Abstract
Multidetector computed tomography (MDCT) cystography is rapidly becoming the most recommended study for evaluation of the bladder for suspected trauma. This article reviews the bladder trauma with emphasis on the application of MDCT cystography to traumatic bladder injuries using a pictorial essay based on images collected in our level I trauma center.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Bladder anatomy
The urinary bladder is a hollow muscular organ located deep in the pelvis in adults and in the lower abdomen in children. The bladder is separated from the pubic symphysis by a potential prevesical space known as the space of Retzius (Figs. 1 and 2). The pubovesical, medial, and paired lateral umbilical ligaments strengthen the association of the bladder with the anterior pelvic wall. The bladder neck is contiguous with the prostate in males and it is attached to the pubis by the puboprostatic ligaments (Fig. 2). The pubourethral ligaments support the bladder neck and urethra in females (Fig. 1). The bladder dome is covered superiorly by the extraperitoneal fat and peritoneal reflections. The bladder is supported inferiorly by the urogenital diaphragm and laterally by the obturator internus muscles.
The type of urinary leakage, either intraperitoneal or extraperitoneal, depends upon the location of the injury in relation to the peritoneal reflections. If the rupture occurs above the peritoneal reflections, the leakage is intraperitoneal. If the injury occurs below the peritoneal reflections, the leakage is extraperitoneal. Urinary leakage may be combined, intraperitoneal and extraperitoneal, if the rupture occurs directly at the level of peritoneal reflections.
Classification and mechanisms of bladder trauma
Trauma to the genitourinary system occurs in approximately 5–10% of all patients with trauma. Most of these injuries are secondary to blunt trauma, and approximately 10% of genitourinary injuries result in bladder trauma. Bladder injuries occur in 1.6% of blunt abdominal trauma cases [1]. Bladder rupture occurs in 2–11% of patients with pelvic fractures. However, 60–90% of patients with bladder rupture have a pelvic fracture [2, 3].
Bladder trauma may arise from a variety of mechanisms divided into blunt trauma 60–85%, penetrating trauma 15–40%, and iatrogenic injury 5% (cystoscopy, laparoscopy, abdominal, and vaginal surgery).
Penetrating injury is often secondary to impaling objects, missiles, or stab wounds. In penetrating traumas, the most frequent causes are: gunshot wounds (85%) and stabbings (15%).The penetrating bladder injuries occur in 3.6% of abdominal gunshot wounds, 13% of penetrating injuries to the rectum and 20% of penetrating injuries to the buttock [3].
Blunt pelvic trauma secondary to motor vehicle accidents accounts for between 70% and 90% of cases [4]. The most common mechanisms of blunt trauma are: motor vehicle accidents (70–90%), falls (5–15%), and assaults (5–10%).
Five types of bladder injuries seen with conventional cystography were described by Sandler et al. [5].
Type I | Type II | Type III | Type IV | Type V |
|---|---|---|---|---|
Contusion | Intraperitoneal | Interstitial or bladder wall hematoma | Extraperitoneal | Combined |
IVa: Simple | ||||
IVb: Complex |
Extraperitoneal bladder rupture is the most common type occurring in 70–80% whereas intraperitoneal and combined bladder ruptures occurs in 15–20% and 5–10% of patients, respectively [6].
Blunt injury to the urinary bladder usually results either from an impact to the lower abdomen when the bladder is distended, or when there is associated pelvic fracture with loss of protective effect of the pelvic ring and disruption of the bladder at its fascial attachments. A bony spicule may also lacerate directly the bladder.
Bladder contusion is an intramural injury resulting from damage to the bladder mucosa or muscularis without full-thickness disruption of wall continuity.
Interstitial bladder rupture is an intramural or partial thickness injury of the bladder wall without complete perforation. In this type of rupture, the serosa is intact. This results in an irregularity in the bladder wall on multidetector computed tomography (MDCT) cystography, but without frank leakage of contrast material outside the bladder.
Extraperitoneal bladder rupture is usually the result of penetrating trauma, but in cases of blunt trauma it is believed to be secondary to direct laceration of the bladder by adjacent bone fragments. The mechanism of traumatic extraperitoneal ruptures was considered to be from a direct perforation by a bony fragment from the fractured pelvis. However, the pelvic fracture is likely coincidental and the bladder rupture can also result from direct shearing. These ruptures are usually associated with fractures of the anterior pubic arch and the anterolateral aspect of the bladder can be perforated by bony spicules. The classic cystographic finding is contrast leakage around the base of the bladder confined to the perivesical space. The contrast material may extend to the thigh, perineum, and scrotum or into the anterior abdominal wall with a more complex injury.
The location of extraperitoneal injury is most commonly at the bladder base. A blow directed to the inferior portion of the bladder, often associated with pelvic fractures, can result in rupture of the bladder into the extraperitoneal space. Traumatic extraperitoneal ruptures usually are associated with pelvic fractures (89–100%).
Intraperitoneal bladder rupture is less common than extraperitoneal bladder rupture. Delayed diagnosis of intraperitoneal bladder rupture results in an increased mortality. It has the highest morbidity and mortality due to the risk of chemical peritonitis and requires operative management. The mechanism of traumatic intraperitoneal ruptures is a sudden large increase in intravesical pressure in a full bladder when the bladder dome fibers are widely separated with little resistance to sudden changes in intravesical pressure. The risk of bladder rupture rises proportionally to the extent of bladder filling at the time of injury [7].
Intraperitoneal bladder ruptures are believed to occur more frequently in small children undergoing motor vehicular accidents than adults as the seat belt fits over the anterior lower abdomen rather than the superior iliac spines and the bladder is positioned in the lower abdomen rather than deep in the pelvis [3].
Combined intraperitoneal and extraperitoneal ruptures account for approximately 5–10% of all traumatic bladder-perforating injuries. The diagnosis of combined intraperitoneal and extraperitoneal rupture may be missed if the rupture site is large to the extent that full bladder distention cannot be achieved, and most of the contrast agent leaks into the extraperitoneal compartment but not into the intraperitoneal one [8].
MDCT appearance of bladder trauma
While bladder injuries will frequently be seen on standard CT with intravenous contrast bolus and a clamped bladder catheter, this antegrade approach to bladder distension cannot reliably exclude bladder injury [9]. MDCT cystography is indicated if bladder rupture is suspected especially when blood is seen clinically in the meatus or pelvic fracture is seen on conventional abdominal trauma MDCT. In the absence of pelvic fluid, especially if only microscopic hematuria is present, MDCT cystography may be avoided [10]. The presence of fluid, however, is not as strong a positive predictor because hematoma can result from orthopedic injury alone. MDCT cystography should be done when pelvic fluid is present, especially when there are fractures or gross hematuria, to define which of the patients has a bladder rupture and to define the type of bladder rupture [10].
Compared to helical CT, MDCT improves temporal and spatial resolution, decreases image noise and provides longer anatomic coverage. The thin-section scanning in MDCT allows the production of higher quality multiplanar reformation (MPR) images [11]. MPR images provide better anatomic delineation. Sagittal and coronal multiplanar reformations may be helpful in identifying most sites of bladder rupture, especially in visualizing intraperitoneal rupture where the bladder dome which is parallel to the scanning plane of the axial scan (Figs. 3 and 4). Coronal MPR reformatted images constitute a helpful asset to surgeons because the orientation of structures is similar to that seen during exploratory laparotomy Fig. 5.
Intraperitoneal bladder rupture: sagittal reformatted image from MDCT cystography demonstrates rupture through dome of bladder with leakage of contrast between bowel loops. Intraperitoneal leakage of contrast identified outlining the uterus. The green arrow depicts the site of bladder dome disruption
MDCT cystography is performed after assessment and appropriate management of urethral injury, due to the high incidence of concomitant urethral injury [12]. Diagnosis is made with either direct instillation of contrast medium (350–400 ml) into the bladder via a urethral or suprapubic catheter. CT cystography is accurate as conventional cystogram in diagnosing bladder trauma [9, 13–15]. MDCT cystography is 95% sensitive and 99% specific in detecting overall bladder rupture [13]. To reliably diagnose bladder injury, sufficient distension must be obtained to initiate detrusor muscle contraction. A normal MDCT cystogram finding does not exclude entirely a bladder rupture due to spasm of the detrusor muscle, which is possibly secondary to the irritation effect of the contrast medium causing a leak to become sealed. With general anesthesia, the detrusor relaxes and therefore the eventual intraoperative leakage can be seen.
MDCT cystography is applied to a classification scheme for bladder injury based on the degree of wall injury and anatomic location with demonstrating characteristic imaging features for each type of injury [14].
In bladder contusion (type I), findings at conventional and MDCT cystography are normal. Manifestations of interstitial injury (type III) include intramural hemorrhage and submucosal extravasation of contrast material without transmural extension. Interstitial bladder rupture results in an irregularity in the bladder wall on MDCT cystography, but without frank extravesical leakage of contrast Fig. 6.
In intraperitoneal rupture (type II), MDCT cystography demonstrates intraperitoneal contrast material around bowel loops, between mesenteric folds, and in the paracolic gutters (Fig. 7).
a Intraperitoneal bladder rupture: axial MDCT cystography shows rupture of bladder with intraperitoneal leakage of contrast between bowel loops (green arrow). Note large filling defect within bladder, compatible with clot. b Intraperitoneal bladder rupture: coronal reformatted image from MDCT cystography shows rupture of the bladder with intraperitoneal leakage of contrast between bowel loops (green arrow). There is a large filling defect within the bladder, compatible with clot. c Intraperitoneal bladder rupture: sagittal reformatted image from MDCT cystography demonstrates rupture through the dome of the bladder (green arrow) with intraperitoneal leakage of contrast between bowel loops (red arrow)
In extraperitoneal rupture (type IV), the pathway of extravasated contrast material is variable: extravasation is confined to the perivesical space in simple extraperitoneal ruptures (type IVa), Fig. 8, whereas in complex extraperitoneal ruptures, Fig. 9, contrast material extends beyond the perivesical space and may dissect into a variety of fascial planes and spaces (type IVb).
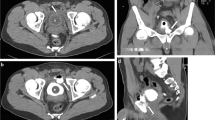
a Extraperitoneal simple bladder rupture: axial MDCT cystography shows contrast leakage confined to perivesical space (green arrow). b Extraperitoneal simple bladder rupture: coronal MDCT cystography shows left pubic ramus fracture (red arrow) with contrast in perivesical space: (green arrow). c Extraperitoneal simple rupture: Sagittal MDCT cystography shows bladder rupture at bladder base (green arrow). Note left pubic ramus fracture (red arrow)
a Extraperitoneal complex bladder rupture: axial MDCT retrograde cystography shows leakage of contrast into perivesical space extending into fascial planes of right abdominal walls (green arrows). b Extraperitoneal complex bladder rupture: axial MDCT retrograde cystography shows leakage of contrast into perivesical space extending into fascial planes of anterior abdominal wall (green arrow), perineum (red arrow), and soft tissues of upper thigh (blue arrow). Pelvic fracture is seen (yellow arrow)
Free contrast-enhanced urine pooling in the paravesical spaces has been described as having a “molar tooth” appearance on axial MDCT (Fig. 10). Combined intra- and extraperitoneal rupture (type V) usually demonstrates extravasation patterns that are typical for both types of injury (Fig. 11).
a Extraperitoneal bladder rupture: axial MDCT cystography shows leakage of contrast into perivesical space creating “molar tooth” appearance (green arrows). Note comminuted fracture of right iliac bone (blue arrow). b Extraperitoneal bladder rupture: Axial MDCT cystography shows leakage of contrast into perivesical space (green arrows) associated with comminuted fracture of right iliac bone extending to the acetabulum (blue arrows)
a Combined bladder rupture: axial MDCT cystography demonstrates rupture in the left lateral bladder wall with leakage of contrast into the perivesical space (blue arrow) creating the molar tooth appearance (yellow arrow). Note contrast extension into the fascial planes of the anterior abdominal wall (green arrow). The more cranial image demonstrates contrast in the peritoneal space outlining bowel loops (red arrow). b Combined bladder rupture: coronal MDCT cystography demonstrates rupture in the left lateral bladder wall with leakage of contrast into the perivesical space (yellow arrows) extending intraperitoneally around intestinal loops (green arrows) and extraperitoneally (red arrows) though multiple pelvic fractures (blue arrows)
Leakage of opacified urine into the posterior fornix of the vagina can mimic intraperitoneal bladder rupture. Familiarity with these MDCT cystographic features allows accurate classification of bladder injury and allows prompt, effective treatment with less radiation exposure than and without the added cost of conventional cystography [14].
Conclusion
Rapid diagnosis and accurate identification of bladder injury are crucial for optimal patient management and in decreasing patient morbidity and mortality [14]. Knowledge of the mechanisms, classifications, and imaging features of bladder trauma assist the clinician in clinical decision making and promote improved patient outcomes. Immediate MDCT cystography is required in the presence of free fluid, hematuria, and pelvic fracture.
References
Udekwu PO, Gurkin B, Oller DW (1996) The use of computed tomography in blunt abdominal injuries. Am Surg 62:56–59
Cass AS (1989) Diagnostic studies in bladder rupture: indication and technique. Urol Clin North Am 16:267–273
Gomez RG, Ceballos L, Coburn M et al (2004) Consensus statement on bladder injuries. BJU Int 94:27–32
Corriere JN Jr, Sandler CM (1999) Bladder rupture from external trauma: diagnosis and management. World J Urol 17:84–89
Sandler CM, Goldman SM, Kawashima A (1998) Lower urinary tract trauma. World J Urol 16:69–75
Novelline RA, Rhea JT, Bell T (1999) Helical CT of abdominal trauma. Radiol Clin North Am 37:591–612
Lynch TH, Martinez-Pineiro L, Plas E et al (2005) European Association of Urology: guidelines on urological trauma. Eur Urol 47:1–15
Power N, Ryan S, Hamilton P (2004) Computed tomography in bladder trauma: pictorial essay. Can Assoc Radiol J 55:304–308
Peng MY, Parisky YP, Cornwell E, Radin R, Bragin S (1999) CT cystography versus conventional cystography in evaluation of bladder injury. AJR 173:1269–1272
Morgan DE, Nallamala LK, Kenney PJ, Mayo MS, Rue LW 3rd (2000) CT cystography: radiographic and clinical predictors of bladder rupture. AJR 174:89–95
Rydberg J, Buckwalter K, Caldemeyer KS et al (2000) Multisection CT: scanning techniques and clinical applications. RadioGraphics 20:1787–1806
Koraitim MM, Marzouk ME, Atta MA et al (1996) Risk factors and mechanisms of urethral injury in pelvic fractures. Br J Urol 77:876–880
Chan DP, Abujudeh HH, Cushing GL Jr, Novelline RA (2006) CT cystography with multiplanar reformation for suspected bladder rupture: experience in 234 cases. AJR Am J Roentgen 187(5):1296–1302
Vaccaro JP, Brody JM (2000) CT cystography in the evaluation of major bladder trauma. RadioGraphics 20:1373–1381
Quagliano PV, Delair SM, Malhotra AK (2006) Diagnosis of blunt bladder injury: a prospective comparative study of computed tomography cystography and conventional retrograde cystography. J Trauma 61(2):410–421, discussion 421–2
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 37 kb)
Rights and permissions
About this article
Cite this article
Ishak, C., Kanth, N. Bladder trauma: multidetector computed tomography cystography. Emerg Radiol 18, 321–327 (2011). https://doi.org/10.1007/s10140-011-0947-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-011-0947-6