Abstract
Traumatic injury of the abdominal aorta is rare and potentially lethal. The authors present the case of a restrained passenger who was involved in a high-speed, head-on motor vehicle accident. On arrival in the emergency department, the patient complained of abdominal pain, was tachycardic and had a large ecchymoses on his right flank and lower abdominal wall. Computed tomography (CT) angiography (CTA) of the abdomen revealed a degloving injury to the abdominal wall, small bowel injury, and a distal abdominal aortic injury with a small amount of retroperitoneal hemorrhage. The patient underwent surgical repair of bowel injuries and the anterior abdominal wall. Because of risk of peritoneal soiling, open repair of the aorta was not attempted. The interventional radiology and vascular surgery services performed an endovascular repair of the aortic injury using a bifurcated endograft.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Report of case
A 31-year-old-male restrained passenger was airlifted to Harborview Medical Center after a 50-mph head-on motor vehicle crash. On arrival in the emergency department, the patient complained of abdominal pain and had a large ecchymosis on his right flank and lower abdominal wall. Although the patient was initially tachycardic, he became hemodynamically stable after fluid resuscitation. There were palpable dorsalis pedis pulses and normal ankle/arm indices bilaterally. Computed tomography angiography (CTA) of the abdomen revealed a degloving injury to the abdominal wall, a small bowel injury, and a distal abdominal aortic injury. The aortic injury extended from below the inferior mesenteric artery into the proximal right common iliac artery and to the orifice of the left common iliac artery (Fig. 1). A small quantity of retroperitoneal hemorrhage was present around the distal aorta. In the operating room, the patient underwent resection and repair of the bowel injuries, and repair of the anterior abdominal wall. The surgeon did not do an open repair of the abdominal aorta because of risk of peritoneal soiling. Immediately after bowel and anterior abdominal wall repair, the interventional radiology and vascular surgery services performed an endovascular repair of the aortic injury using an “Excluder” bifurcated endoprosthesis (Gore, Flagstaff, AZ, USA) in the operating room. A surgical cut down was performed to both common femoral arteries. Aortography was performed, and the aorta was measured for stent placement. The aortic diameter was 17.5 mm above the injury and 20 mm at the injured aortic bifurcation. The common iliac arteries measured 10 mm. A 23-mm diameter aortic graft with 12-mm limbs was placed (Figs. 2 and 3). A bifurcated stent graft was selected due to involvement of the distal abdominal aorta with extension into both common iliac arteries as this is the only method to preserve all three lumens.
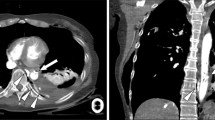
A 31-year-old male with a distal abdominal aortic injury from a high-speed motor vehicle crash. a Axial CTA of the distal abdominal aorta at the aortic bifurcation shows circumferential intimal flaps. b Coronal oblique thin-slab maximum intensity volumetric reformation of the distal abdominal aorta shows the proximal and distal extent of the injury. The intimal flaps extend into the origins of the common iliac arteries
Pre- and post-endograft placement aortogram in a 31-year-old male with a distal abdominal aortic injury. a Flush aortogram demonstrates a small aortic pseudoaneurysm with proximal and distal intimal flaps. The distal aspect of the injury involves the aortic bifurcation. b Following endograft placement, the intimal flaps are no longer visible and the aorta has a normal contour
Discussion
Abdominal aortic injury is a rare consequence of blunt abdominal trauma and represents only 4–6% of aortic injuries, the remainder involving the thoracic aorta [1]. These injuries are commonly associated with high-speed motor vehicle accidents, and have been linked to steering wheel injury to the lower abdomen and the use of lap-belt restraints [2]. Acute manifestations include symptoms of acute arterial insufficiency, an acute abdomen, or neurologic deficits. The lesion may be asymptomatic initially, when there are no associated injuries to produce an acute abdomen, or when there is a non-occlusive intimal flap. The mechanism of injury is thought to be due to direct compression of the aorta against the spine, although other theories postulate elevation of the intraluminal aortic pressure, causing stretching of the aortic wall, and aortic distraction from hyperflexion [2]. Injuries are typically limited in length. The most commonly injured sites are at the level of the inferior mesenteric artery (33%), renal arteries (24%), and between the IMA and bifurcation (19%) as in this case [3].
Death has occurred in three of the four documented conservatively treated examples [3], so the current consensus is that treatment is necessary, except for those with minimal intimal disruptions. The more severe injuries may be divided into true dissection, where there is an intimal flap with a false lumen; and a transection, where the lesion is often circumferential, with intimo-medial flaps proximal and distal to a dilated segment due to a compromised aortic wall. Surgical treatment is associated with an overall mortality of 27%. Because of the high incidence of associated bowel injury [3], surgical placement of a prosthetic graft at the time of initial laparotomy risks graft infection. Some have described endoluminal treatment of aortic injuries [2], and this, using non-covered stents, provides excellent results with inframesenteric aortic dissections [4]. For those cases of contained transection, both covered and uncovered stents [4] have been employed successfully. This endoluminal approach minimizes the risk of contamination from the potentially soiled peritoneum. However, with evidence of spinal cord ischemia or hypovolemic paraplegia, open repair with surgical revascularization of lumbar arteries would be preferred [4].
Traumatic injury of the abdominal aorta is rare and potentially lethal. As there may be no immediate sign of injury, high clinical suspicion in the setting of a vertebral fracture or lap-belt sign warrants CT aortography. Endovascular stent grafts provide a less invasive method of repair in this population.
References
Naude GP, Back M, Perry MO, Bongard FS (1997) Blunt disruption of the abdominal aorta: report of a case and review of the literature. J Vasc Surg 25:931–935
Fontaine AB, Nicholls SC, Borsa JJ, Hoffer E, Bloch RD, Kohler T (2001) Seat belt aorta: endovascular management with a stent-graft. J Endovasc Ther 8:83–86
Lock JS, Huffman AD, Johnson RC (1987) Blunt trauma to the abdominal aorta. J Trauma 27:674–677
Berthet JP, Marty-Ane CH, Veerapen R, Picard E, Mary H, Alric P (2003) Dissection of the abdominal aorta in blunt trauma: endovascular or conventional surgical management? J Vasc Surg 38:997–1003, discussion 1004
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gunn, M., Campbell, M. & Hoffer, E.K. Traumatic abdominal aortic injury treated by endovascular stent placement. Emerg Radiol 13, 329–331 (2007). https://doi.org/10.1007/s10140-006-0556-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-006-0556-y