Abstract
We report the case of a 41-year-old man who presented to the ER following a fall in his back garden during which he sustained a left orbital injury. Computed tomography (CT) demonstrated an intraorbital linear lucency surrounded by haziness in the intraconal fat. An intraocular wooden twig was confirmed during subsequent surgery. The possibility of a wooden intraorbital foreign body should be strongly suspected following orbital trauma when there is intraorbital density below that of the surrounding intraorbital fat on CT, as this may mimic organic foreign bodies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Intraorbital foreign bodies (IOFBs) are a common occurrence worldwide and happen at a frequency of once in every six cases of orbital trauma. Metallic foreign bodies are commoner than inorganic nonmetallic foreign bodies, such as glass, plastic, and rubber, as well as organic foreign bodies such as vegetables [1, 2]. Imaging and management should be tailored individually. In this report, we present the case of a 5-cm-long intraorbital wooden foreign body that appeared to simulate intraorbital air on computed tomography (CT).
Case report
A 41-year-old white man presented to the ER with painful left eye movements and diplopia—1 day after falling face-down in his back garden and sustaining left-sided orbital injury. Pertinent physical and laboratory findings include swelling with a laceration of his left lower eyelid, redness, and tenderness, as well as features of left periorbital cellulitis. Although the patient had normal fundoscopic and visual acuity tests and no evidence of corneal laceration, there were restricted left eye movements, most notably on upward gaze.
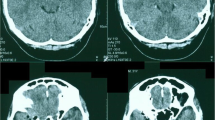
Pre- and postcontrast (hand-injected 50 ml of Niopam® 300) axial helical CT scans (Siemens SOMATOM Sensation 16) of the orbit were obtained (Figs. 1, 2, 3, 4, 5, and 6) with 0.75-mm-slice collimation. Image data were reconstructed at a slice thickness setting of 3 mm. Axial and coronal reconstructed images were viewed with soft tissue (W: 350, L: 50), bony (W: 2,500, L: 250), and lung (W: 1,500, L: −600) window settings on a 512 × 512 matrix. The scan demonstrated left-sided periorbital and orbital edema, proptosis, and a low-density linear foreign body resembling air that extended from the left lower eyelid into the intraconal retro-orbital fat infero-medially, 7 mm from the left optic nerve.
Same image as in Fig. 8, with cursor showing the HU of 462 in the center of the wooden foreign body
The patient was treated with antibiotics and analgesics, and the 5-cm-long dry twig, along with a shriveled leaf (Figs. 10 and 11), was removed under general anesthesia. His left ocular motility and cellulitis have since improved.
CT images of the extracted twig demonstrate the porous center with a density very similar to that of air (Figs. 7, 8, and 9).
Discussion
Orbital injuries occur commonly following maxillofacial trauma [3]. The severity of penetrating orbital injury is often underestimated by physical examination, and diagnosis of IOFB therefore requires high clinical suspicion and an appropriate choice of imaging modalities [4].
Wood and other organic IOFBs still present a diagnostic challenge despite improved resolution of CT scanners. The CT densities of wooden foreign bodies vary according to their porosity [5]. They may present with densities similar to that of the intraocular muscles, especially with late presentation [1], but in the acute stages, they tend to resemble bubbles of air. Dry pine has a density of −656 Hounsfield units (HU) compared with fresh pine, which has a density of −24 HU [6]. In the absence of a fracture, intraorbital air should raise the suggestion of an IOFB, particularly if the air has a linear configuration, as in our case [7].
CT is generally considered to be the gold standard for IOFBs [8]. It is safe to use with metallic IOFBs, excludes orbito-cranial extension, and is also able to diagnose orbital wall fractures and orbital sepsis with high accuracy [9, 10]. Abscess formation in the orbit, bone, and brain are other complications that CT may exclude.
Spiral CT has advantages over conventional CT due to higher quality coronal and sagittal images, reduced motion artifact, lower lens dose [11], and reduced beam-hardening artifact from metallic IOFBs [12]. CT is also accurate for the detection and localization of glass, metal, and stone foreign bodies [13], and the nature of the IOFB may be deduced from the Hounsfield numbers [14].
Metallic density is easily distinguished on CT, but size overestimation of metals on soft tissue window settings is a well-recognized occurrence [15]. The CT threshold size for the detection of metallic foreign bodies is 0.07 mm3 with thin slice CT [16]. A separate study has found steel to be the easiest IOFB to detect, followed by copper, aluminum, spectacle glass, vehicle window glass, and wood [17].
Chronic cases of wooden IOFB may become more visible with contrast enhancement due to the surrounding inflammatory reaction [1, 18], which may also contribute to the increased density of the wood along with the increased water content of the wood.
Suspected IOFB and associated injuries may also be investigated with plain radiographs, ultrasound, and magnetic resonance imaging (MRI), depending on local expertise, facilities available, and the probable constitution of the IOFB. Plain radiographs are inexpensive but underestimate plastic and wooden IOFBs. Normal structures, such as the ophthalmo-meningeal foramen, may be mistaken for IOFBs on plain radiographs [19]. Ocular ultrasound has a higher sensitivity than plain radiographs for detecting all kinds of IOFBs and is accurate for intraocular foreign bodies [13, 14]. However, it is time consuming, does not visualize the orbit completely [6], and may result in false positives, such as intraorbital air mimicking solid foreign bodies on ultrasound [20]. MRI scans should be performed when there is a high suspicion of IOFBs, especially wooden IOFBs and a negative CT scan. MRI can also distinguish between air and wood and is more helpful in cases of organic IOFBs when CT is negative [21]. MRI is, however, more expensive, less accessible, and requires pre-MRI imaging (plain radiographs and CT) to exclude metallic IOFBs in cases of orbital trauma. Treatment principles for IOFB include pain relief, broad-spectrum antibiotic cover, and surgical extraction [22, 23].
In summary, multimodality imaging can provide the required information regarding the location and type of IOFB and allows preoperative surgical planning. Radiologists should be aware that intraorbital gaseous densities might represent wooden foreign bodies, especially if given the appropriate clinical information. We recommend CT orbits for all suspected intraocular foreign bodies and MRI for negative CT scans, particularly if the suspected IOFB is organic. The use of ultrasound would depend on local expertise and availability.
References
Boncoeur-Martel MP, Adenis JP, Rulfi JY, Robert PY, Dupuy JP, Maubon A (2001) CT appearances of chronically retained wooden intraorbital foreign bodies. Neuroradiology 43(2):165–168
Fulcher TP, McNab AA, Sullivan TJ (2002) Clinical features and management of intraorbital foreign bodies. Ophthalmology 109(3):494–500
Wessberg GA, Wolford LM, Zerdecki JW, Epker BN (1981) Ophthalmologic considerations in maxillofacial trauma. Anatomy and diagnostic evaluation. Int J Oral Surg 10(4):236–246
Cartwright MJ, Kurumety UR, Frueh BR (1995) Intraorbital wood foreign body. Ophthal Plast Reconstr Surg 11(1):44–48
Ho VT, McGuckin JF, Smergel EM (1996) Intraorbital wooden foreign body: CT and MR appearance. AJNR Am J Neuroradiol 17:134–136
McGuckin JF, Akhtar N, Ho VT, Smergel EM, Kubacki EJ, Villafana T (1996) CT and MR evaluation of a wooden foreign body in an in vitro model of the orbit. AJNR Am J Neuroradiol 17:129F–133F
Green BF, Kraft SP, Carter KD, Buncic JR, Nerad JA, Armstrong D (1990) Intraorbital wood. Detection by magnetic resonance imaging. Ophthalmology 97(5):608–611
Rubinstein A, Riddell CE, Kafil-Hussain N, Assaf A (2005) Self-inserted intra-orbital foreign bodies. Ophthalm Plast Reconstr Surg 21(2):156–157
Howe L, Jones NS (2004) Guidelines for the management of periorbital cellulitis/abscess. Clin Otolaryngol 29(6):725–728
Michon J, Liu D (1994) Intraorbital foreign bodies. Semin Ophthalmol 9(3):193–199
Prokesch R, Lakits A, Scholda C, Bankier A, Ba-Ssalamah A, Imhof H (1998) Spiral CT and conventional CT in the preoperative imaging of intraocular metal foreign bodies. Radiologe 38(8):667–673
Lakits A, Steiner E, Scholda C, Kontrus M (1998) Evaluation of intraocular foreign bodies by spiral computed tomography and multiplanar reconstruction. Ophthalmology 105(2):307–312
Lakits A, Prokesch R, Scholda C, Bankier A (1999) Orbital helical computed tomography in the diagnosis and management of eye trauma. Ophthalmology 106(12):2330–2335
Lagalla R, Manfre L, Caronia A, Bencivinni F, Duranti C, Ponte F (2000) Plain film, CT and MRI sensibility in the evaluation of intraorbital foreign bodies in an in vitro model of the orbit and in pig eyes. Eur Radiol 10(8):1338–1341
Papadopoulos A, Fotinos A, Maniatis V, Kavadias S, Michaelides A, Avouri M, Kalamara C, Stringaris K (2001) Assessment of intraocular foreign bodies by helical-CT multiplanar imaging. Eur Radiol 11(8):1502–1505
Otto PM, Otto RA, Virapongse C, Friedman SM, Emerson S, Li KC, Malot R, Kaude JV, Staab EV (1992) Screening test for detection of metallic foreign objects in the orbit before magnetic resonance imaging. Invest Radiol 27(4):308–311
Tate E, Cupples H (1981) Detection of orbital foreign bodies with computed tomography: current limits. AJR Am J Roentgenol 137:493–495
Guckel C (1988) Possible computed tomographic and magnetic resonance tomographic detection of wood foreign bodies following perforating eye injuries. Radiologe 28(7):334–337
Nabili S, Ferguson AW, Gamble P, Zealley IA, MacEwen CJ (2006) The ophthalmo-meningeal foramen masquerading as an intraocular foreign body. Emerg Med J 23(7):e41
Bhavsar AR, Fong DS, Kerman B, Yoshizumi MO (1997) Intraorbital air simulating an intraocular foreign body. Am J Ophthalmol 123(6):835–837
LoBue TD, Deutsch TA, Lobick J, Turner DA (1988) Detection and localization of nonmetallic intraocular foreign bodies by magnetic resonance imaging. Arch Ophthalmol 106(2):260–261
Karcioglu ZA, Nasr AM (1998) Diagnosis and management of orbital inflammation and infections secondary to foreign bodies: a clinical review. Orbit 17(4):247–269
Ho VH, Wilson MW, Fleming JC, Haik BG (2004) Retained intraorbital metallic foreign bodies. Ophthal Plast Reconstr Surg 20(3):232–236
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Adesanya, O.O., Dawkins, D.M. Intraorbital wooden foreign body (IOFB): mimicking air on CT. Emerg Radiol 14, 45–49 (2007). https://doi.org/10.1007/s10140-007-0576-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-007-0576-2