Abstract
Abdominal aortic injuries are uncommon following blunt trauma, with relatively few reported series in the radiology literature. This study was conducted to identify common locations and imaging features of blunt traumatic abdominal aortic injury, the presence of associated visceral and osseous injuries, and the mechanisms of trauma. A retrospective review of 9,213 trauma registry entries over a 7-year period yielded 103 patients with aortic injuries, 12 of which had direct signs of abdominal segment involvement (dissection flap, focal intimal injury, intramural hematoma, active extravasation of contrast, or pseudoaneurysm formation). The majority (75 %) was isolated to the abdomen—67 % of which was infrarenal, 33 % suprarenal—while the other 25 % was a contiguous extension from a thoracic injury. Abdominal aortic injuries were uncommonly seen in isolation: all but one patient (92 %) demonstrated either retroperitoneal blood or stranding, hemoperitoneum, and/or CT signs of hypoperfusion complex, and only one patient (8 %) had no associated solid organ or skeletal injuries. All patients had a mechanism of injury which involved direct trauma to the abdomen, most commonly a motor vehicle collision. Similar to other recent series, there was an increased rate of abdominal segment injury (11.7 % of all aortic injuries) in this series compared to more remote autopsy series. This difference is likely due to detection of injuries which went undiagnosed before the widespread use of multidetector CT, which has become the standard of care for both acute evaluation following blunt trauma and for follow-up.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Traumatic aortic injury following blunt (nonpenetrating) trauma is a rare but potentially lethal injury. Large autopsy series have reported that aortic injuries occur in approximately 1 % of patients suffering blunt trauma [1, 2]. Aortic injuries involving the abdominal segment are even less common following blunt trauma, with only a few reported series in the radiology literature. Abdominal aortic injuries were seen in about 4–5 % of all aortic injuries in older autopsy series [1, 3]. More recent series have shown the incidence of abdominal aortic injuries to be higher than previously reported, ranging from 12 to 15 % [4, 5]. However, the multidetector CT (MDCT) features of acute abdominal aortic injury are well documented, likely due to the relative rarity of this injury.
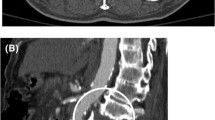
In contrast, the imaging features of traumatic injury to the proximal descending thoracic aorta have been well described, as this is the most common site of aortic injury in blunt trauma, largely due to the fixed nature of the aorta at the isthmus [6, 7] (Fig. 1). MDCT is now the preferred modality to evaluate the trauma patient, due to its availability, rapid acquisition of images with a single contrast bolus, and ability to scan multiple body parts [8, 9]. As contrast-enhanced CT has become the standard method of evaluating these patients; multiple direct and indirect CT features of aortic injury have been described with acute traumatic aortic injury within the thorax, including dissection flap, intramural hematoma, eccentric thrombus, active extravasation of contrast, and pseudoaneurysm formation [6]. With these thoracic aortic injury patterns in mind, the purpose of this paper is to review the MDCT features of abdominal aortic injury in a small series, document the common locations of these injuries, and detail the presence of associated injuries and the mechanisms of trauma.
Transverse CT image a of acute traumatic aortic injury in the most common location—the aortic isthmus—demonstrating an intimal dissection flap (black arrowheads), pseudoaneurysm formation (white dotted arrow), and periaortic hematoma (white arrowheads). b Caudal extension of the dissection flap into the abdominal aorta (black arrowhead). Note also the lumbar vertebral body fracture as well (white arrow)
Methods
After formal application, investigational review board exemption was approved by the Washington University Human Research Protection Office. A retrospective query of the trauma registry was performed for CT imaging of aortic injury over a 7-year period (1 January 2002 to 24 March 2009), for both thoracic and abdominal aortic injuries. Query of the registry yielded at total of 9,213 patients who were admitted for or died from nonpenetrating trauma. A total of 103 patients with aortic injury were identified in the registry for review.
Each case was reexamined by three separate board-certified radiologists—one junior abdominal radiologist, one senior chest radiologist, and one senior abdominal radiologist; the senior radiologists each had 10 years experience reading body CT with a focus on emergency radiology. The images were anonymized, and the readers were blinded to the original CT interpretation. Three radiologists were used to address interreader variability, since many of the patients encountered did not undergo aortography to confirm aortic injury, making MDCT the gold standard exam in this study. Initial interpretations were performed independently, and discrepancies between the reads were addressed by conferring and deciding on consensus collectively. All patients in the study were evaluated on either 16 or 40 row MDCT (Sensation, Siemens Medical, Erlangen, Germany), using a routine trauma protocol that consists of contrast-enhanced images only. Given the range of dates included in the study, the slice thickness varied from 0.6 to 1.5 mm. Interpretation of the cases was primarily performed with the axial images with employment of a 3D workstation as needed.
Only cases with contiguous aortic injury involving both the thoracic and abdominal segments, injury isolated to the abdominal aorta, or separate but concomitant abdominal and thoracic aortic injuries were included. Injuries which concomitantly involved the thoracic aorta were included to help determine the incidence of isolated abdominal aortic injury. The patients’ electronic medical records were reviewed as well to discern the circumstances and mechanism of injury.
The MDCT imaging features of each aortic injury were then recorded. The abdominal aorta was separated into segments. The suprarenal aorta was defined as including both the perihiatal segment extending from the diaphragmatic hiatus to the celiac axis as well as the juxtarenal segment from the celiac axis to the renal arteries. The infrarenal segment was defined as extending from the renal arteries to the iliac bifurcation. A total of 12 patients were selected based on the presence of direct signs of abdominal aortic injury, including presence of a large intraluminal flap, a focal intimal injury (defined as intraluminal tear or thrombus less than 1 cm in diameter without external aortic contour abnormality), intramural hematoma, pseudoaneurysm formation, or active extravasation of contrast material. Each reader was oriented as to the definition of various aortic injury findings to help improve interreader consistency. Indirect findings were also assessed, including the presence of retroperitoneal hematoma as well as surrounding retroperitoneal or mesenteric fat stranding. MDCT features of shock were also documented, including hyperenhancing bowel, hyperenhancement of the adrenals and kidneys, and/or slit-like inferior vena cava [10]. The presence and frequency of associated injuries involving the liver, spleen, kidney, bowel, mesentery, and bones were evaluated and documented as well.
Results
Location of injury
A total of 25 % (3 out of 12) of the patients had injuries to both the thoracic and abdominal aorta. In all cases, these injuries were contiguous (Table 1; Fig. 2). The other 75 % (9 out of 12) had isolated injuries to the abdominal aorta. The location of isolated abdominal aortic injury varied, with isolated infrarenal injuries seen most commonly, comprising 67 % (six out of nine) of isolated abdominal aortic injuries. Only one patient (11 %, one out of nine) with isolated abdominal aortic injury had an injury confined to the juxtarenal segment. The remainder of isolated abdominal injuries occurred around the diaphragmatic hiatus: 22 % (two out of nine) of injuries were seen in the perihiatal region, extending from the level of T7 to the celiac axis.
Direct findings
Direct signs of abdominal aortic injury include the presence of a large intraluminal flap, intramural hematoma, focal intimal injury, pseudoaneurysm formation, or active extravasation of contrast material (Figs. 3 and 4). A large intimal flap was noted in 83.3 % (10 out of 12) of patients (Fig. 3); the remaining 16.7 % (2 out of 12) of patients all had a focal intimal injury without a large flap (Fig. 4). Intramural hematoma was noted in 33 % (4 out of 12) of cases, and was never seen in the absence of an intraluminal flap or focal intimal injury. Only one case (8 %) demonstrated pseudoaneurysm formation (Fig. 5). Active extravasation of contrast material was seen only in cases with an associated thoracic aortic injury (3 out of 12) and was always located in the descending thoracic aorta; no active extravasation of contrast material was noted from an isolated abdominal aortic injury.
Indirect findings
Indirect findings of abdominal aortic injury include the presence of retroperitoneal hematoma as well as surrounding retroperitoneal or mesenteric stranding. The most common indirect finding seen was either stranding or hematoma within the retroperitoneum, seen in 58 % (7 out of 12) of cases (Figs. 3 and 4). MDCT features of hypoperfusion complex or shock, including hyperenhancing bowel, hyperenhancement of the adrenals and kidneys, and/or slit-like inferior vena cava, were seen in 25 % (3 out of 12) of cases (Fig. 6).
Transverse CT images demonstrate mucosal hyperenhancement within multiple loops of small bowel (a, arrowheads), consistent with hypoperfusion complex, which also manifested with a slit-like inferior vena cava (b, white arrowhead) in this patient with a focal suprarenal dissection flap (b, black arrowhead)
Concomitant injuries
Many patients in this study had other serious injuries including pneumothorax, visceral laceration, bowel injury, and fractures. Sixty-seven percent (9 out of 12) of cases had at least one concomitant solid organ (liver, spleen, or kidney) or bowel/mesenteric injury (Fig. 7). The liver was the most commonly injured organ seen in the setting of abdominal aortic injury, noted in 42 % (5 out of 12) of cases. Simultaneous osseous injuries were very common, seen in 83 % (10 out of 12) of cases, varying in severity and predominantly involving the spine, pelvis, and ribs.
Mechanisms of injury
A number of mechanisms were identified, ranging from driver or passenger motor vehicle collision (MVC) (58 %, 7 out of 12) to motorcycle accident, fall from height, or pedestrian struck by automobile. One patient suffered an abdominal crush injury. The common factor in all reviewed patients was severe, nonpenetrating abdominal trauma. No clear connection was found between the mechanism of injury and presence or absence of concomitant injuries. One patient without any additional intra-abdominal or osseous injuries suffered a motor vehicle collision. Another patient who had no osseous injuries suffered a severe crush injury to the abdomen (patient crushed between a truck and a dolly).
Discussion
Aortic injury is a known complication of severe blunt trauma, the frequency of which was largely reaffirmed by our study: of the 9,213 patients who presented after nonpenetrating trauma during the period we studied, 1.1 % (103 total) had aortic injuries. Direct comparison to various autopsy series for incidence of all aortic injuries following blunt trauma is difficult due to varying patient cohorts, but aortic injuries have been shown to occur in approximately 1 % of all autopsy patients in one study [3]. Similarly, a large study of Vietnam War veteran medical records revealed a 1 % incidence of aortic injuries [2]. A more recent large series in the literature showed an incidence of 0.67 % of all blunt trauma patients [4]. These data seem to indicate a relatively stable incidence of aortic injury among trauma patients, though the patient populations in these studies are obviously disparate.
The number of all abdominal segment injuries represents 0.13 % (12 out of 9,213) of all blunt trauma patients in this study. Isolated abdominal aortic injuries were even less common, occurring in 0.097 % of all blunt trauma patients. This incidence is higher than reported in a similar series in the surgical literature, which reported a 0.05 % incidence of abdominal aortic injury in blunt trauma patients [11]. Our study also showed abdominal segment injuries in 11.6 % of all aortic injuries encountered. Isolated abdominal aortic injuries were less common, seen in 8.7 % of all aortic injuries. Comparatively, a recent series in the vascular literature showed that abdominal segment injuries occurred in 12.1 % of all aortic injuries [5]. Another relatively recent series showed abdominal aortic injuries in approximately 15 % of all aortic injuries [4]. Both our study and these recent series show that the fraction of all aortic injuries involving the abdominal segment is higher than in two landmark autopsy series which both showed abdominal aortic injuries to occur in approximately 4.2–4.7 % of all aortic injuries [1, 3]. These differences in reported incidence are likely a result of discovering injuries which may have had no immediate clinical manifestations, previously undetected prior to the use of MDCT. As evidence supporting the clinically occult nature of some subtle aortic injuries, delayed diagnosis has been reported in up to 34.3 % of patients [12]. Detection of subtle injuries on MDCT continues to improve as multidetector arrays allowing rapid acquisition of thinly collimated images and multiplanar reconstruction have become standard of care [6, 8].
The infrarenal segment was shown to be the most common site of isolated abdominal aortic injury in this study, which supports data found in other studies performed before the widespread use of CT [13]. However, suprarenal injuries were seen in greater frequency in our study (33 %) than previously described in the surgical literature, in which approximately 7 % of abdominal aortic injuries were suprarenal in position [13]. Larger autopsy series in the past have not listed the frequency of injury to various subsegments of the abdominal aorta. Again, though comparative data are limited, it is possible that some suprarenal injuries such as those seen in our study previously went undiagnosed, explaining the difference in injury distribution.
Direct findings of abdominal aortic injury similar to those seen in the thorax were criteria for inclusion of patients in this study, and therefore, all patients had either a frank intimal flap or a focal intimal injury. A slight majority (58 %) of patients also demonstrated adjacent stranding or hematoma within the retroperitoneum. However, all but one patient (92 %) demonstrated either retroperitoneal blood or stranding, hemoperitoneum, and/or MDCT features of shock. Similarly, only one patient (8 %) demonstrated no associated solid organ or skeletal injuries. These data indicate that abdominal aortic injury is uncommonly seen in isolation, that is, without other injuries, evidence of intra-abdominal bleeding, or MDCT evidence of hypoperfusion complex. Given the frequent association of abdominal aortic injury and other solid organ and osseous injuries in our study, it is particularly important to include the abdominal aorta in a CT search pattern in patients with severe traumatic injuries. Close inspection of the aorta is particularly important in patients with atherosclerosis, hypertension, or Marfan’s disease, as the intima tears more easily in patients with these conditions [13–15].
This study is limited by the small sample size of 12 patients, but this attests to the relative rarity of this injury pattern. The discrepancy between the rate of thoracic and abdominal aortic injuries likely arises from the difference in mobility of the respective segments [13]. As the abdominal aortic segment is fixed in position, injury to the aorta below the diaphragm seems to arise more commonly from direct abdominal trauma rather than deceleration injury as is often the cause in the thorax [13, 16, 17]. It has been postulated that in the setting of motor vehicle collision, a crushing force between the steering wheel or seat belt and the lumbar spine is more likely the cause of an abdominal aortic injury rather than deceleration [13]. Data from this study support this mechanism as well, given that all nonmotor vehicle collision injuries had some sort of direct abdominal trauma.
While previously all patients with traumatic abdominal aortic injury were repaired surgically, the management of certain subtypes of aortic injuries, such as focal or “minimal” intimal injury, continues to evolve, and currently includes endovascular therapy and/or watchful waiting with antiplatelet therapy, depending on the patient’s clinical status, operative risk, and/or presence of other injuries which warrant more immediate surgical intervention [5]. In fact, a recent large series of aortic injuries in the vascular literature has proposed management of focal intimal injuries with blood pressure control and aspirin, an approach supported by the positive outcomes in that study [5]. Due to the risk of distal embolization, pseudoaneurysm formation, thrombosis, and/or aortic rupture, patients with minimal intimal injury should have a short-term follow-up CT as treatment for these injuries continues to evolve [5, 18].
Conclusion
In conclusion, although rare, abdominal aortic injury does occur following nonpenetrating trauma and may be more common than previously described in autopsy series. The injury pattern appears to arise from a direct blow to the abdomen rather than a deceleration injury based on this and other studies. The direct and indirect MDCT signs of abdominal aortic injury are similar to those described in the thorax, and are uncommonly seen in isolation. Close attention to the entire aorta is warranted in the setting of blunt trauma, particularly as this series showed a fairly wide variety of locations involved in injury, although the infrarenal segment is the most common location of injury. As minimally invasive surgical techniques and possibly conservative observation have emerged as alternatives to immediate surgical repair for abdominal aortic injuries, MDCT is not only a valuable diagnostic tool but also a means for follow-up for these types of injuries to guide management in patients.
References
Parmley LF, Mattingly TW, Manion WC et al (1958) Nonpenetrating traumatic injury of the aorta. Circulation 17:1086–1101
Billy LJ, Amato JJ, Rich NM (1971) Aortic injuries in Vietnam. Surgery 70:385–391
Strassman G (1947) Traumatic rupture of the aorta. Am Heart J 33:508
Michaels A, Gerndt S, Taheri P et al (1996) Blunt force injury of the abdominal aorta. J Trauma 41(1):105–109
Starnes BW, Lundgren RS, Gunn M et al (2012) A new classification scheme for treating blunt aortic injury. J Vasc Surg 55(1):47–54
Creasy JD, Chiles C, Routh WD et al (1997) Overview of traumatic injury of the thoracic aorta. Radiographics 17(1):24–75
Steenburg S, Ravenel J (2007) Multi-detector computed tomography findings of atypical blunt traumatic aortic injuries: a pictorial review. Emerg Radiol 14:143–150
Neschis D et al (2008) Blunt aortic injury. NEJM 359:1708–1716
Gavant M et al (1996) CT aortography of thoracic aortic rupture. Am J Roentgenol 166(4):955–961
Prasad KR, Kumar A, Gamanagatti S et al (2011) CT in post-traumatic hypoperfusion complex—a pictorial review. Emerg Radiol 18(2):139–143
Brathwaite CM, Rodriguez A (1992) Injuries of the abdominal aorta from blunt trauma. Am Surg 58:350
Solovei G, Alame A, Bardoux J et al (1994) Paraplegia and dissection of the abdominal aorta after closed trauma. A propos of a case. Current review of the literature (1982–1993). J Chir (Paris) 131:236–244
Lassonde J, Laurendeau F (1981) Blunt injury of the abdominal aorta. Ann Surg 194(6):745–748
Clark JC, Milroy CM (2000) Injuries and deaths of pedestrians. In: Mason JK, Purdue BN (eds) The pathology of trauma, 3rd edn. Arnold, London, pp 17–29
Marti M, Pinilla I, Braudraxler F (2006) A case of abdominal aortic dissection caused by blunt trauma. Emerg Radiol 12:182–185
Ricen E, Dickens PF (1942) Traumatic aneurysm of the abdominal aorta of 27 years duration. US Naval Med Bull 40:692–694
Roth S et al (1997) Blunt injury of the abdominal aorta: a review. J Trauma 42(4):748–755
Halkos ME, Nicholas J, Kong LS et al (2006) Endovascular management of blunt abdominal aortic injury. Vascular 14(4):223–226
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mellnick, V.M., McDowell, C., Lubner, M. et al. CT features of blunt abdominal aortic injury. Emerg Radiol 19, 301–307 (2012). https://doi.org/10.1007/s10140-012-1030-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-012-1030-7