Abstract
Large-bowel obstruction (LBO) is a relatively common abdominal emergency. The CT exam has become the most important imaging modality for the diagnosis of LBO, following abdominal ultrasound and plain radiography. The recent multi-detector CT (MD-CT) is able to clarify the etiology of LBO and to help in deciding how to treat LBO. Therefore, it is important for the radiologists to become familiar with the imaging findings of LBO, including plain radiograph and CT, due to various causes. In this article, we have shown the characteristics of the radiological findings including plain radiograph, barium study, and CT as well as their correlations with pathologic findings of LBO. The etiology of LBO is usually divided into neoplastic diseases and nonneoplastic diseases. However, the most common cause is the neoplastic etiology. Now, we can afford the critical information concerning the level of obstruction, its cause, the viability of the involved bowel loops, and a decision-making regarding the therapy for patients with LBO, using MD-CT high technology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Large-bowel obstruction (LBO) is a critical clinical condition, which may present as an emergency that requires early and accurate diagnosis for a prompt treatment. The first-line imaging modality for acute abdomen includes abdominal ultrasonography and plain radiograph. Under these baseline exams suspected for large-bowel obstruction, the problem-solving role of CT in the diagnosis and assessment of LBO has expanded further due to feasibility, short examination time, and a large volume of information. Nowadays, CT can afford the critical information: whether there is a mechanical obstruction or not, where the level of obstruction is, whether LBO is associated with bowel ischemia, and finally, the recommended management for LBO [1, 2]. Moreover, the recent introduction of multi-detector CT (MD-CT) technology with intravenous contrast medium dynamic enhancement with rapid bolus injection and early (arterial phase) and delayed (portal venous phase) scanning method has made it possible to diagnose the site of obstruction, the etiology and the extent of the lesion, and also the associated bowel ischemia more easily than when only single helical CT scanning was available.
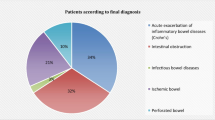
As the cause of LBO, colorectal cancer, diverticulitis, and volvulus account for approximately 80–85 % of the cases of LBO [2]. We recently published the review article entitled “Radiological diagnosis of large-bowel obstruction: nonneoplastic etiology” [3]. In this article, we present the radiological findings of LBO of neoplastic etiology, including plain radiography and CT, with special emphasis on CT findings, as it is important for radiologists to become familiar with the CT findings of LBO.
The following contents are presented:
-
1.
Colorectal carcinoma
-
2.
Obstructive colitis
-
3.
Adult intestinal intussusception
-
4.
Colonic obstruction caused by external neoplastic causes
Colorectal carcinoma
Colorectal tumors are the most common cause of LBO in about 60 % of cases [2]. Most of these tumors are adenocarcinoma and cause obstruction by luminal compromise and bowel wall thickening.
On plain radiograph, left-sided LBO usually causes a dilatation of most part of the large-bowel loops (Fig. 1), whereas right-sided LBO sometimes causes gasless ascending colon and gaseous small-bowel dilatation, which mimicks small-bowel obstruction (Fig. 2). For differentiation between right-sided LBO and small-bowel obstruction, it is important to see whether the cecum and ascending colon are filled with fecal materials without gas, which we call as “dilated cecal sign”, suggesting right-sided LBO (Fig. 3).
A 56-year-old man presented with slowly progressive abdominal fullness and vomiting. The erect (a) and supine (b) abdominal radiographs showed markedly gaseous dilatation of the entire colon. On erect XP, air–fluid level was seen in the sigmoid colon (a). On barium enema (c), annular stenosis was depicted, which was pathologically confirmed as adenocarcinoma of the rectum
A 64-year-old woman presented with nausea and vomiting. Abdominal radiograph revealed several dilated small-bowel loops (a) with air–fluid levels (b), mimicking small-bowel obstruction. Subsequent barium enema showed complete obstruction of the barium column at the mid-ascending colon (c). The operative specimen revealed Borrmann type-2 ascending colon cancer
A 72-year-old man with ascending colon cancer. The erect abdominal radiogram (a) showed markedly dilated ascending colon with short air–fluid level, which we have called as “dilated cecal sign”. The CT scan revealed the enhanced mass lesion (arrow) in the ascending colon and numerous dilated small-bowel loops (b). The operative specimen confirmed ascending colon cancer (c)
Contrast enema using barium or water-soluble iodinated contrast medium is the conventional radiologic examination for evaluating patients with suspected obstructing colon carcinoma. Although contrast enema can show the obstructing lesion, the search for other more proximal tumors is difficult in the setting of LBO.
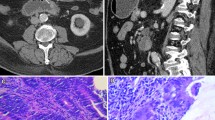
CT, especially MD-CT, becomes a main problem-solving tool for neoplastic LBO [4, 5]. MD-CT can demonstrate the well-enhanced tumor as a cause of LBO and help assess the tumor extension, involvement of adjacent structures, associated lymphadenopathy, and intraperitoneal metastasis using the multiplanar reconstruction (MPR) of the sagittal and coronal images [4] (Fig. 4).
Obstructive colitis
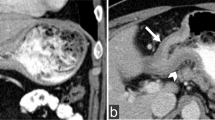
Ischemic colitis proximal to an obstructing colon carcinoma has been termed obstructive colitis. Pathologically, it is an ulcero-inflamatory disorder, proximal to a complete or partial obstructive lesion in the large intestine. Characteristically, there is a normal intervening colonic segment of variable length separating the proximal ulceration and inflammation from the distal obstruction [6–8]. Adenocarcinoma of the colon has been the predominant obstructing lesion. Obstructive colitis shows a proximal thumb-printing bowel loop on barium study (Figs. 5 and 6) and an edematous submucosal thickening, a pericolic vascular engorgement, and a thickening of an adjacent fascia on CT [9] (Fig. 6), which may often be over-staged as a tumor infiltration (Fig. 6). Pathologically, the severity of colitis ranges from a single discrete ulcer to an extensive area of fulminant colitis. Clinically, obstructive colitis is often misdiagnosed as ischemic colitis not only on clinical aspects but also on CT findings as the enhanced mass lesion distal to the ischemic colonic lesion is often overlooked (Fig. 5).
A 59-year-old male presented with a sudden onset of abdominal pain and nausea at midnight. Laboratory exam revealed elevated WBC (19,200/μl; normal 4,000–8,000/μl) and elevated CRP (19.42 mg/dl; normal <0.1 mg/dl). The post-contrast CT images showed marked submucosal edema of the transverse colon and splenic flexure, suggesting ischemic colitis (a). The subsequent barium enema exam showed prominent thumb-printing appearances in the transverse colon and splenic flexure (b). This patient was treated for ischemic colitis, and colonoscopy revealed a cancerous stenosis in the splenic flexure, and preoperative barium enema confirmed annular stenosis in the splenic flexure (c). Retrospectively, the enhanced mass lesion could be missed on initial CT (d). Three weeks later, the operative specimen showed annular colon cancer without residual ischemic changes macroscopically (e)
A 67-year-old woman presented with acute left-sided abdominal pain several days after her left knee surgery. Post-contrast CT images (a, b) showed enhanced mass lesion in the descending colon with pericolic fluid accumulation and submucosal edema in the transverse colon. Barium enema revealed long-segment annular stenosis in the descening colon (c). The operative specimen showed descending colon cancer without trans-serosal invasion microscopically
Adult intestinal intussusception
Approximately 5 % of all intussusceptions occur in adults, accounting for 1 % of all bowel obstruction [10, 11]. Adult intussusception is frequently caused by a serious underlying disease in 70–90 % [10, 11].
The classic CT appearances of intussusception include target appearance (intraluminal soft tissue mass and eccentric fat density), reniform pattern (bilobed density with peripheral high-density attenuation and low attenuation centrally), and sausage pattern (alternating areas of low and high attenuation related to the bowel wall, mesenteric fat and fluid, intraluminal fluid, contrast material, or air) (Fig. 7) [12]. CT is also useful in differentiating intussusception with lead point from transient intussusception without lead point (no underlying disease). Several features including a short-segment (less than 3.5 cm) proximal small-bowel (jejunal) intussusception without an obstructing sign and leading point in asymptomatic patients may suggest transient intussusception, which can be managed with a nonsurgical method [11–13]. More than one-half of large-bowel intussusceptions are associated with malignant lesions, including primary tumors and metastatic disease [11]. Adenocarcinoma of the colon is the most common malignant neoplasm causing colonic intussusception [12]. CT can depict the leading mass lesion more easily than in small-bowel intussusception.
A middle-aged man presented with acute abdominal pain, diarrhea, and a little rectal bleeding. Lab exam showed elevated WBC (19,200/μl; normal 4,000–8,000/μl) and reduced serum albumin (3.8 g/dl; normal 3.9–4.9 g/dl). Post-contrast CT of the whole abdomen showed intussusception in the lower rectum (a). The sagittal reconstructed images depicted well the appearance of the intussusception including the enhanced mass lesion and a large amount of mesenteric fat (b). Emergent barium enema showed a “coiled spring” appearance in the rectum (c)
Barium enema shows streaks of barium extended around the mass, producing a “coiled spring” configuration. Surgical resection is usually recommended because of the chance of perforation and potential spillage of microorganism and malignant cells as a complication of perforation caused by a non-operative reduction [9]. However, a cautious attempt at hydrostatic reduction may be contemplated when the patients is partially or completely obstructed but without clinical, laboratory, or radiological evidence of bowel ischemia [14].
Colonic obstruction caused by external neoplastic causes
Colonic obstruction is often caused by external neoplastic stenosis. The spread of neoplasms within the peritoneal cavity occurs by the processes of direct invasion, intraperitoneal seeding, hematogenous metastases, and lymphatic extension [15]. The pattern of involvement and the respective effects of secondary malignancies of the colon present the characteristic radiologic features on contrast enema study as well as on CT study. Differentiating colonic obstruction caused by external neoplastic causes from primary colon cancer is usually not difficult on clinical history and imaging findings (Fig. 8). Yet sometimes, the symptoms induced by a secondary lesion present clinically earlier than those by the primary malignancy, when the diagnosis is not easy (Fig. 9).
Conclusion
Accurate and early definitive diagnosis may reduce morbidity and mortality among patients with LBO. MD-CT is a reliable tool in predicting the presence of associated strangulation and bowel ischemia that require urgent surgical intervention. MPR images help assess the lesion identification and involvement of adjacent structures. The quicker imaging time allows acquisition of diagnostic images even in critically ill and uncooperative patients. Radiologists should be familiar with the CT features of various causes of LBO to decide on the treatment of patient with LBO.
References
Sinha R, Verma R (2005) Multidetector row computed tomography in bowel obstruction. Part 2. Large bowel obstruction. Clin Radiol 60:1068–75
Taourel P, Kessler N, Lesnik A, Pujol J, Morcos L, Bruel JM (2001) Helical CT of large bowel obstruction. Abdom Imaging 28:267–75
Hayakawa K, Tanikake M, Yoshida S et al (2012) Radiological diagnosis of large-bowel obstruction: nonneoplastic etiology. Jpn J Radiol 30:541–552
Frager D, Rovno S, Baer JW, Bashist FM (1998) Prospective evaluation of colonic obstruction with computed tomography. Abdom Imaging 23:141–46
Aufort S, Charra L, Lesnik A, Bruel JM, Taourel P (2005) Multidetector CT of the bowel obstruction: value of pos-processing. Eur Radiol 15:2323–2329
Gramtama S et al (1995) Obstructive colitis: an analysis of 50 cases and a review of the literature. Pathology 27:324–329
Toner M et al (1990) Obstructive colitis. Ulceroinflammatory lesions occurring proximal to colonic obstruction. Am J Surg Pathol 14:719–728
Levine TS et al (1994) Obstructive enterocolitis: a clinico-pathological discussion. Histopathology 25:57–64
Ko GY et al (1997) Usefulness of CT in patients with ischemic colitis proximal to colonic cancer. AJR Am J Roentgenol 168:951–956
Agha FP (1986) Intussusception in adults. AJR Am J Roentgenol 146:527–531
Kim YH, Blake MA, Harisinghani MG, Archer-Arroyo K, Hahn PF, Pitman MB, Mueller PR (2006) Adult intussusception: CT appearances and identification of a causative lead point. RadioGraphics 26:733–44
Horton KM, Fishman EK (2008) MDCT and 3D imaging in transient enteroenteric intussusception: clinical observations and review of the literature. AJR Am J Roentgenol 191:736–742
Sundaram B, Miller CN, Cohan RH, Schipper MJ, Francis IR (2009) Can CT features be used to diagnose surgical adult bowel intussusception? AJR Am J Roentgenol 193:471–478
Begos DG, Sandor A, Modlin IM (1997) The diagnosis and management of adult intussusception. Am J Surg 173:88–94
Meyers MA (1980) Pattern of spread of malignancy to the colon. In: Marshak RH, Lindner AE, Maklansky D (eds) Radiology of the colon. Philadelphia, Saunders, pp 335–366
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hayakawa, K., Tanikake, M., Yoshida, S. et al. Radiological diagnosis of large-bowel obstruction: neoplastic etiology. Emerg Radiol 20, 69–76 (2013). https://doi.org/10.1007/s10140-012-1088-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-012-1088-2