Abstract
The purpose of this study was to determine the necessity for splenectomy in patients with active extravasation on contrast enhanced CT secondary to splenic trauma. We reviewed cases of splenic injury and classified these according to the American Association for the Surgery of Trauma (AAST) grading scale. The presence of active extravasation and associated injuries was assessed. Chart review was then performed to determine age, sex, mechanism of injury, indications for splenectomy, and clinical outcome. Of 82 cases evaluated, 12 grade I, 15 grade II, 30 grade III, 17 grade IV, and 8 grade V injuries were present. Eighteen patients were actively extravasating. Of extravasating patients, 13 eventually underwent open splenectomy or embolization and five (27.8%) were managed expectantly with success. Of grade IV injuries, 9/17 showed active extravasation, of which six underwent splenectomy. Of grade V injuries, 3/8 showed active extravasation, and all three underwent intervention. Splenectomy may not be necessary in appropriately chosen patients with active extravasation from the spleen in blunt abdominal trauma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The spleen is the most commonly injured solid abdominal organ and a recent study of blunt abdominal trauma showed the spleen is also the most common organ to show arterial extravasation on initial CT examination [1]. Bleeding from splenic trauma can be devastating and unstable patients are usually taken immediately to surgery; however, appropriate management for the clinically stable patient with splenic injury remains controversial. Given the lifelong increased risk of sepsis in asplenic patients, conservative therapy has been gaining popularity in more recent years.
Contrast enhanced CT examination of the abdomen is now commonplace in blunt trauma to evaluate for solid visceral organ injury, however the American Association for the Surgery of Trauma (AAST) grading scale has not been shown to be reliable in the prediction of nonoperative management failure in splenic injury. While the AAST grading scale for splenic injury has been adapted to CT findings, often the surgical findings are poorly concordant. Concurrent imaging findings, such as intraperitoneal hemorrhage or active extravasation, have no place in the current grading scale. While increased AAST grade of injury has been shown to be associated with increased probability of splenectomy, it has not been shown to be predictive of which patients will fail observation. Other variables have been considered to help determine which patients will eventually require splenectomy including transfusion requirements and other clinical factors (age and mechanism of injury) but has not been widely reproduced or accepted [2].
Several studies have investigated the presence of active extravasation and the presence of vascular malformations and have concluded that patients with these findings are much more likely to fail observation. Therefore splenectomy should be performed in these patients regardless of their clinical status [3–5]. Other studies indicated that the only absolute predictor for failure of conservative management is clinical instability, regardless of the presence of active extravasation [6].
In our institution we have observed that some of our surgeons favor nonoperative management even when contrast extravasation is present. The purpose of this study was therefore to examine our patient population and determine whether active extravasation predicts the eventual need for splenectomy.
Materials and methods
A retrospective search was performed for patients that had been assigned a diagnostic code related to splenic injury at discharge or expiration between the dates of April 1999 and November 2002 from William Beaumont Hospital, a busy level I trauma center in Royal Oak, MI, USA. 87 patients were identified that sustained injuries as a result of blunt trauma and had a contrast enhanced CT examination during initial evaluation in the Emergency Department. Standard contrast enhanced CT examination of the abdomen and pelvis of adults in our institution includes intravenous injection of 120 cc Omnipaque 300 (Amersham, Buckinghamshire, UK) at a rate of 3 cc/s with a delay of 90 s. Variations occur on a case-to-case basis (pediatric cases, patients with renal failure, etc.). 5 mm axial images are obtained from above the diaphragm through the pubic symphysis. Oral and rectal contrast are not routinely administered to trauma patients at our institution. Over the period studied two different CT scanners were used: a Siemens Somatom Plus 4 (single slice helical) and a Siemens Somatom Volume Zoom (four slice).
These cases were reviewed on PACS stations by the authors (CR and SZJ) who were blinded to clinical outcome for determination of AAST grades and the presence or absence of extravasation. Active extravasation was defined by the presence of contrast blush within or adjacent to an injured spleen. Attempt to discern the presence of pseudoaneurysm was not performed as delayed or follow up examinations were rarely available. Studies of poor quality including those with suboptimal contrast bolus and patient motion were included in the study. A retrospective chart review of all 82 patients was undertaken to determine clinical outcome that fell into one of four categories: successful observation, failed observation, splenectomy, or endovascular therapy. Failed observation was defined as the requirement for splenectomy during the documented observation period.
Results
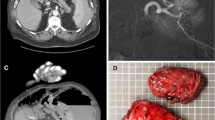
Eighty-seven patients were identified as having splenic injury due to blunt trauma on CT examination. About 70% were male and approximately 50% were due to motor vehicle accidents. The remainder was composed mainly of falls (18%) and sports related injuries (11%). The average patient age was 34 years with ages ranging from 2 years to 94 years. Figures 1, 2, and 3 demonstrate AAST grade III–V splenic injuries as seen in our patient population.
A summary of splenic injury in our patients by AAST grade is listed in Table 1. Of all patients reviewed, 19 patients (22%) required immediate splenectomy. Three of these patients died intraoperatively. One patient was referred to angiography for successful embolization. Of those patients that entered observation, four (5%) failed observation and required urgent splenectomy. 63 (72%) of patients were successfully observed. Please see summary in Fig. 4.
A total of 21 (24%) patients were actively extravasating on initial CT. Of these patients, 11 (52% of actively extravasating patients) went immediately to surgery and one (5%) went immediately to interventional radiology for embolization. Seven (33%) were successfully observed and two patients (10%) failed observation. A breakdown of outcome by grade is presented in Table 2.
Of the 67 patients that were initially considered clinically stable enough to enter observation, nine (13%) were actively extravasating and a total of four (6%) failed observation which includes two patients that weren’t initially extravasating; one patient had a grade II injury without extravasation, one had a grade IV injury without extravasation. Of the other two patients, one had a grade III injury with active extravasation, and one had a grade IV injury with active extravasation. A summary is provided in Table 3.
One patient developed delayed rupture confirmed by CT examination and was successfully treated with observation. This patient was counted in the successful observation group as the he did not require splenectomy. This data regarding all patients included in the study is presented in a flow chart in Fig. 5.
Discussion
The CT examination has become the standard of care for determination of intraabdominal injury in blunt trauma and recent literature is discordant regarding the clinical value to referring physicians. Some studies suggest that active extravasation predicts failure of conservative therapy while others argue that the only patients that require splenectomy without a trial of observation are those that are clinically unstable.
In our study, nonoperative management was attempted in 67 of 87 patients (77%) and 4 of 67 (6%) of the patients that were determined by the surgical service to be stable enough to enter observation, regardless of the presence of extravasation, developed hemodynamic instability requiring urgent splenectomy. The remaining 72% of all patients (63 of 87), or 94% of patients in which observation was attempted (63 of 67), were successfully observed and discharged home. Our rates of observation are higher than several previously published studies [2–5]. Active extravasation was detected in 24% of all patients, a number comparable to other studies [1, 3, 5, 7]. All patients considered, the positive predictive value of active extravasation for the need for splenectomy is 67% with a negative predictive value of 85%, suggesting that the majority of patients with active extravasation will require splenectomy. However, when the evaluation of the clinical service is considered and only those patients considered stable enough to tolerate nonoperative management are examined, the positive predictive value of active extravasation in regards to splenectomy drops to 22% with a negative predictive value of 97%. This suggests that the presence of active extravasation is a poor predictor for failure in the initially stable patient and that, as of yet, no reliable radiographic predictor exists in this regard. Our findings further support proposals, mostly in the surgical literature, that the finding of active extravasation may be present but can be clinically insignificant [6]. In addition, as discussed by Federle et al. [7], a grading scheme that focuses solely on one organ with disregard to injury within the remainder of the abdomen is not likely to accurately predict outcome.
Upon review of the current literature an often-present complicating factor, also present in this study, is surgeon bias; patients that have CT findings suggestive of arterial extravasation are more likely to receive intervention, not necessarily as indicated by the clinical status, but because the surgeon is aware of CT findings. As such, the surgeon may be more wary to observe the patient and may have a lower threshold for intervention [6]. Therefore, it is difficult to infer that because an intervention was performed that is was absolutely required. In our institution, where many of our surgeons are more comfortable with nonoperative management, a higher percentage of patients are being observed successfully, even in the face of active extravasation.
Since the conclusion of this study endovascular techniques have become more popular at our institution. Anecdotal observation has shown that increased numbers of stable or high risk operative patients may be visiting the angiography suite prior to observation for further evaluation of active extravasation seen on CT examination and possible intervention.
Abbreviations
- AAST:
-
American association for the surgery of trauma
References
Yao DC, Jeffrey RB, Mirvis SE, Weekes A, Federle MP, Kim C et al (2002) Using contrast-enhanced helical CT to visiualize arterial extravasation after blunt abdominal trauma: incidence and organ distribution. Am J Roentgenol 178(1):17–20
Velmahos GC, Chan LS, Kamel E, Murray JA, Yassa N, Kahaku D et al (2000) Nonoperative management of splenic injuries: have we gone too far? Arch Surg 135:674–681
Gavant ML, Schurr M, Flick PA, Croce MA, Fabian TC, Gold RE (1997) Predicting clinical outcome of nonsurgical management of blunt splenic injury: using CT to reveal abnormalities of splenic vasculature. AJR Am J Roentgenol 168:207–212
Nwomeh BC, Nadler EP, Meza MP, Bron K, Gaines BA, Ford HR (2004) Constrast extravasation predicts the need for operative intervention in children with blunt splenic trauma. J Trauma 56:537–541
Schurr MJ, Fabian TC, Gavant M, Croce M, Kudsk KA, Minard G et al (1995) Management of blunt splenic trauma: computed tomographic contrast blush predicts failure of nonoperative management. J Trauma 39(3):507–512
Omert LA, Salyer D, Dunham MC, Porter J, Silva A, Protech J (2001) Implications of the “Contrast Blush” finding on computed tomographic scan of the spleen in trauma. J Trauma 51(2):272–278
Federle MP, Courcoulas AP, Powell M, Ferris JV, Peitzman AB (1998) Blunt splenic injury in adults: clinical and CT criteria for management, with emphasis on active extravasation. Radiology 206:137–142
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rhodes, C.A., Dinan, D., Jafri, S.Z. et al. Clinical outcome of active extravasation in splenic trauma. Emerg Radiol 11, 348–352 (2005). https://doi.org/10.1007/s10140-005-0416-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-005-0416-1