Abstract
Shoulder injuries, including acromioclavicular (AC) joint separations, remain a common reason for presentation to the emergency room. Although the diagnosis can be made apparent through proper history and physical examination by the emergency medicine physician, ascertaining the degree of injury can be difficult on the basis of clinical evaluation alone. While there is consensus in the literature that low-grade AC joint injuries can be treated with conservative management, high-grade injuries will generally require surgical intervention. Furthermore, the treatment of grade 3 injuries remains controversial, making it incumbent upon the radiologist to become comfortable with distinguishing this diagnosis from lower or higher grade injuries. Imaging of AC joint injuries after clinical evaluation is generally initiated in the emergency room setting with plain film radiography; however, on occasion, an alternative modality may be presented to the emergency room radiologist for interpretation. As such, it remains important to be familiar with the appearance of AC joint separations on a variety of modalities. Another possible patient presentation in both the emergent and nonemergent setting includes new onset of pain or instability in the postsurgical shoulder. In this scenario, the onus is often placed on the radiologist to determine whether the pain or instability represents the sequelae of reinjury versus a complication of surgery. The purpose of this review is to present an anatomically based discussion of imaging findings associated with AC joint separations as seen on multiple modalities, as well as to describe and elucidate a variety of potential complications which may present to the emergency room radiologist.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Traumatic injuries, including fractures and dislocations, remain among the most common reasons for a visit to the emergency room in the USA today [1]. Among these injuries, AC joint separations encompass up to 12 % of dislocations involving the shoulder [2]. This type of injury is particularly common among young male athletes, who have a five-time greater incidence over their female counterparts [2]. Proper clinical history, in conjunction with physical examination findings, may illuminate the diagnosis forthright. However, in many cases, the role of imaging remains paramount in the proper diagnosis and classification of shoulder injuries and in particular AC separations. With regards to AC separations, the most common mechanism of injury involves a blow to the acromion with the shoulder in the adducted position. A predictable pattern of traumatic tearing ensues, beginning with disruption of the AC ligaments, followed by the joint capsule, the coracoclavicular (CC) ligaments, and finally the deltotrapezial fascia [3]. This is usually due to a direct force mechanism of injury from a fall onto the superolateral aspect of the shoulder [3]. Activities commonly associated with this type of injury include a variety of sports in which traumatic contact is common, such as tackle football or falling from a bike while cycling. AC separations are particularly common amongst football players, with the reported incidence of AC separations among shoulder injuries in this population accounting for around 40 % overall [4]. Indirect mechanisms of injury are also possible, including a superiorly directed force due to a fall onto an outstretched hand or elbow, a history that is common to a variety of different osseous and ligamentous injuries other than AC joint separation. The most common initial complaint among patients who have sustained this injury is pain, which can be extreme in nature. Physical examination findings can vary with the degree of injury, although the most frequent include regional swelling and/or bruising.
Despite what may seem to be a readily apparent clinical diagnosis, imaging remains an important component of the complete workup of AC joint separation due to potential surgical implications, which are based upon the grade of injury. Plain radiography has continued to be the mainstay of initial imaging for this type of suspected injury in both the emergency room and ambulatory settings. However, evaluation of higher-grade injuries, including of potential ligamentous injury, may require the use of additional imaging modalities such as multidetector computed tomography (MDCT) or magnetic resonance imaging (MRI). Specifically, MDCT can be helpful in situations that require precise delineation of the alignment of the joint, which is not sufficiently demonstrated on plain radiography. MRI provides superior evaluation of the integrity of the ligaments as well as other soft tissue injury. While the role of ultrasound in the evaluation of acute traumatic shoulder injuries as well as arthritic changes of the AC joint has been described, its utilization remains limited, most likely secondary to a number of confounding factors for use in the emergency room setting. These include the availability of the proper ultrasound transducers, as well as the necessity for proper technique and methodology when evaluating the AC joint, which is currently not widely taught [5, 6].
The purpose of this review is to (1) discuss the anatomical basis for the classification of various types of acromioclavicular joint separations, including important points of differentiation between each grade, (2) review the different treatment options for these injuries, including the controversial grade 3 injury, (3) describe what can be expected to be seen by the radiologist on post-surgical imaging, and (4) demonstrate different complications for which patients may present to the emergency radiologist such that the imaging appearances are familiar when investigating the source of pain in the postoperative patient. We will first review the anatomy of the shoulder, including key anatomical landmarks and how these are optimally imaged. We will then present the current accepted classification scheme for acromioclavicular joint separations, the Rockwood classification system. Finally, we will describe and show the surgical repair of higher-grade acromioclavicular joint separations as well as their postoperative complications on plain radiography, as this is the most commonly utilized initial modality for imaging acute shoulder pain in the emergency room setting.
Normal anatomy of the AC joint
The AC joint is principally formed by the lateral margin of the distal clavicle and the medial surface of the acromion. An articular disc may be present between the articular surfaces. When present, typically, the disc incompletely separates the osseous structures, although on occasion complete separation can be seen. When the separation does occur, it is usually along the superior margin of the articulation. However, frequently, this articular disc is not present. Surrounding the articular margin, there is a joint capsule, which is lined by a synovial membrane [7]. In conjunction with this capsule are two ligaments located above and below the joint known as the superior and inferior AC ligaments. These structures provide restraint against horizontal translation of the joint [8].
The coracoclavicular (CC) ligament consists of two separate components: the conoid ligament and the trapezoid ligament. The conoid ligament is located medial to the trapezoid ligament, and the two are separated by either fat or a bursa. This ligament is conical in shape, with dense fibers that broadly span from the apical attachment at the base of the coracoid to its base at the conoid tubercle along the undersurface of the clavicle at the junction of the mid and lateral thirds. The apex of this ligament is located posteromedial to the trapezoid ligament and lateral to the scapular notch, coursing in a spiral fashion superiorly and nearly vertical in orientation [7]. The primary function of the conoid ligament is to resist anterosuperior clavicle translation and rotation. The trapezoid ligament is the anterolateral fasciculus of the coracoclavicular ligament and is quadrilateral in shape. The principal source of resistance against posterior displacement of the clavicle, it also renders some resistance to superior, inferior, and anterior forces [9]. Thinner than the conoid ligament, its inferior attachment is found along the superior surface of the coracoid process, while its superior attachment is to the oblique ridge of the undersurface of the clavicle. The ligamentous anatomy of the acromioclavicular joint is illustrated in Fig. 1.
The ligamentous anatomy of the acromioclavicular joint. The acromioclavicular (AC) joint is a complex joint with numerous ligamentous support structures. Of particular importance when assessing injuries to the AC joint are the acromioclavicular ligaments [4] and the coracoclavicular ligament, which is composed of the conoid and trapezoid ligaments [2, 3]. In addition to these ligaments, an articular disc may be present between the clavicle and the acromion. The normal AC interval is approximately 1–6 mm. The normal CC interval is approximately 11–13 mm. Additional structures are as labeled
Two muscular attachments to the acromion that are worth noting are the trapezius and deltoid muscle attachments. Both muscles have attachments to the acromion and the scapular spine. The trapezius has its insertion on the superior aspect of these two osseous structures, while the deltoid has origins from the inferolateral aspect of both structures. Along the spectrum of AC joint injuries, a defect in the deltotrapezial fascia is indicative of a significant injury [3].
Imaging of the AC joint
As with many direct blow injuries in the emergency room setting, initial imaging of the AC joint is usually performed via plain radiography. The normal distance between the distal clavicle and the acromion ranges from approximately 1 to 6 mm, while the normal coracoclavicular distance is approximately 11 to 13 mm [2]. Due to the nature of the most common mechanism of injury, that being direct force trauma, unilateral separation is suspected in most instances. However, the AC joints should ideally be imaged bilaterally, even when unilateral injury is suspected. This is due to the natural anatomic variation inherent to this joint, requiring the opposite side for comparison [10]. The importance of bilateral imaging of the AC joints in cases of suspected separation is demonstrated in Fig. 2. An AP view of the AC joints with or without cephalic tube angulation serves as the standard for initial imaging. While a straight AP view allows for more anatomical positioning of the joint, angulating the tube in a cephalic direction does have the advantage of projecting the AC joint with increased separation from the proximal aspect of the acromion [10]. Consideration should be given to reducing radiation dose to the patient during imaging. Different exposure methods can be utilized in this regard, though the method of choice is generally facility dependent. As AC separations are an injury that is more commonly present in young patients, careful attention to minimizing radiation dose to the patient’s thyroid gland is always prudent. At our institution, we utilize a separate exposure method, in which the images are coned down to the AC joint utilizing a single cone with imaging of the two sides performed separately. Inherently, this method reduces the radiation dose to the patient’s thyroid as it is not directly exposed to the radiation beam. The primary disadvantage of this method, however, is that separate exposures allow for increased variance between projections, which may render the images untenable for comparison. As an alternative to separate exposures, a customized binocular cone may be used to simultaneously image the AC joints while also minimizing radiation exposure to the patient’s thyroid by avoiding direct beam exposure. However, as this type of cone is not widely available in general practice, this view is not routinely obtained.
Bilateral imaging. It is ideal to image the AC joints bilaterally when a separation is suspected, even when the injury is thought to be unilateral. a AP view, b Zanca view, and c axillary views of the right shoulder. This patient presented after falling from his bicycle onto his shoulder. There is apparent inferior displacement of the acromion relative to the position of the clavicle. This was initially diagnosed as a grade 3 AC separation. d Zanca views of the bilateral shoulders demonstrate a symmetric appearance to the AC joints, indicating the position of the acromion relative to the distal clavicle is likely normal anatomy for this patient
On occasion, it may be helpful to further exaggerate the suspected separation by utilizing other views. To this end, a weight-bearing or stress view is utilized at some institutions, including our own, to help differentiate between grades of injury. In particular, this view is thought to be helpful in differentiating between grade 2 and 3 separations. It may also be useful in ascertaining whether or not a separation truly exists. However, the ultimate utility of the weight-bearing view is somewhat controversial. A study performed by Bossart et al. [11] found that weight-bearing views were only able to reveal a higher-grade injury in 4 % of cases, which would indicate that this view is of limited clinical value. In addition, an analysis performed by Vanarthos et al. [12] on cadaveric models showed that an AP view with the shoulder in internal rotation may occasionally be sufficient for diagnosis of grade 3 injuries, thus alleviating the potential pain that would be experienced by a patient with an acute shoulder injury during a weight-bearing view. Furthermore, the method by which the weight-bearing view is performed has also provoked some controversy, with differences of opinion over whether it is appropriate to have the patient hold weights in his/her hands versus having the weights hanging from the wrists. While theoretically holding the weights can cause contraction of the trapezius muscle and reduce the visibility of a separation [13], a study evaluating the difference in effect under real-time ultrasound showed no significant difference in the amount of distraction when comparing hand-held weights versus weights which were suspended from the wrists [14]. Regardless, the weight-bearing view is performed either by having the patient hold weights (e.g., sandbags) or suspending the weights from the patient’s wrists, with each weight weighing approximately 10–15 lbs. A difference in craniocaudal measurement of >3 mm from the nonweight-bearing view is considered abnormal (Fig. 3) [15]. As another alternative to the weight-bearing view, advanced imaging modalities such as MDCT can provide a more detailed analysis of osseous displacement, though at the cost of increased radiation exposure to the patient.
Non-weight-bearing vs. weight-bearing views. AP views of the left clavicle a without weight-bearing/arm in external rotation and b with weight-bearing/arm in internal rotation. Note the increased displacement between the clavicle and the acromion in this patient with a grade 1 AC separation. The weight-bearing view is obtained with a 10–15-lb weight hanging from the patient’s wrist in an attempt to exaggerate the distance between the distal clavicle and the acromion in more subtle cases. A difference in measurement of the AC distance of >3 mm between the two views is considered abnormal. Note that placing the arm in internal rotation can help to facilitate visualization of this difference
Another view that can be useful is a Zanca view (Fig. 4). In order to obtain a Zanca view, the X-ray tube is centered at the AC joint with a 10–15 ° cephalic tilt. The standard kilovoltage is also decreased up to 50 % in order to better visualize the soft tissues and to increase joint detail [10]. If there is continued suspicion for an AC joint separation, but the separation remains poorly demonstrated on the standard views, additional stress views while placing the patient’s arm on the affected side in a variety of positions may help accentuate the separation. A potential confounding factor in the diagnosis of AC joint injury in the emergency room setting is that patients may be imaged at the bedside while recumbent or at an angle other than the upright position. Placing the patient in an erect position not only properly orients the patient for the exam but also allows gravity to assist in demonstrating the separation.
Advanced methods for imaging the AC joint include CT and MRI. CT image acquisition is generally straightforward as imaging in the transaxial plane utilizing bone and soft tissue windows can be reconstructed in the sagittal and coronal planes. In addition, 3D volume rendering can be helpful in difficult cases to improve visualization of the degree and trajectory of bony displacement. Furthermore, CT may better demonstrate subtle fractures, which can be missed on the plain radiographs. However, while subtle fractures may be more readily apparent on CT, the findings compatible with AC joint separation are similar to those of plain film radiography but with the disadvantage of a much larger radiation dose to the patient. In general, CT is best reserved for cases in which there is a higher index of suspicion for a fracture rather than an AC separation. MRI is an ideal imaging modality for soft tissue evaluation, especially ligamentous injury. Sequence acquisition varies between various institutions, and satisfactory images can be obtained on a 1.5-T or a 3-T magnet, both of which are utilized at our institution. As an example, our image acquisitions of the AC joint comprise of the following sequences, which are modified from our shoulder MRI protocol with an extended field of view to visualize more medial structures: coronal T1, T1 with fat saturation (fat sat), and T2 fat sat, sagittal T1 fat sat, axial T1 fat sat, and an axial oblique T1 fat sat. The normal anatomy of the coracoclavicular ligament is best demonstrated on T1-weighted (T1W) images due to high contrast to noise, whereas on T2-weighted fat saturated images, these structures are slightly more difficult to delineate. Conversely, in the setting of injury, the edema related to trauma around these ligaments allows for improved identification of their fibers on T2 fat sat and intermediate-weighted, fat-saturated MR images, while these structures may become less conspicuous on the T1W images (Fig. 5) [9]. As a supplement, administration of intravenous gadolinium can further assist in depicting the path and full extent of soft tissue injury in fine detail [9]. It has been suggested that patients with more advanced degrees of injury requiring surgical reconstruction may benefit from having an MRI performed prior to surgery to define the full extent of injury, though the role of MRI in AC separations is not clearly defined [9]. Overall, MRI provides incomparable detail of the anatomy of the soft tissues surrounding the AC articulation. As a caveat regarding both CT and MR imaging, it is important to remember that the study is acquired with the patient in a recumbent position. Thus, the relative positions of the clavicle and acromion may be altered, particularly in less severe injuries. Furthermore, the advantage of gravitational assistance garnered from having the patient in an upright position when acquiring radiographs is lost, which again may mask the true extent of separation.
MRI anatomy of the AC joint. a Oblique coronal T1-weighted image of the left AC joint, profiling the superior (long black arrow) and inferior (white arrow) acromioclavicular ligaments. A portion of the intraarticular disc is visible (short black arrow). A acromion, C clavicle. b Oblique coronal T1-weighted image located anterior to the first image demonstrates the conoid (short black arrow) and trapezoid (long black arrow) portions of the coracoclavicular ligament. Notice that these two components are separated by a small amount of fat (white arrow). C clavicle, c coracoid
Classification of injuries
The original classification of AC joint separations was first described by Tossy and Allman in the 1960s [16, 17]. This classification scheme divided AC joint separations into three separate grades based primarily on the position of the distal clavicle relative to the acromion. An injury was considered grade 1 if the distal clavicle demonstrated normal anatomical alignment with the acromion, indicating only a sprain of the ligamentous structures. A grade 2 injury involved displacement of the clavicle that was <100 % of the clavicular width. This type of injury was thought to be associated with rupture of the AC ligaments and sprain of the otherwise intact CC ligaments. An injury was considered grade 3 when there was displacement of the distal clavicle >100 % of its width with a simultaneous 25–100 % increase in the coracoclavicular distance. The AC and CC ligaments were both considered ruptured in this type of injury. From this original classification system, modifications were made by Rockwood et al. in 1989 [18], bringing about the classification system that is currently used in practice by radiologists. This classification system involves six different grades of AC joint separation. A summary of the Rockwood classification system along with pertinent radiographic findings associated with each grade can be found in Table 1.
Grade 1 injury
Grade 1 injuries of the AC joint can be difficult for the emergency radiologist to appreciate without the proper clinical context, as the joint may appear normal on plain radiography. An injury is considered grade 1 when there is a sprain of the AC ligaments without a complete tear. Clinically, patients with this type of injury may present with tenderness (with or without swelling) in the region of the AC joint. However, typically, there is no tenderness in the area of the CC interspace. While this type of injury may be seen to better advantage on MRI, plain radiography is often the initial and only modality encountered by the emergency radiologist. On radiographs, findings include possible mild swelling or edema of the soft tissues overlying the AC joint. The joint itself is often normal in appearance (Fig. 6). This type of injury is suggested when there is >2 mm separation between the distal clavicle and the acromion. However, it should be noted that this measurement is confounded by a number of factors that are often encountered by the emergency radiologist including suboptimal imaging technique or patient positioning. When this type of injury is suspected, it can be helpful to obtain a dedicated AC joint image such as the previously described Zanca view or a comparison view of the contralateral side. A weight-bearing view may further assist in confirming the diagnosis. However, if radiographs are normal and there is continued clinical suspicion for a grade 1 injury, an MRI can be a helpful and more definitive examination. As demonstrated in Fig. 7, fluid-sensitive MRI sequences such as short tau inversion recovery can vividly demonstrate edema about the AC joint with distension of the capsule, findings that are consistent with a sprain. MRI can also be utilized to demonstrate a complete ligamentous tear, the presence of which would disqualify the injury for classification as a grade 1 injury. However, it is important to note that while MRI can be a useful examination, there are no specific signs on MRI that indicate a grade 1 separation. This is especially true in adult patients, as signal abnormalities in the region of the AC joint are a common finding [9]. Overall, this is the most common type of AC joint injury encountered in clinical practice, and as such, it is important for the emergency radiologist to remain mindful of this diagnosis.
Grade 2 injury
Grade 2 injuries are another common type of AC joint separation, which are often more clinically apparent than the grade 1 injury. Together with grade 1 separations, they occur twice as frequently as the remaining grades of injury [19]. In a grade 2 injury, there is disruption of the AC joint capsule with tearing of the AC ligaments, causing horizontal instability. The CC ligaments remain intact. The patient usually presents with tenderness and swelling over the AC joint, similar to a grade 1 injury. However, unlike with a grade 1 injury, there is also point tenderness over the CC interval. As the CC ligaments are still intact, vertical stability is overall preserved, and elevation of the distal clavicle is usually not well appreciated on physical examination. On plain radiography, the AC joint is disrupted with widening of the AC joint space. While widening of the CC interspace may also be present, the increase in distance should be <25 % [9] (Fig. 8).
Grade 3 injury
Although grade 1 and 2 injuries are the most common type of AC joint separation, grade 3 injuries are still relatively frequently encountered, reportedly comprising up to 40 % of AC separations [20]. In grade 3 injuries, there is further progression along the spectrum of ligamentous disruption. Along with tearing of the AC ligaments, grade 3 separation involves tearing of the CC ligaments as well as a higher grade tearing of the AC joint capsule. Patients with this type of injury present with symptoms of pain and restricted motion of the affected side. On physical examination, the distal clavicle is often prominent in appearance and presents as a palpable bump due to cranial translation. While there is elevation of the distal clavicle relative to the acromion, the displacement is reducible. Radiographically, there is widening of the AC joint as well as a 25–100 % increase in the size of the CC interspace (Fig. 9). In general, this grade of separation can usually be seen without the assistance of weights. This type of injury should be distinguished from a fracture of the articular surface of the distal clavicle. These injuries can share a common history of direct blow trauma as well as an appearance of displacement at the articular surface on plain radiography. As the fracture may be subtle, it can be difficult to distinguish these two entities. However, unlike a grade 3 separation, the articular fracture does not inherently involve disruption of the ligaments about the AC joint. Interestingly, the management strategies of grade 3 separations and intraarticular fractures of the lateral third of the clavicle are both controversial and with significant overlap, with advocates of nonoperative and operative management in the literature for both types of injury. Conservative management for both injuries involves a sequence of immobilization followed by structured rehabilitation, while operative management involves different types of fixation with or without distal clavicular resection, with varying degrees of success [21]. Evaluation of the joint with additional views can often be helpful in differentiating these two entities, or alternatively, CT can be useful to definitively identify a fracture line or a fracture fragment. Management options for grade 3 injuries are discussed later under “Treatment options.”
AP view of a grade 3 separation. Grade 3 separations are more severe than grade 2. There may again be widening of the AC joint space (solid arrows). However, the distinguishing feature of a grade 3 separation is a tear of the CC ligament, with resulting 25–100 % increase in the CC interspace (dashed arrows)
Grade 4 injury
Overall, grade 4 AC separations are relatively rare in clinical practice. Grade 4 injuries involve AC joint separation with displacement of the distal clavicle into or through the trapezius muscle. Unlike a grade 3 injury, this type of separation cannot be reduced, and on physical examination, there may be prominence of the anterior acromion. Radiographs can sufficiently demonstrate the posterior translation of the distal clavicle, and an axillary view is ideal for demonstrating this translation to greatest effect (Fig. 10). Although overall neurovascular injuries are uncommon in the setting of AC separation without a concomitant injury to the shoulder girdle [22], grade 4 injuries can be associated with damage to the ipsilateral brachial plexus [3]. In addition to symptoms of pain and alteration of motion in the affected shoulder, patients can present with symptoms of brachial plexopathy, ranging from mild weakness and numbness to complete lack of feeling and movement in the ipsilateral arm. As such, an MRI of the brachial plexus may be necessary in the context of clinical symptoms suggestive of an associated injury.
Grade 4 separation. Axillary view of the left AC joint demonstrating posterior displacement of the distal clavicle. Grade 4 separations are distinguished by posterior displacement of the clavicle into or through the trapezius muscle. This displacement is best appreciated on an axillary view. Clinically, the AC joint will be irreducible, with prominence of the anterior acromion. In patients with suspected grade 4 injury, it is important to evaluate the sternoclavicular joint for a possible bipolar clavicular dislocation
Bipolar clavicle dislocation
When evaluating a grade 4 injury, it is important to view both the proximal and distal ends of the clavicle to not only search for AC joint pathology but also to assess the alignment of the sternoclavicular (SC) joint. This is important in order to exclude the possibility of a bipolar clavicular dislocation (Fig. 11). Such bipolar dislocations of the clavicle are rare and are usually associated with an indirect mechanism of high-energy trauma, such as an impactful blow to the lateral aspect of the shoulder or truncal torsion with simultaneous pressing together of the shoulders [23]. These types of injuries can be referred to by a variety of names, including traumatic floating clavicle, panclavicular dislocation, or bifocal clavicle dislocation [24]. Treatment of this type of injury can range from conservative management in the asymptomatic patient to open reduction and internal fixation in patients with pain, instability, or requirements of higher functionality. In chronic cases, this type of injury has also been treated with total claviculectomy [24]. It is crucial for the emergency radiologist to recognize this entity when present, as overlooking the bipolar nature of the injury can result in insufficient management by directing the focus of the surgeon’s attention to a single area of separation, leading to poor functional outcomes.
Floating clavicle. a AP view of the right clavicle demonstrates a readily apparent AC separation. There is also disruption of the sternoclavicular joint (arrow), though this is more difficult to appreciate due to overlapping shadows on this view. b Angled view demonstrates this disarticulation to better advantage. Note the relative position of the proximal right clavicle compared to the opposite side (circles). c 3D surface rendered reconstruction from a CT scan better demonstrates the separation of both the right AC and SC joints, causing the clavicle to be “floating”
Grade 5 injury
With grade 5 injury, there is further propagation of damage to the supporting structures, including complete disruption of all of the stabilizing ligaments of the AC joint as well as extensive detachment of the deltoid and trapezius muscles and fascia. Similar to a grade 3 injury, there is elevation of the distal clavicle relative to the acromion, although with grade 5 injury >100 % CC interspace widening can be seen. The cranial translation of the distal clavicle can be marked on clinical exam, with subcutaneous positioning of the clavicle noted on physical exam. Unlike a grade 3 injury, this AC joint separation is irreducible on physical exam (Fig. 12).
AP view of a grade 5 separation. In grade 5 separations, there is complete disruption of all of the stabilizing ligaments of the AC joint. There is >100 % increase in the CC interspace (arrows). This appearance implies extensive detachment of the deltoid and trapezius muscles and fascia. Unlike a grade 3 separation, clinically these separations are irreducible. A focus of heterotopic ossification is seen inferior to the distal clavicle, consistent with chronic injury
Grade 6 injury
A grade 6 injury occurs when there is separation of the AC joint with displacement of the distal clavicle into a subacromial or subcoracoid position. Often, a history of high-impact trauma while the patient’s shoulder is in an externally rotated, hyperabducted position can be elicited. Given the association with high-energy trauma, these injuries often are seen with multiple fractures of the ribs and the clavicle [3]. Much like the grade 4 injury, which also involves multiplanar displacement of the distal clavicle, the subcoracoid displacement of the distal clavicle has an increased incidence of associated brachial plexus and/or vascular injury. In the context of clinical symptoms such as numbness in the extremity, an MRI of the brachial plexus can be helpful for further evaluation. Furthermore, vascular injury in a patient with diminished or absent pulses may be assessed with an angiographic examination such as an MR angiogram or a conventional angiogram.
Treatment options
Treatment options for AC joint separations vary depending on the grade of separation and are summarized in Table 2. Several studies in both the surgical and physical rehabilitation medicine literature support a conservative approach to management of the grade 1 or 2 separation [25–27]. Several methods of management and rehabilitation of the injury have been espoused, including a four-phase method of immobilization followed by rehabilitation in a study of athletes with low grade AC joint separations [25]. Occasionally, patients may complain of continued pain in the joint following nonsurgical management, which may be secondary to the development of arthritic changes in the joint. In cases where nonsurgical management fails either due to pain or inappropriate level of function for the patient’s level of activities, surgery may provide a better result, though these instances are rare [28]. Additional studies in the surgical literature have shown the advantage of operative management of grade 4–6 injuries [25, 29]. The management of grade 3 injuries remains controversial. With studies both in support of and against surgical management, a true consensus regarding treatment of this injury remains elusive [30, 31]. Irrespective of the ultimate course of treatment, it remains important to recognize grade 3 injury so that an appropriate discussion between the patient and the clinician regarding future management can take place.
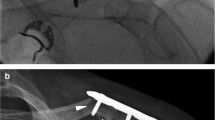
A variety of different surgical methods have been devised to correct the mechanical and physical derangement associated with this injury, and it is important to be familiar with these methods in order to appropriately recognize the findings on postoperative imaging. The common goal of all methods of surgical fixation is to reestablish and to maintain anatomical AC joint alignment through open and/or arthroscopic reduction. In general, these procedures also attempt to repair the deltotrapezial fascia if it is disrupted as well as to debride the articulation. A procedure that was utilized in the past was primary pin fixation to affix the clavicle to the coracoid base. Although findings related to this procedure may be encountered in older patients, this method is no longer utilized secondary to the rare but disastrous complication of pin migration, with case reports of migration into the great vessels and spinal canal [32, 33]. Primary fixation with other devices is still performed today, including use of a hook plate, which is primarily performed in Europe [34, 35] (Fig. 13). This procedure can be performed with or without reconstruction of the ligaments. Ligament reconstruction was first described by Weaver and Dunn, and a modified Weaver–Dunn procedure remains a common choice among orthopedic surgeons [36, 37] (Figs. 14 and 15). As initially described, this procedure involved three principle steps including resection of the distal 2 cm of the clavicle, detaching the acromial attachment of the coracoacromial ligament, and suturing this attachment to the distal clavicle [38]. The distal clavicle resection portion of the procedure attempts to avoid late degenerative changes, a step that has found favorable support in the surgical literature [39, 40]. While distal clavicle resection does offer the advantage of potential avoidance of late osteoarthrosis, it does increase the possibility of destabilization of the joint, a point that should be kept in mind by the radiologist viewing the postoperative imaging. Open or arthroscopic distal clavicle resection may also be used in the rare instances of grade 1 or 2 injury, which develop severe arthritic changes that limit the functionality of the joint [28]. At our institution, the predominant method of choice for surgical reconstruction is coracoclavicular fixation utilizing a double endobutton technique (Fig. 16). Generally, this method of repair involves placement of a loop of synthetic material between the coracoid process and distal clavicle, allowing for joint strength and stiffness equal to or greater than that of the native anatomy [41].
Diagram of a modified Weaver–Dunn procedure with tendon augmentation. Resection of the distal clavicle is performed in an attempt to prevent osteoarthrosis. The coracoacromial ligament is then mobilized and sutured into the newly resected distal clavicle for stabilization of the joint (circle). Tendon or suture augmentation can further support joint stabilization (arrow). Other methods of enhancing joint stability include tape cerclage or use of other types of graft material
Intraoperative photographs from an AC separation repair utilizing a modified Weaver–Dunn technique. a The distal clavicle has been resected (asterisk). In addition, one end of an autologous graft has been affixed to the coracoid process. The other end (arrow) will be affixed to the clavicle. b The remaining end of the graft is affixed to the clavicle, completing the reapproximation of the torn coracoclavicular ligaments (photographs are courtesy of the Department of Orthopedic Surgery at the University of Southern California)
Diagram of endobutton technique. An endobutton is inserted through surgically created tunnels in the clavicle and the coracoid (circle). This recreates the conoid portion of the CC ligament. A second endobutton insertion may also be used to recreate the trapezoid portion. This procedure can also be performed in conjunction with a distal clavicular resection to prevent osteoarthrosis (arrow)
Imaging of potential postoperative complications
The imaging of the postsurgical AC joint will vary based on the type of surgery that was performed, and knowledge of the surgical history is paramount to proper evaluation. Expected postsurgical findings include near or complete restoration of the normal alignment of the AC joint with or without the presence of radiopaque hardware, partial resection of the distal clavicle, and osseous tunneling related to graft placement. When present, the margin of the resected distal clavicle should be sharp and without evidence of lucency out of proportion to the patient’s overall bone mineralization. While there is variability in the amount of clavicle resected, it has been shown that, in terms of prevention of complications, a resection margin of 0.8–1 cm is optimal for prevention of postsurgical complications related to the resection. Resection margins above or below this range are more susceptible to complications related to over- or underresection, respectively [42]. A myriad of postoperative complications may occur, many of which can be readily diagnosed by the radiologist. The various methods of surgical reconstruction are geared toward prevention of these complications. The most common complication is late osteoarthrosis. Findings on plain radiography suggestive of the diagnosis include osteophyte formation and foci of heterotopic calcification (Fig. 17). Persistent instability is another commonly encountered postsurgical complication [41]. This instability may be related to a number of different etiologies including postoperative osteolysis or graft insufficiency. When available, baseline radiographs following surgery can be invaluable for proper evaluation of potential postsurgical pathology. These baseline studies can be particularly useful when evaluating for osteolysis, as it can be difficult to differentiate between the expected postsurgical AC interval and early osteolysis. However, over serial examinations, osteolysis will progress, while postoperative changes should remain stable (Fig. 18). Furthermore, as subtle changes over time that may lead to instability will not be readily appreciated on a single radiograph, a baseline comparison can be extremely helpful in making this observation on subsequent exams. When evaluating the postoperative radiograph, the degree of widening of the joint space should also be noted, as overzealous resection can contribute to joint instability [40].
Osteolysis. a AP view of the left AC joint following endobutton repair of a grade 5 AC separation. Note the bone density of the distal clavicle as well as the space between the distal clavicle and the acromion. b AP view of the left AC joint 5 months later. There is distal resorption of bone with widening of the AC interval, consistent with osteolysis. Note the orientation of the more cranial endobutton has changed. Though readily apparent in this patient, this case illustrates the importance of utilizing baseline postoperative radiographs for comparison when they are available
Graft insufficiency or rupture is another potential cause of post-surgical AC joint instability. Though the range of incidence of graft failure varies by procedure and between different studies, overall graft failure leading to chronic subluxation or disruption has been reported to be as high as 30 % [43]. While some grafts have a radiopaque component like an endobutton, other types of graft material used for fixation may be radiolucent. It is thus important for the emergency radiologist to consider this potential complication as a source of instability when there is abnormal alignment of the postoperative AC joint, even in the absence of visible hardware or graft material (Fig. 19).
Graft failure. a Baseline AP view of the left AC joint following endobutton fixation. b AP view of the left AC joint 7 months after surgery. Note the stretching of the graft as evidenced by increased distance between the radioopaque components of the endobutton graft. Graft failure is a potential source of postsurgical instability of the AC joint, as evidenced in this case by the increased craniocaudal interval between the distal clavicle and the acromion
Failure of the surgical hardware used for AC joint reconstruction can also be seen independent of or in conjunction with the aforementioned complications, emphasizing the importance of prior imaging for comparison to insure the integrity of the instrumentation. One such complication includes migration of the device used for or to support the fixation (Fig. 20). A more serious complication includes a delayed fracture at the surgical site, which can be seen on either plain film or MDCT (Fig. 21). Postoperative infection is a potential complication as well, and suspicion for this complication may manifest itself on clinical exam. Although rare, damage to adjacent nerves, including the suprascapular nerve, or to blood vessels may occur during surgery. Injuries to these structures are best evaluated with MRI and angiographic imaging, respectively. Recognition of these complications is a crucial element of proper follow-up of the postsurgical shoulder, and it will often be the radiologist who initially recognizes the complication.
Hardware failure. a AP view of the right AC joint following endobutton reconstruction of an AC separation. Note the relationship of the caudal endobutton to the inferior margin of the coracoids. b AP view of the right AC joint 1 month later. The caudal endobutton has migrated superiorly, as evidenced by the new position of the endobutton relative to the inferior margin of the coracoid
Fracture and tunnel widening. a AP view of the right AC joint following endobutton reconstruction. Note the width of the tunnels as well as the position of the endobuttons. b AP view of the right AC joint 1 year after surgery. There is tunnel widening (arrows), which may have precipitated endobutton migration (middle arrow). A fracture of the coracoid process is also present (circle)
Summary
Shoulder pain as a result of traumatic injury will continue to remain a common indication for presentation to the emergency room, and the role of the radiologist in the proper diagnosis of AC joint separations is essential. As the grade of injury can profoundly impact the patient’s clinical management, the radiologist must maintain familiarity with the classification system for these injuries and with their appearances on various imaging modalities. Additionally, it is not uncommon for patients to present to the emergency room complaining of new onset of pain or instability following surgical management. Thus, knowledge of the different methods of surgical correction, as well as their imaging appearances, is of utmost importance. Finally, as the source of the patient’s complaint may be the result of a postoperative complication, it is necessary to be able to distinguish these entities from other potential causes of morbidity in order to help direct appropriate patient care.
References
National Center for Health Statistics (2011) Health, United States, 2010: with special feature on death and dying. National Center for Health Statistics, Hyattsville
Bucholz RW, Heckman JD (2001) Rockwood and Green’s fractures in adults, Chapter 29: acromioclavicular joint injuries, 5th edn. Lippincott Williams & Wilkins, Philadelphia, PA, pp 1210–1244
Simovitch R, Sanders B, Ozbaydar M, Lavery K, Warner JJP (2009) Acromioclavicular joint injuries: diagnosis and management. J Am Acad Orthop Surg 17:207–219
Kaplan LD, Flanigan DC, Norwig J, Jost P, Bradley J (2005) Prevalence and variance of shoulder injuries in elite collegiate football players. Am J Sports Med 33:1142–1146
Alasaarela E, Tervonen O, Takalo R et al (1997) Ultrasound evaluation of the acromioclavicular joint. J Rheumatol 24:1959–1963
Iovane A, Midiri M, Galia M et al (2004) Acute traumatic acromioclavicular joint lesions: role of ultrasound versus conventional radiography. Radiol Med 107:367–375
Williams PL, Bannister LH, Warwick R et al (1995) The anatomical basis of medicine and surgery. In: Gray H, Pick TP, Howden R (eds) Gray’s anatomy, 38th edn. Churchill Livingston, London, pp 619–622
Lee KW, Debski RE, Chen CH et al (1997) Functional evaluation of the ligaments at the acromioclavicular joint during anteroposterior and superoinferior translation. Am J Sports Med 25:858–862
Antonio GE, Cho JH, Chung CB et al (2003) MR imaging appearance and classification of acromioclavicular joint injury. Am J Roentgen 180:1103–1110
Ernberg LA, Potter HG (2003) Radiographic evaluation of the acromioclavicular and sternoclavicular joints. Clin Sports Med 22:255–275
Bossart PJ, Joyce SM, Manaster BJ et al (1988) Lack of efficacy of ”weighted” radiographs in diagnosing acute acromioclavicular separation. Ann Emerg Med 17:20–24
Vanarthos WJ, Ekman EF, Bohrer SP (1994) Radiographic diagnosis of acromioclavicular joint separation without weight bearing: importance of internal rotation of the arm. Am J Roentgenol 162:120–122
Beim GM (2000) Acromioclavicular joint injuries. J Athl Train 35:261–267
Sluming VA (1995) A comparison of the methods of distraction for stress examination of the acromioclavicular joint. Br J Radiol 68:1181–4
Vaatainen U, Pirinen A, Makela A (1991) Radiological evaluation of the acromioclavicular joint. Skeletal Radiol 20:115–116
Tossy JD, Mead MC, Sigmond HM (1963) AC separations: useful and practical classification for treatment. Clin Orthop Relat Res 28:111–119
Allman FL Jr (1967) Fractures and ligamentous injuries of the clavicle and its articulation. J Bone Joint Surg Am 49:774–784
Williams GR Jr, Nguyen VD, Rockwood CA Jr (1989) Classification and radiographic analysis of acromioclavicular dislocations. Appl Radiol 18:29–34
Lemos MJ (1998) The evaluation and treatment of the injured acromioclavicular joint in athletes. Am J Sports Med 26:137–144
Alyas F, Curtis M, Speed C et al (2008) MR imaging appearances of the acromioclavicular joint dislocation. Radiographics 28:463–479
Banerjee R, Waterman B, Padalecki J et al (2011) Management of distal clavicle fractures. J Am Acad Orthop Surg 19:392–401
Fraser-Moodie JA, Shortt NL, Robinson CM (2008) Injuries to the acromioclavicular joint. J Bone Joint Surg Br 90-B:697–707
Scapinelli R (2004) Bipolar dislocation of the clavicle: 3D CT imaging and delayed surgical correction of a case. Arch Orthop Trauma Surg 124:421–424
Artingar E, Holzman M, Gunther S (2001) Bipolar clavicular dislocation. Orthopedics 34:e316–319
Cote MP, Wojcik KE, Gomlinski G, Mazzocca AD (2010) Rehabilitation of acromioclavicular separations: operative and nonoperative considerations. Clin Sports Med 29:213–228
Gladstone J, Wilk K, Andrews J (1997) Nonoperative treatment of acromioclavicular injuries. Oper Tech Sports Med 5:78–87
Bjerneld H, Hovelius L, Thorling J (1983) Acromio-clavicular separations treated conservatively: a 5-year follow-up study. Acta Orthop Scand 54:743–745
Lervick GN (2005) Direct arthroscopic distal clavicle resection: a technical review. Iowa Orthop J 25:149–156
Ponce BA, Millett PJ, Warner JJP (2004) Acromioclavicular joint instability—reconstruction indications and techniques. Operative Techniques in Sports Medicine 12:35–42
Spencer EE Jr (2007) Treatment of grade III acromioclavicular joint injuries: a systematic review. Clin Orthop Relat Res 455:38–44
Smith TO, Chester R, Pearse EO et al (2011) Operative versus non-operative management following Rockwood grade III acromioclavicular separation: a meta-analysis of the current evidence base. J Orthop Traumatol 12:19–27
Norrell H Jr, Llewellyn RC (1965) Migration of a threaded Steinmann pin from an acromioclavicular joint into the spinal canal: a case report. J Bone Joint Surg Am 47:1024–1026
Sethi GK, Scott SM (1976) Subclavian artery laceration due to migration of a Hagie pin. Surgery 80:644–646
Sim E, Schwarz N, Hocker K et al (1995) Repair of complete acromioclavicular separations using the acromioclavicular-hook plate. Clin Orthop Relat Res 314:134–142
Liu HH, Chou YJ, Chen CH et al (2010) Surgical treatment of acute acromioclavicular joint injuries using a modified Weaver–Dunn procedure and clavicular hook plate. Orthopedics 33:552
Laprade RF, Wickum DJ, Griffith CJ, Ludewig PM (2008) Kinematic evaluation of the modified Weaver–Dunn acromioclavicular joint reconstruction. Am J Sports Med 36:2216–2221
Tauber M, Gordon K, Koller H, Fox M, Resch H (2009) Semitendinosus tendon graft versus a modified Weaver–Dunn procedure for acromioclavicular joint reconstruction in chronic cases: a prospective comparative study. Am J Sports Med 37:181–190
Weaver JK, Dunn HK (1972) Treatment of acromioclavicular injuries, especially complete acromioclavicular separation. J Bone Joint Surg Am 54:1187–1194
Snyder SJ, Banas MP, Karzel RP (1995) The arthroscopic Mumford procedure: an analysis of results. Arthroscopy 11:157–164
Stine IA, Vangsness CT Jr (2009) Analysis of the capsule and ligament insertions about the acromioclavicular joint: a cadaveric study. Arthroscopy 25:968–74
Struhl S (2007) Double endobutton technique for repair of complete acromioclavicular joint dislocations. Techniques in Shoulder and Elbow Surgery 4:175–179
Strauss EJ, Barker JU, McGill K et al (2010) The evaluation and management of failed distal clavicle excision. Sports Med Arthrosc Rev 18:213–219
Thiel E, Mutnal A, Gilot G (2011) Surgical outcome following arthroscopic fixation of acromioclavicular joint disruption with the TightRope device. Orthopedics 34:267
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, A.C., Matcuk, G., Patel, D. et al. Acromioclavicular joint injuries and reconstructions: a review of expected imaging findings and potential complications. Emerg Radiol 19, 399–413 (2012). https://doi.org/10.1007/s10140-012-1053-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-012-1053-0