Abstract
We examined the yield and utility of shunt series (SS) performed for suspected shunt malfunction and whether an abnormal SS lead to shunt revision when head computed tomography (CT) was normal or unchanged. We reviewed medical records for all adult emergency patients over a 34-month period with suspected shunt malfunction imaged with both SS and head CT to determine whether a shunt revision was performed contemporaneous with imaging. Nine (3.4%) abnormal SS were identified among 263 studies performed. Among the 192 cases in which CT was normal or unchanged, two patients with abnormal SS underwent contemporaneous shunt revision. Yield of SS is very low, and in the presence of a normal or unchanged head CT, SS provides the imaging basis for contemporaneous shunt revision in 1% (2/192) of cases.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ventriculo-peritoneal shunts are subject to a number of complications including, but not limited to, improper placement, obstruction, infection, fracture, migration, hematoma or loculated fluid formation, or alteration in programmable shunt settings [1]. In adults, suspected ventriculo-peritoneal shunt malfunction is routinely investigated in the emergency department (ED) with head computed tomography (CT), primarily to detect hydrocephalus, and with radiographs of the entire course of the shunt and tubing, a “shunt series” (SS) to evaluate for discontinuity or obstructive phenomena. These studies are often ordered simultaneously.
Previous data on utility of SS are limited but suggest that SS are rarely abnormal and their role in providing an imaging basis for revision is unclear. The few studies that have investigated this topic have primarily been in pediatric populations. One of these, reviewing 67 SS in 21 unique patients, found no abnormal SS, and no patients with normal ventricles on CT underwent shunt revision [2]. A second study assessed the predictive value of radiographs and CT in shunt obstruction in a pediatric population. Among 233 patients studied, the authors found 12 abnormal SS (sensitivity 20%; negative predictive value [NPV] for revision 22%), 50 abnormal head CTs (sensitivity 83%; NPV 93%) and when combined, 53 abnormal shunt investigations (sensitivity 88%; NPV 95%). They concluded that routine performance of SS had a low overall yield but, on rare occasions, detected abnormalities that were missed by CT [3].
Although an abnormal CT may warrant further investigation with radiographs, we wondered if a normal or unchanged head CT might obviate SS altogether in providing an imaging basis for revision. In the present study, we examine the yield of the SS in an adult population to assess its utility among patients undergoing head CT and to determine if it is contributory among patients with a normal or unchanged head CT. Our hypotheses were that (1) the yield of a SS is low, and that (2) when the head CT is normal or unchanged, abnormal SS do not prompt contemporaneous shunt revision.
Materials and methods
Study design
We performed a retrospective record review using a computer database (IDXrad Radiology Information System, IDX Systems, Burlington, VT) and our hospital electronic medical record.
Study setting and population
We identified all SS performed in patients presenting to our adult-only (≥16 years), urban, academic ED over a 34-month period, 1/1/2001 to 3/31/2004. We further identified all head CTs performed in these patients within 24 h of the SS. Analysis was limited to those having these two studies performed within 24 h of one another as part of their ED evaluation for suspected shunt malfunction. Those patients who had a SS but no accompanying CT were excluded from primary analysis, and these studies were reviewed separately.
Study protocol
An emergency physician and emergency radiologist (RG, SL) reviewed all original radiographic interpretations rendered by an emergency radiology staff to determine the results of imaging studies. We also reviewed operative notes, discharge summaries, and ED visit notes to determine whether shunt revision occurred contemporaneous with imaging, which was defined as revision occurring within 72 h of imaging. Surgical procedures performed for reasons other than shunt revision were excluded. Documentation of imaging results for patients with head CT performed at an outside facility and transferred to our ED was obtained from the patients’ electronic medical record.
SS reports were coded as either normal or abnormal. Nondiagnostic exams were excluded. CT reports were coded in one of five categories: (1) normal (with or without prior exam), (2) hydrocephalus without prior exam for comparison, (3) increased hydrocephalus compared to prior exam, (4) unchanged hydrocephalus when compared to prior exam, or (5) decreased hydrocephalus when compared to prior exam. These five categories of CT findings were subsequently collapsed into two groupings to allow comparison of studies indicative of obstruction (increased hydrocephalus and hydrocephalus with no prior imaging) with those not typically suggestive of obstruction (normal, unchanged from prior, and decreased hydrocephalus).
Measurements
Our primary outcome measures were:
-
1)
Percent of cases with an abnormal or possibly abnormal SS,
-
2)
Percent of cases with an abnormal or possibly abnormal SS and a normal or unchanged head CT who underwent shunt revision within 72 h.
Data analysis
For each radiographic test and combination of tests, a two-by-two table was created based on the result of the test and the clinical outcome. Sensitivity, specificity, positive, and NPVs were determined. Descriptive data are presented.
Institutional Review Board approval was obtained, and the study was conducted in compliance with Health Insurance Portability and Accountability Act regulations.
Results
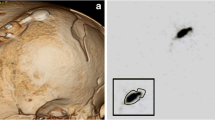
During the study period, 263 cases met the inclusion criteria, with SS and head CT performed among 174 unique patients. The median age was 48, with a range of 17–90. An overview of imaging results and the subsequent number of patients undergoing shunt revision are presented in Fig. 1.
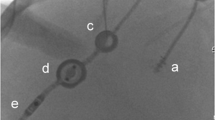
Nine SS were interpreted as abnormal or possibly abnormal and included one or more of the following: fluid collection (“CSF-oma” [CSF, cerebospinal fluid]) around the distal shunt (one), kinking (three), discontinuity (five), and migration (two). Specific imaging findings and outcomes among the nine patients with abnormal SS are presented in Table 1.
A total of 71 (27%) head CTs showed evidence of obstruction: increased hydrocephalus (37); hydrocephalus with no prior CT for comparison (34). A total of 192 head CTs were not otherwise suggestive of new or worsening obstruction: normal (9); no change from prior exam (159); decreased hydrocephalus (24).
Contemporaneous shunt revision took place in a total of 46/263 (17%) cases (Fig. 2). CT provided the sole imaging basis for revision in 21/46 cases (46%). SS provided the sole imaging basis for revision in 2/46 cases (4.3%), such that overall, among those with a normal or unchanged CT, SS provided the sole imaging basis for revision in 1% of cases (2/192). Test characteristics and predictive values are presented in Table 2.
Discussion
Many factors other than imaging are considered when diagnosing shunt malfunction and may influence the decision whether to perform shunt revision. Retrospective determination of which factors contributed primarily to the decision for revision would be mostly speculative. The extent to which imaging informs the decision to revise is uncertain. That revision was performed in 20/46 (43%) cases in which there was no imaging evidence for shunt failure or obstruction, indicates that the role of imaging may be limited [4]. A review of the imaging performed in suspected shunt malfunction can, nevertheless, help clarify and quantify how these studies may or may not provide an “imaging basis” for revision.
In defining a timeframe for which results of imaging were likely to have had a significant impact on the decision for shunt revision, we chose an a priori cutoff of 72 h between time of imaging and shunt revision. Shunt revision performed within 72 h of imaging was deemed “contemporaneous with imaging.” This determination was based on our clinical experience for timing of shunt revisions and further validated by a review of clinical outcomes among those in our cohort, with a normal SS who also underwent revision, that found only one patient whose revision fell within 2 weeks of our 72-h cutoff.
In determining the yield of SS, we used the most inclusive criteria of “abnormal or possibly abnormal,” resulting in the identification of 9 (3%) of the 263 SS. Two of these patients underwent shunt revision despite absence of hydrocephalus on CT, preventing the conclusion that there was no utility of SS among those with normal or unchanged head CT in the evaluation of suspected shunt malfunction among our adult ED population. Our findings are consistent with those in the pediatric population, which also show a very low yield of radiographic SS in assessing suspected shunt malfunction [3]. It is notable that all five patients with obvious discontinuity on SS underwent contemporaneous revision, whereas those with lesser findings (kinking, etc.) and a normal or unchanged head CT did not. Excluding the four “possibly abnormal” SS would decrease the overall yield of abnormal SS to 5/263 (1.9%) and would increase the specificity and PPV to 100% for an abnormal SS in providing the imaging basis for revision.
Although small numbers limit the significance of comparisons, there may be some additional value in SS beyond that suggested by their low yield. For example, the revision rate is 11% when both SS and CT are normal or unchanged, but 100% when both studies are abnormal (Fig. 2). When the SS is normal and the CT is abnormal the revision rate is 31% (21/68), and when the SS is abnormal and the CT is normal, the revision rate is 33% (2/6). However, the relative value of SS should not be overstated, as the small numbers are reflective of the very low sensitivity of 11% for SS. The addition of SS to CT for shunt investigation in these 263 cases increased sensitivity from 55% to only 57% and NPV from 88% to only 89% and resulted in the detection of only 2/192 cases of shunt malfunction that were missed by initial CT.
We identified 16 patients who underwent SS without CT who were excluded from this study, primarily, for reasons other than suspicion of shunt malfunction. In three cases, there were symptoms (fever, lethargy, agitation, dementia) that could be construed as indications to evaluate for shunt malfunction, and it is unclear why neuroimaging was not performed. However, none of these patients underwent shunt revision. Among these 16, there were two abnormal SS. One of these patients had a right upper quadrant abdominal mass on physical exam and radiographic evidence of the shunt tubing curled in the soft tissue. This patient underwent externalization of the shunt. The second patient had more than one catheter in place and evidence of discontinuity in the functioning catheter, but did not undergo revision. Because of difficulties in identifying the cohort, we were unable to perform a similar review of patients undergoing head CT for suspected shunt malfunction without SS.
Limitations
This study has a number of limitations. It carries the limitations inherent to a retrospective design. However, all imaging studies performed in our system are ordered, tracked, and stored electronically, making it highly unlikely that there was incomplete capture of relevant imaging during the study period. For patients who had CT performed at an outside institution, results of these studies were limited to what was reported in our medical record. These results were not as detailed or thorough as radiology reports of studies performed at our own institution. However, the information present was adequate in indicating whether evidence of obstruction was present.
Although our study did not permit a review of the timing of onset of symptoms, this may be important in considering the significance of findings on imaging. In most cases, true shunt failure as detected on shunt radiographs would precede development of hydrocephalus on CT [5], although the time course to the presence of these findings on CT is not clear. Further, we did not explore the reason for, date or type of shunt placement, the symptoms leading to suspicion of shunt malfunction, nor the exact medical decision making behind each shunt revision. Although shunt revision has been used as the gold standard in studies of this type to date, the introduction of programmable shunts may affect results. It is possible that changes on CT may be thought to be due to over- or under-shunting and addressed with adjustment of the shunt rather than suspicion for shunt failure and the need for operative management.
Repeat visits for suspected shunt malfunction and even shunt revision are common in this population. Patients may be admitted, re-evaluated, and restudied only to have shunt revision days or weeks later. It is difficult to determine the potential impact of these patients on our primary outcome measures, as these medical decisions may occur for reasons unrelated to imaging findings.
Although our study period covered 34 months, our sample size of abnormal SS is relatively small. So, although demonstration of low yield is compelling, this also limits what conclusions can be made based on these numbers. Our study might have benefited from a longer study period, yet our sample size is larger than any prior published study in this area. External validity can be problematic in studies such as this one, where patient populations and management strategies may not be generalizable. We feel that our results should be reasonably applicable across most adult populations presenting to EDs. Prospective studies adding to this body of knowledge would be helpful.
Conclusion
In conclusion, although the yield and sensitivity of the radiographic SS is very low, it can rarely detect abnormalities otherwise undetected on initial CT, providing the primary imaging basis for shunt revision.
References
Hunter TB et al (2004) Medical devices of the head, neck, and spine. Radiographics 24(1):257–285, Jan–Feb
Gilbreath PL, Mulligan ME, Sileo DR (1999) Utilization and cost effectiveness review of SS to rule out ventriculoperitoneal shunt malfunction. Emerg Radiol 6:345–349, Dec
Zorc JJ, Krugman SD, Ogborn J, Benson J (2002) Radiographic evaluation for suspected cerebrospinal fluid shunt obstruction. Pediatr Emerg Care 18(5):337–340, Oct
Iskandar BJ, McLaughlin C, Mapstone TB et al (1998) Pitfalls in the diagnosis of ventricular shunt dysfunction: radiology reports and ventricular size. Pediatrics 101:1031–1036
Murtagh FR, Quencer RM, Poole CA (1979) Cerebrospinal fluid shunt function and hydrocephalus in the pediatric age group. Radiology 132:385–388
Acknowledgment
We would like to acknowledge the invaluable assistance of Garrett Fitzmaurice, D.Sc., and Andrew McAfee, M.D., M.Sc., for statistical support; Wendy Mar, M.S., for data retrieval and Jacquelyn Sinclair, R.Ph., M.M., for administrative coordination.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Griffey, R.T., Ledbetter, S. & Khorasani, R. Yield and utility of radiographic “shunt series” in the evaluation of ventriculo-peritoneal shunt malfunction in adult emergency patients. Emerg Radiol 13, 307–311 (2007). https://doi.org/10.1007/s10140-006-0557-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-006-0557-x