Abstract
Background
To compare the efficacy of oxaliplatin-based and oxaliplatin-free adjuvant chemotherapies in patients with different Lauren type gastric cancers after D2 gastrectomy.
Methods
From our established gastric cancer database, patients with pathological stage II and III gastric cancer who received adjuvant chemotherapy after D2 gastrectomy at Zhongshan Hospital of Fudan University were analyzed. Patients who received different adjuvant chemotherapy regimens were divided into two subgroups: oxaliplatin-based and oxaliplatin-free subgroup. Clinical outcomes were analyzed according to pathological stage and different Lauren types.
Results
From Jan 2010 to June 2017, a total of 580 patients met all the eligibility criteria and were enrolled. The median DFS for all the patients was 24.37 months and the median OS was 56.70 months. In patients with intestinal type gastric cancer, the median DFS of the oxaliplatin-based subgroup was significantly longer than that of oxaliplatin-free subgroup (48.73 vs. 18.33 months, P < 0.001). The median OS was not reached in the oxaliplatin-based subgroup and 54.33 months in the oxaliplatin-free subgroup (P = 0.006). In patients with diffuse type gastric cancer, neither DFS nor OS differed significantly between two subgroups. In multivariate analysis, oxaliplatin-based adjuvant chemotherapy was independent positive predictor of DFS (HR 0.40; 95% CI 0.28–0.59; P < 0.001) and OS (HR 0.35; 95% CI 0.20–0.62; P < 0.001) in patients with intestinal type gastric cancer.
Conclusions
The results of our study suggested that oxaliplatin-based adjuvant chemotherapy was more effective in patients with intestinal type gastric cancer after D2 gastrectomy but showed no more survival benefit in patients with diffuse type.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer is one of the most common malignancies in the gastrointestinal tract. About one million new cases of stomach cancer are estimated to have occurred each year all over the world, making it the fifth most common cancer and the third leading cause of cancer related deaths [1, 2]. More than 70% of cases occur in developing countries and half of cases occur in Eastern Asia (mainly in China) [1]. The highest estimated mortality rates also occurred in Eastern Asia [1]. While D2 gastrectomy as a standard surgical procedure is crucial for potential cure in gastric cancer, it is unfortunate that metastases and recurrences are relatively common after surgery and patients with gastric cancer still have a very poor prognosis [3, 4].
Globally, there has been a large volume of randomized clinical trials describing the role of adjuvant chemotherapy in decreasing the risk of relapse and improving the survival of patients with gastric cancer [5,6,7,8,9,10,11,12]. Notably, there have been some clinical trials which showed a survival benefit with oxaliplatin-based adjuvant chemotherapy after D2 gastrectomy. The CLASSIC trial, a multi-center study in Eastern Asia, showed that oxaliplatin plus capecitabine regimen as adjuvant chemotherapy after curative D2 gastrectomy improved the disease-free survival (DFS) and overall survival (OS) compared with surgery alone [5, 6]. Other studies reported that adjuvant chemotherapy with oxaliplatin plus S-1 for gastric cancer was also associated with survival benefit [7,8,9]. Based on these results, the oxaliplatin-based adjuvant chemotherapy has been one of the standard treatments for operable gastric cancer. Meanwhile, some representative studies have documented the survival benefit of oxaliplatin-free adjuvant chemotherapy for patients after D2 gastrectomy. The ACTS-GC trial which was conducted in Japan showed that S-1, a novel oral fluoropyrimidine, as a mono-medicine adjuvant regimen could improve relapse free survival rate and overall survival rate compared with surgery alone [10, 11].
Generally, the decision and choice of chemotherapy treatment for gastric cancer patients are mainly based on pathological TNM stage according to the AJCC staging system. Meanwhile, Lauren classification, which was based on the tissue structure and biological behavior of gastric cancer, is one of the most widely applicable classification systems around the world and plays a very important role in distinguishing the biological behaviors of gastric cancer [13]. The Lauren classification stratified gastric cancer into intestinal type and diffuse type in 1965 [13]. The intestinal type was described as a tumor with gland-like structures, resembling colonic carcinoma accompanied by intestinal metaplasia, while the diffuse type was described as a tumor composed of a population of non-cohesive, scattered tumor cells which differentiated poorly [14]. The classification of the two types of gastric cancer had been used to distinguish prognosis of patients with gastric cancer. Several studies have indicated that patients with intestinal type gastric cancer had a better prognosis than those with diffuse type [14, 15].
As one of the third-generation platinum, oxaliplatin has been proved to decrease the risk of relapse and improve the survival for patients with gastric cancer. To the best of our knowledge, few studies have evaluated the efficacy of adjuvant chemotherapy regimens with or without oxaliplatin for gastric cancer patients of different Lauren types after D2 gastrectomy. The main purpose of our study was to compare the prognosis of patients receiving oxaliplatin-based adjuvant chemotherapy regimen with that of patients receiving oxaliplatin-free adjuvant chemotherapy regimen in intestinal type or diffuse type gastric cancer.
Materials and methods
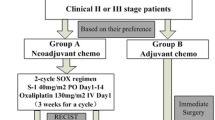
Patients selection
From our established gastric cancer database which was used to record information of patients with gastric cancer from stage I to IV, we investigated 1069 patients who underwent D2 gastrectomy and received adjuvant chemotherapy at Zhongshan Hospital (Fudan University, Shanghai, China) between January 2010 and June 2017. In this database, our requirements to screen patients for our study were as follows: (1) histologically proven gastric adenocarcinoma after radical gastrectomy with D2 lymph node dissection, (2) patients aged between 20 and 75 years with adequate organ functions, (3) no preoperative chemotherapy or radiotherapy, (4) no evidence of metastatic disease, (5) pathological stage II or III gastric cancer according to the 8th edition of the AJCC cancer staging manual with Lauren classifications (diffuse type or intestinal type), (6) patients receiving adjuvant chemotherapy which complied with our requirements, (7) no adjuvant radiotherapy or chemoradiotherapy within 6 months after surgery and (8) no synchronous or metachronous cancer. The patients with positive resection margin, M1 lymph node, distant metastases or change of adjuvant chemotherapy regimen were excluded from our study. In the eligible patients, the dose escalations were allowed in the absence of grade 2–4 toxic effects.
Our database information included patients’ gender, age, pathological and clinical TNM stage, detailed pathological information, chemotherapy regimen, date of diagnosis, date of operation, date of initiation and termination of chemotherapy, date of recurrence or progression, date of follow-up or death and so on.
This study was performed with the approval of the Ethics Committee of Zhongshan Hospital affiliated to Fudan University. All patients were enrolled after signing informed consent.
Chemotherapy regimen
All patients received adjuvant chemotherapy within 6 weeks after surgery. We performed adjuvant chemotherapy based on guidelines of National Comprehensive Cancer Network (NCCN) and Chinese Society of Clinical Oncology (CSCO). Patients who received different adjuvant chemotherapy regimens were divided into two subgroups, which were oxaliplatin-based regimen and oxaliplatin-free regimen. The oxaliplatin-based chemotherapy regimen subgroup included XELOX (oxaliplatin 130 mg/m2 on day 1 of each cycle intravenously, oral capecitabine 1000 mg/m2 twice daily on day 1–14 of each 3-week cycle) and SOX (oxaliplatin 130 mg/m2 on day 1 of each cycle intravenously, oral S-1 a daily dose of 80, 100, or 120 mg in two separate doses on the basis of different body surface area on day 1–14 of each 3-week cycle). The oxaliplatin-free chemotherapy regimen subgroup included S-1 (a daily dose of 80, 100, or 120 mg in two separate doses on the basis of different body surface area orally for 2 weeks, followed by 1 week of no chemotherapy).
Follow-up
The database was followed up every year in the form of outpatient visit and telephone enquiry. The follow-up visit rates are about 80% every year. All patients were followed up with physical examination, serum tumor marker evaluation, chest CT and abdominal CT, gastrointestinal endoscopic examination. When necessary, whole-body bone scan, abdominal magnetic resonance imaging (MRI) and positron emission tomography/computed tomography (PET/CT) scan were additionally performed.
Statistical analysis
The date of the first relapse and the date of death were recorded. The primary endpoint was the disease-free survival (DFS). The secondary endpoint was overall survival (OS). DFS was measured from the date of the operation to the date of recurrence of the original gastric cancer, development of a new gastric cancer or death from any cause. OS was defined as the period from the date of the operation to the date of the last follow-up or death for any reason. DFS and OS were estimated using the Kaplan–Meier method. The Chi-squared test was used to compare the categorical parameters. Analyses were performed with SPSS software (version 19.0). Estimates of treatment effect were calculated as hazard ratios (HRs) with 95% confidence intervals (CIs). Significant variables in the univariate analysis were further estimated in multivariate analysis using the Cox proportional hazards model. P < 0.05 was considered statistically significant.
Results
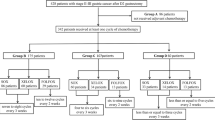
From January 2010 to June 2017, a total of 580 patients satisfied all the eligibility criteria and 489 patients were excluded from the study (Fig. 1). The last follow-up time was June 2018 and the median follow-up time was 25.77 months (range 2.90–103.2 months). Of the 580 patients, 344 patients (59.3%) had recurred and 185 patients had died (31.9%) by the last follow-up day. For all the eligible patients, there were 143 patients (24.7%) with pathological stage II and 437 patients (75.3%) with pathological stage III gastric cancer. According to the Lauren classification, there were 331 patients (57.1%) with diffuse type and 249 patients (42.9%) with intestinal type gastric carcinoma. In the oxaliplatin-based chemotherapy regimen subgroup, 391 patients (83.7%) received at least 6 cycles of adjuvant chemotherapy.
The characteristics of the 580 patients were summarized in Table 1. The patients with diffuse type gastric cancer had a higher female ratio and more advanced tumor stage than patients with intestinal type. The median disease-free survival for the patient population was 24.37 months (Fig. 2a), and the median overall survival was 56.70 months (Fig. 2b). The median DFS of patients with diffuse type and intestinal type were 21.20 months and 32.17 months, respectively (P < 0.001, HR 1.56, 95% CI 1.26–1.92, Fig. 2c). The median OS of patients with diffuse type was 46.60 months, while that of patients with intestinal type was not reached (P < 0.001, HR 1.82, 95% CI 1.32–2.36, Fig. 2d). The background of the patients who received adjuvant chemotherapy with and without oxaliplatin in each histological subtype is summarized in Table 2. In patients with intestinal and diffuse type gastric cancer, oxaliplatin-containing adjuvant chemotherapy is more commonly used in patients with gastric lymph node metastasis and patients with stage III disease, which differed significantly. However, in patients without gastric lymph node metastasis or patients with pathological stage II, there was no significant difference in the choice of the two regimens. There were no significant differences in median DFS (oxaliplatin-based subgroup: 25.73 months vs. oxaliplatin-free subgroup: 19.63 months, P = 0.174, HR 0.84, 95% CI 0.63–1.09, Fig. 2e) and median OS (oxaliplatin-based subgroup: 60.50 months vs. oxaliplatin-free subgroup: 46.60 months, P = 0.558, HR 0.90, 95% CI 0.61–1.30, Fig. 2f) between patients receiving oxaliplatin-based chemotherapy and that receiving oxaliplatin-free chemotherapy. More specially, in patients of pathological stage II, the median DFS in oxaliplatin-based and oxaliplatin-free subgroups were 50.47 months and 59.83 months, respectively, which did not differ significantly(P = 0.710, HR 0.90, 95% CI 0.52–1.56, Fig. 2g). However, in patients of pathological stage III, the median DFS in oxaliplatin-based subgroup was significantly longer than that in oxaliplatin-free subgroups(21.80 months and 16.57 months, respectively, P = 0.001, HR 0.61, 95% CI 0.38–0.78, Fig. 2g). The median OS did not differ significantly between oxaliplatin-based and oxaliplatin-free subgroups in both patients of pathological stage II and stage III. More specially, in patients of stage II, the median OS was not reached in both oxaliplatin-based and oxaliplatin-free subgroups (HR 0.78, 95% CI 0.35–1.71, Fig. 2h). And in patients of stage III, the median OS was 55.43 and 34.30 months in oxaliplatin-based and oxaliplatin-free subgroups, respectively (HR 0.69, 95% CI 0.40–1.06, Fig. 2h). Tables 3 and 4 showed the predictive factors in univariate and multivariate analysis on DFS and OS. Multivariate analysis indicated that Lauren type, chemotherapy regimen with oxaliplatin and pathological TNM stage was independent predictors for DFS and OS of all eligible patients. Intestinal type gastric cancer was correlated with better DFS (P < 0.001) and OS (P < 0.001).
Kaplan–Meier survival curves of disease-free survival and overall survival. DFS analysis (a) and OS analysis (b) of all eligible patients. DFS analysis (c) and OS analysis (d) of intestinal type and diffuse type. DFS analysis (e) and OS analysis (f) of oxaliplatin-based chemotherapy subgroup and oxaliplatin-free chemotherapy subgroup. DFS analysis (g) and OS analysis (h) of patients with pathological stage III and pathological stage II
In the intestinal type subgroup, 184 patients received oxaliplatin-based chemotherapy and 65 patients received oxaliplatin-free chemotherapy. The oxaliplatin-based chemotherapy subgroup had a longer median DFS and OS compared with oxaliplatin-free chemotherapy subgroup (DFS: 48.73 months vs. 18.33 months, P < 0.001, HR 0.48, 95% CI 0.27–0.62, Fig. 3a; OS: not reached vs. 54.33 months, P = 0.006, HR 0.48, 95% CI 0.22–0.77, Fig. 3b). For patients with intestinal type of pathological stage III, the oxaliplatin-based chemotherapy subgroup had a significant longer median DFS (34.87 months vs. 18.17 months, P < 0.001, HR 0.43, 95% CI 0.20–0.56, Fig. 3c) and median OS (69.80 months vs. 35.47 months, P = 0.007, HR 0.44, 95% CI 0.15–0.74, Fig. 3d) than those of oxaliplatin-free chemotherapy subgroup. For patients with intestinal type of pathological stage II, as the same, the oxaliplatin-based chemotherapy subgroup achieved significantly longer DFS and OS compared with oxaliplatin-free chemotherapy subgroup (DFS: not reached vs. 49.00 months, P = 0.013, HR 0.39, 95% CI 0.16–0.80, Fig. 3e; OS: not reached vs. not reached, P = 0.031, HR 0.25, 95% CI 0.07–0.87, Fig. 3f). Univariate and Multivariate analysis indicated that chemotherapy regimen with oxaliplatin and pathological TNM stage was independent predictors for DFS and OS (Tables 3, 4). Oxaliplatin-based adjuvant chemotherapy was correlated with better DFS (P < 0.001) and OS (P < 0.001).
Kaplan–Meier survival curves of disease-free survival and overall survival according to different adjuvant chemotherapy regimen and Lauren type. DFS analysis (a) and OS analysis (b) for patients in the oxaliplatin-based chemotherapy subgroup and the oxaliplatin-free chemotherapy subgroup in different Lauren type gastric cancer. DFS analysis (c) and OS analysis (d) for patients in the oxaliplatin-based chemotherapy subgroup and the oxaliplatin-free chemotherapy subgroup in different Lauren type gastric cancer of pathological stage III. DFS analysis (e) and OS analysis (f) for patients in the oxaliplatin-based chemotherapy subgroup and the oxaliplatin-free chemotherapy subgroup in different Lauren type gastric cancer of pathological stage II
In the diffuse type subgroup, 283 patients received oxaliplatin-based chemotherapy and 48 patients received oxaliplatin-free chemotherapy. There were no significant differences on DFS and OS between the oxaliplatin-based and oxaliplatin-free chemotherapy subgroups (DFS: 20.17 months vs. 22.17 months, P = 0.173, HR 1.33, 95% CI 0.89–1.87, Fig. 3a; OS: 46.77 months vs. 44.77 months, P = 0.354, HR 1.29, 95% CI 0.77–2.06, Fig. 3b). In patients with pathological stage III, the DFS and OS did not differ significantly between the oxaliplatin-based and oxaliplatin-free chemotherapy subgroups (DFS: 19.23 vs. 16.47 months, HR 0.73, 95% CI 0.41–1.18, Fig. 3c. OS: 41.57 vs. 34.30 months, HR 0.82, 95% CI 0.41–1.58, Fig. 3d). In patients with pathological stage II, as the same, the DFS and OS did not reach significant difference between the oxaliplatin-based and oxaliplatin-free chemotherapy subgroups, either(DFS: 27.23 months vs. not reached, HR 2.25, 95% CI 0.98–4.36, Fig. 3e. OS: 52.23 months vs. not reached, HR 1.62, 95% CI 0.56–4.35, Fig. 3f). Univariate and multivariate analyses on factors influencing DFS and OS of patients with diffuse type were presented in Tables 3 and 4. Only pathological TNM stage was indicated as an independent predictor for DFS (P < 0.001) and OS (P = 0.002).
Discussion
The standard surgical procedure for gastric cancer in Asia, especially Japan, Korea and China is radical gastrectomy plus D2 lymph node dissection. The evidence for postoperative adjuvant chemotherapy comes from the results of two large-phase III studies. One was the ACTS-GC study [10] conducted in Japan, which evaluated the efficacy of a 1-year adjuvant chemotherapy with S1 monotherapy in patients with gastric cancer after D2 radical surgery. The results showed that the 3-year overall survival rates of the adjuvant chemotherapy group and the surgery alone group were 80.1% and 70.1%, respectively, and the risk of death in the adjuvant chemotherapy group was reduced by 32% (P = 0.0024). The CLASSIC study [5] included a total of 1035 gastric cancer patients in 37 clinical centers in Korea, China and Taiwan, with the aim of evaluating whether postoperative adjuvant chemotherapy(XELOX regimen) can reduce the risk of recurrence. The results showed that the 3-year DFS in the adjuvant chemotherapy group and the observation group were 74% and 60%, respectively, and the risk of disease progression in the adjuvant chemotherapy group was reduced by 44% (P < 0.0001). At the ASCO meeting in 2018, a recent phase III clinical trial conducted in Japan reported the interim study results. Compared with S1 monotherapy, docetaxel combined with S1 as an adjuvant chemotherapy regimen after D2 radical surgery not only significantly improved 3-year recurrence-free survival (65.9% vs 49.5%, HR 0.632, P = 0.0007), but also further reduced the risk of lymph node, peritoneal and distant metastasis. The three Phase III studies mentioned above are the most important medical evidence for postoperative adjuvant chemotherapy for gastric cancer. However, so far, no clinical studies have compared platinum- and platinum-free adjuvant chemotherapy regimens.
Besides, although the Lauren classification system dates back to 1965, it is still widely accepted and has been proved to be one of the most meaningful prognostic factors for gastric cancer. Clinical trial conducted by Qiu et al. [14] showed that gastric carcinoma patients with the diffuse type had poorer prognosis than patients with intestinal type. This view was supported by Liu in 2013 who claimed that intestinal type gastric cancer showed a higher accumulative 5-year survival rate compared to that in diffuse type cases [15]. However, the three previously mentioned clinical studies on adjuvant chemotherapy for gastric cancer have not compared the prognosis of different Lauren classifications of gastric cancer. In addition, the three clinical trials are interventional studies, which are limited by a lot of conditions, such as age, physical condition of patients, etc. As a result, practical applications of chemotherapy regimen as exactly as calculated in the trials are limited. This study is based on our established gastric cancer database and long-term follow-up data. The choice of patients’ chemotherapy regimens is based on guidelines from different eras and the actual conditions of patients.
In our study, a total of 580 gastric cancer patients after D2 gastrectomy were divided by Lauren classification and subdivided into oxaliplatin-based chemotherapy group or oxaliplatin-free chemotherapy group. Our study showed that in the intestinal type gastric cancer, oxaliplatin-based adjuvant chemotherapy after gastrectomy reduced the risk of cancer recurrence and death compared with oxaliplatin-free chemotherapy regimen, which suggested that the intestinal type of gastric cancer was more sensitive to oxaliplatin. But for diffuse type gastric cancer, the patients receiving oxaliplatin-based chemotherapy did not have significant better DFS and OS than patients receiving oxaliplatin-free chemotherapy regimens. So the gastric cancer patients of the diffuse type may not benefit from oxaliplatin.
Therefore, if clinicians would be able to choose adjuvant chemotherapy regimen based on Lauren classification after D2 gastrectomy, it will be of great benefit to gastric cancer patients. In recent years, some clinical studies have shown that adjuvant chemotherapy with docetaxel-based regimen yielded promising DFS and OS in gastric cancer patients who had undergone D2 gastrectomy [12, 16]. We believe that docetaxel-based regimen is a candidate for future trials to explore the optimal adjuvant chemotherapy regimen for diffuse type gastric cancer.
As mentioned before, diffuse type gastric cancer has worse clinical outcomes than intestinal type of gastric cancer. According to our study, the patients of intestinal type were more sensitive to oxaliplatin, but patients with diffuse type were not. So in the patients with diffuse type gastric cancer, the research of insensitivity mechanism to oxaliplatin would be of interest. In the diffuse type gastric cancer, signet ring cell was the predominant histological component [17]. Signet ring cells lacked free ribosomes but were rich in lysosomes and mucus, which impeded anticancer chemotherapeutic drug to get into the cancer cells [18, 19]. Other studies found that increased activity of RhoA, which was the founding member of the Rho GTPase family, in diffuse type gastric cancer was correlated with worse overall survival and inhibition of RhoA could reverse chemotherapy resistance to cisplatin in diffuse type cancer stem-like cell [20, 21]. Further research focusing on mechanism of oxaliplatin-resistance of diffuse-type gastric cancer is warranted.
Nevertheless, there has been conflicting result reported that in diffuse type gastric cancer; patients in the oxaliplatin-based chemotherapy group had a longer median DFS (47.0 months vs. 28.6 months, P = 0.04) and OS (51.9 months vs. 34.5 months, P = 0.048) compared with those in taxane-based chemotherapy group [22]. We believed that the possible reasons for these conflicting results might be the selection of enrolled patients and different adjuvant chemotherapy regimens. While Zheng’s study enrolled patients of pathological stage IB–IV, we enrolled patients of pathological stage II or III. Meanwhile, in Zheng’s study, the taxane-based chemotherapy included cisplatin which belongs to the platinum. We speculated that the selection of patients with pathological stage IV and the addition of cisplatin might influence the results.
Our study has some limitations. In the ACTS-GC study [10] and the CLASSIC study [5], patients with pathological stage III accounted for 55.3% and 50.1%, respectively, while stage III patients in our study accounted for 75.3%, which was much higher than the previous two studies. The possible reason is that the screening rate of gastric cancer in China is lower than that in Japan and South Korea so that most patients are at locally advanced stage at the time of diagnosis. In our study, the 5-year RFS and OS of patients with stage II were 43.0% and 62.3%, respectively, compared with 79.2% and 84.2% of the stage II patients in the adjuvant chemotherapy group in the ACTS-GC study. The 5-year RFS and OS of patients with stage III were 19.5% and 43.9%, respectively, while the corresponding data in the AGCS-GC study were 37.6–61.4% and 34.4–50%, respectively. The postoperative DFS and OS of gastric cancer patients in China are still shorter than those in Japan. The possible reasons of these differences are as follows: First, our database includes data from patients all over our country. Although all of our patients underwent D2 radical surgery, the level of surgery procedure varies, which may affect the overall DFS. Second, the economic level and wishes to receive chemotherapy of our patients varied. This made palliative therapy differed a lot when patients were diagnosed relapse or metastasis, which may further impact OS. Besides, our study enrolled only Chinese gastric cancer patients who received adjuvant chemotherapy after D2 gastrectomy. The situations might differ between eastern countries and western countries. An international study with standardized D2 dissection could lead to more valuable research results.
In conclusion, the results of our study showed that the oxaliplatin-based adjuvant chemotherapy regimen was associated with better survival in intestinal type gastric cancer patients after D2 gastrectomy, but not in diffuse type gastric cancer, compared with oxaliplatin-free adjuvant chemotherapy regimen. Oxaliplatin-based adjuvant chemotherapy should be considered preferentially for patients with intestinal type.
References
Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int Cancer. 2015;136(5):E359–86.
Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108.
Gallo A, Cha C. Updates on esophageal and gastric cancers. World J Gastroenterol. 2006;12(20):3237.
Middleton G, Cunningham D. Current options in the management of gastrointestinal cancer. Ann Oncol. 1995;6(suppl_1):17–26.
Bang YJ, Kim YW, Yang HK, et al. Adjuvant capecitabine and oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): a phase 3 open-label, randomised controlled trial. Lancet. 2012;379(9813):315–21.
Noh SH, Park SR, Yang HK, et al. Adjuvant capecitabine plus oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): 5-year follow-up of an open-label, randomised phase 3 trial. Lancet Oncol. 2014;15(12):1389–96.
Shitara K, Chin K, Yoshikawa T, et al. Phase II study of adjuvant chemotherapy of S-1 plus oxaliplatin for patients with stage III gastric cancer after D2 gastrectomy. Gastric Cancer. 2017;20(1):175–81.
Wang G, Zhao J, Song Y, et al. Phase II study of adjuvant chemotherapy with S1 plus oxaliplatin for Chinese patients with gastric cancer. BMC Cancer. 2018;18(1):547.
Yang L, Yang YI, Qin Q, et al. Evaluation of the optimal dosage of S-1 in adjuvant SOX chemotherapy for gastric cancer. Oncol Lett. 2015;9(3):1451–7.
Sasako M, Sakuramoto S, Katai H, et al. Five-year outcomes of a randomized phase III trial comparing adjuvant chemotherapy with S-1 versus surgery alone in stage II or III gastric cancer. J Clin Oncol. 2011;29(33):4387–93.
Sakuramoto S, Sasako M, Yamaguchi T, et al. Adjuvant chemotherapy for gastric cancer with S-1, an oral fluoropyrimidine. N Engl J Med. 2007;357(18):1810–20.
Fujitani K, Tamura S, Kimura Y, et al. Three-year outcomes of a phase II study of adjuvant chemotherapy with S-1 plus docetaxel for stage III gastric cancer after curative D2 gastrectomy. Gastric Cancer. 2014;17(2):348–53.
Lauren P. The two histological main types of gastric carcinoma: diffuse and so-called intestinal-type carcinoma: an attempt at a histo-clinical classification. Acta Pathol Microbiol Scand. 1965;64(1):31–49.
Qiu M, Cai M, Zhang D, et al. Clinicopathological characteristics and prognostic analysis of Lauren classification in gastric adenocarcinoma in China. J Transl Med. 2013;11(1):58.
Liu L, Wang ZW, Ji J, et al. A cohort study and meta-analysis between histopathological classification and prognosis of gastric carcinoma. AntiCancer Agents Med Chem (Former Curr Med Chem AntiCancer Agents). 2013;13(2):227–234.
Tamura S, Fujitani K, Kimura Y, et al. Phase II feasibility study of adjuvant S-1 plus docetaxel for stage III gastric cancer patients after curative D2 gastrectomy. Oncology. 2011;80(5–6):296–300.
Hass HG, Smith U, Jäger C, et al. Signet ring cell carcinoma of the stomach is significantly associated with poor prognosis and diffuse gastric cancer (Lauren’s): single-center experience of 160 cases. Oncol Res Treat. 2011;34(12):682–6.
Chen L, Shi Y, Yuan J, et al. Evaluation of docetaxel-and oxaliplatin-based adjuvant chemotherapy in postgastrectomy gastric cancer patients reveals obvious survival benefits in docetaxel-treated mixed signet ring cell carcinoma patients. Med Oncol. 2014;31(9):159.
Yang XF, Yang L, Mao XY, et al. Pathobiological behavior and molecular mechanism of signet ring cell carcinoma and mucinous adenocarcinoma of the stomach: a comparative study. World J Gastroenterol. 2004;10(5):750.
Yoon C, Cho SJ, Aksoy BA, et al. Chemotherapy resistance in diffuse-type gastric adenocarcinoma is mediated by RhoA activation in cancer stem-like cells. Clin Cancer Res. 2015;22:971–983.
Kakiuchi M, Nishizawa T, Ueda H, et al. Recurrent gain-of-function mutations of RHOA in diffuse-type gastric carcinoma. Nat Genet. 2014;46(6):583.
Zheng Z, Jin X, He Q, et al. The efficacy of taxanes-and oxaliplatin-based chemotherapy in the treatment of gastric cancer after D2 Gastrectomy for different Lauren types. Medicine (Baltimore). 2016;95(6):e2785.
Acknowledgements
This work was supported by the National Nature Science Foundation of China (no. 81702965) and Shanghai Science and Technology Committee (no. 15411961900, no. 17411951400).
Author information
Authors and Affiliations
Contributions
The corresponding author had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. XC and SY contributed significantly to study design, data analysis, interpretation of the data and drafting the manuscript; all authors were involved in developing the original study and protocols. YW, YC, WL, YY, CT, HJ, YJ, YS, XW, ZS, and FL were responsible for the data analysis and interpretation of the data. All authors provided significant input to the paper by means of critical revisions and have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared no conflicts of interest.
Informed consent
All participants included in the study provided written informed consent.
Research involving human participants and/or animals informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and in compliance with the Helsinki Declaration of 1964 and later versions. The Ethics Committee of Zhongshan Hospital Affiliated to Fudan University approved this study. This study does not involve animal study.
Rights and permissions
About this article
Cite this article
Cheng, X., Yu, S., Wang, Y. et al. The role of oxaliplatin in the adjuvant setting of different Lauren’s type of gastric adenocarcinoma after D2 gastrectomy: a real-world study. Gastric Cancer 22, 587–597 (2019). https://doi.org/10.1007/s10120-018-0895-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-018-0895-x