient motion artifact due to pain related to their acute clinical presentation, discomfort, or anxiety [12]. From an ED workflow perspective, abbreviated MRI protocols may allow for more patients to be scanned with the MRI scanner, helping to maximize utilization of this limited resource. Potential downstream benefits include quicker time to disposition or management with possible shortening of ED length of stay, or expedited referral of patients to specialty services for consideration for ERCP, which are areas for future research. Furthermore, the current American College of Radiology Appropriateness Criteria® could be further optimized by accounting for the clinical setting when making their recommendation.
Non-biliary findings were commonly present in all MRCP studies. In the literature, although MRCP is diagnostically comparable to ERCP for detecting choledocholithiasis, accuracy for evaluating for malignancy is somewhat lower, with sensitivities ranging from 81 to 86% and specificities ranging from 92 to 100% [11]. Our results suggest that the role of an abbreviated MRCP exam in the ED setting is to determine whether an ERCP is indicated. A non-emergent contrast-enhanced MRI could be subsequently performed for the non-emergent evaluation of suspicious lesions or incidental findings.
Of note, a higher proportion of C-MRCP scans were limited by patient motion, which would be expected for studies with longer acquisition times. Efforts should be made to optimize MRI protocols to collect sufficient diagnostic information to answer the specific clinical question in the particular clinical setting. Reducing MRI scan time can reduce patient discomfort and decrease the probability for suboptimal or prematurely aborted exams.
There are several limitations of this study including the retrospective single-center study design with a small sample size of the comparison C-MRCP cohort. Due to the retrospective design, assignment of the MRCP protocol was not randomized, which introduced bias when analyzing the two groups, especially when availability of prior ultrasound or CT results may influence which protocol was used. There is a potential for variable clinical expertise of ED radiologists interpreting MRCP exams affecting the diagnostic accuracy, but our study demonstrated similar accuracy compared to the reported literature. The primary goal of the study was to assess the diagnostic accuracy of the A-MRCP compared with the ERCP, and look at time savings compared to the C-MRCP protocol. Additionally, MRCP exams were interpreted by ED attending radiologists with varied background of fellowship training, not necessarily specific for the interpretation of MRI abdomen exams. Despite this, the diagnostic accuracy of the A-MRCP exams remained relatively high, which may be attributed to the reduced number of sequences needed to be interpreted, as well as focus on answering the specific clinical question of biliary obstruction. In addition, radiological findings from the MRCP studies were extracted from the radiology report, which was done to reflect clinical practice.
Conclusion
An A-MRCP protocol can identify choledocholithiasis in the ED setting with reasonable accuracy when compared to ERCP with significant time savings compared to C-MRCP protocols. From an ED workflow perspective, abbreviated MRI protocols may allow for expeditious triaging and referral of patients to specialty services and increase the availability of MRI for use with additional patients. Non-emergent contrast-enhanced MRCP may be performed for the workup of a small number of incidental or incompletely characterized findings discovered on an A-MRCP scan.
Shorter MRI protocols may help to reduce the number of aborted and suboptimal scans by reducing patient discomfort that contributes to motion artifact. Efforts should be made to optimize MRI protocols to assist in the disposition of patients by answering the specific clinical question when scanning patients in the ED setting.
References
ASGE Standards of Practice Committee (2010 Jan) Maple JT, Ben-Menachem T, Anderson MA, Appalaneni V, Banerjee S, et al. The role of endoscopy in the evaluation of suspected choledocholithiasis. Gastrointest Endosc 71(1):1–9
Yarmish GM, Smith MP, Rosen MP, Baker ME, Blake MA, Cash BD, Hindman NM, Kamel IR, Kaur H, Nelson RC, Piorkowski RJ (2014 Mar 1) ACR appropriateness criteria right upper quadrant pain. J Am Coll Radiol 11(3):316–322
Cronan JJ (1986 Oct) US diagnosis of choledocholithiasis: a reappraisal. Radiology. 161(1):133–134
Kang SK, Hoffman D, Ferket B, Kim MI, Braithwaite RS (2017 Aug) Risk-stratified versus non-risk-stratified diagnostic testing for management of suspected acute biliary obstruction: comparative effectiveness, costs, and the role of MR cholangiopancreatography. Radiology. 284(2):468–481
Verma D, Kapadia A, Eisen GM, Adler DG (2006 Aug 1) EUS vs MRCP for detection of choledocholithiasis. Gastrointest Endosc 64(2):248–254
Makmun D, Fauzi A, Shatri H (2017 Sep) Sensitivity and specificity of magnetic resonance cholangiopancreatography versus endoscopic ultrasonography against endoscopic retrograde cholangiopancreatography in diagnosing choledocholithiasis: the Indonesian experience. Clinical endoscopy 50(5):486–490
Kang SK, Heacock L, Doshi AM, Ream JR, Sun J, Babb JS (2017 Jun) Comparative performance of non-contrast MRI with HASTE versus contrast-enhanced MRI/3D-MRCP for possible choledocholithiasis in hospitalized patients. Abdominal radiology (New York) 42(6):1650–1658
Havsteen I, Ohlhues A, Madsen KH, Nybing JD, Christensen H, Christensen A (2017 May 30) Are movement artifacts in magnetic resonance imaging a real problem?—a narrative review. Front Neurol 8:232
Virzì V, Ognibene NM, Sciortino AS, Culmone G, Virzì G (2018 Oct 1) Routine MRCP in the management of patients with gallbladder stones awaiting cholecystectomy: a single-centre experience. Insights into imaging 9(5):653–659
Mills AM, Raja AS, Marin JR (2015 May) Optimizing diagnostic imaging in the emergency department. Acad Emerg Med 22(5):625–631
Kaltenthaler E, Vergel YB, Chilcott J, Thomas S, Blakeborough T, Walters SJ, Bouchier H. A systematic review and economic evaluation of magnetic resonance cholangiopancreatography compared with diagnostic endoscopic retrograde cholangiopancreatography, https://doi.org/10.1007/s41669-016-0001-4
Zaitsev M, Maclaren J, Herbst M (2015 Oct) Motion artifacts in MRI: a complex problem with many partial solutions. J Magn Reson Imaging 42(4):887–901
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tso, D.K., Almeida, R.R., Prabhakar, A.M. et al. Accuracy and timeliness of an abbreviated emergency department MRCP protocol for choledocholithiasis. Emerg Radiol 26, 427–432 (2019). https://doi.org/10.1007/s10140-019-01689-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-019-01689-w