Abstract
Rapid maxillary expansion (RME) is one of the common treatments of transverse maxillary deficiency, and low-level laser therapy (LLLT) is one of the recommended solutions to enhance biological wound or bone healing. This review article aims to answer the following question: “What are the effects of LLLT, on patients who underwent surgical or non-surgical RME, in improving clinical success, wound healing, and bone regeneration?” A search in PubMed, Scopus, Web of Science, and ProQuest databases was performed, with a focus on the appropriate key words. Related articles, up to May 2017, were screened, and the full text of the randomized controlled trials (RCT) were comprehensively read and subjected to quality assessments. A total of 1804 articles were included after the initial search. Four RCTs were eligible in randomization and methodology. The applied wavelength varied from 660 to 830 nm with an output range of 40–100 mW. Also, the highest exposed energy was 420 J/cm2 and the lowest was 100 J/cm2. The exposure time differed from 20 to 84 s in each defined point in the palate. Based on the RCTs available, LLLT is better to be used at initial phase of RME, because it has some benefits in increasing the rate of bone remodeling.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Maxillary constriction can lead to several problems such as poor esthetics, occlusal dis-harmony, narrowed pharyngeal airway, increased nasal resistance and mouth breathing, altered tongue posture, and obstructive sleep apnea [1, 2]. In all malocclusions, transverse discrepancy is the most common problem encountered [3]. Three methods are suggested for treating maxillary constriction: non-surgical orthodontic rapid maxillary expansion (RME), surgically assisted rapid palatal expansion (SARPE), and segmental LeFort osteotomy [4, 5]. RME has become more common due to its many positive effects on general health. Also, dental or skeletal transverse maxillary discrepancies can be remarkably treated by this method [6]. Moreover, RME can improve nasal breathing by increasing the nasopharyngeal airway [7]. For problems such as large transverse discrepancies (> 7 mm), narrow inter-cuspid dimensions, and maxillary arch length deficiency with crowding, the treatment of choice is SARPE [5, 8]. The clinical procedure for maxillary expansion consists of an active phase with induced lateral forces and a passive phase with retainer maintenance [9]. One of the possible encountered obstacles during RME is rapid relapse of treatment (if retainers are not used) [10]. Insufficient bone regeneration in the mid-palatal suture (MPS) is one of the involved causes of relapsed treatments. Therefore, accelerating the bone regeneration in MPS is encouraged by researchers [11].
Low-level laser treatment (LLLT) is a non-invasive treatment that provides low energy outputs and does not increase temperature of the site higher than the natural norms [12]. It provides an inexpensive treatment that can be used in many orthodontic treatments, as it generates an array of transient biochemical factors that result in cascading biological reactions [13]. LLLT has shown promising results in the expression of cytokines and promotion of wound healing, angiogenesis, cell proliferation, and bone repair and remodeling, by increasing collagen production [13,14,15,16,17]. The effect of LLLT on bone remodeling is well-tracked by Noda et al., who claimed that healing of the tooth extraction socket was enhanced by high-frequency pulsed low-level diode laser irradiation [16]. Also, more homogenous trabecular configuration can be achieved by LLLT, after alveolar bone repair, as suggested by Romao et al. [17]. In vivo studies mentioned that LLLT is advantageous during MPS expansion, by accelerating the formation of better bone and osteoclast differentiation [14, 15]. A valuable and comprehensive textbook on the role of laser in dental sciences has been recently released [13]. One of its chapters is devoted to elaborating the influence of laser on orthodontic purposes, such as gingivoplasty, impacted tooth exposure and bracket placement, pain reduction and post-op managements, and tooth movement. Nevertheless, the role of LLLT on RME and further bone regeneration success is not mentioned exactly.
Based on what was mentioned above and recent focus on the benefits of LLLT, as a non-invasive method, the aim of the current review study is to answer the following question: “What are the effects of using LLLT on clinical success, wound healing, and bone regeneration, compared to other possible methods, in patients who underwent surgical or non-surgical RME?” The null hypothesis is that LLLT does not have any positive effects on improving results of RME.
Methods
Study design
To enhance the structural reporting of the articles, the reviewing setting was in accordance to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline [18].
Initially, a clinical question was defined for screening the qualified clinical studies based on PICO: Patients with constricted maxilla (P, population) who underwent LLLT (I, intervention), compared to other methods (C, comparison), following surgical or non-surgical RME, that caused improvements in clinical success, wound healing, and bone regeneration (O, outcome).
A data search was performed using PubMed, Web of Science, Scopus, and ProQuest electronic databases of articles, based on MeSH and non-MeSH terms in simple or multiple conjunctions (Table 1). The search was conducted manually up to May 2017. Then, the Endnote software version 7 (Thomson Reuters, NY, USA) was used for final confirmation, cross matching, and avoiding any missing of data.
Two independent reviewers (A.D. and M.A.) qualified the eligible articles for review. To select the studies, all obtained reports were reviewed, and titles and abstracts were screened for relevance. The review articles and references from different studies were used to identify the relevant articles. In case of disagreement between reviewers, it was discussed until mutual agreement was reached. Reviewers’ agreement was tested with the Cohen κ test using the MedCalc software (MedCalc Software, Ostend, Belgium).
The studies were subjected to modified Jadad Score Calculation for Critical Appraisal, to lower the risk of bias (Table 2) [19]. The full text of relevant abstracts was obtained, and selected using the following inclusion and exclusion criteria.
Inclusion criteria
-
Randomized clinical trials (RCTs) and prospective studies that investigated the effect of LLLT on surgical or non-surgical maxillary expansion.
-
Clinical research on at least five patients
-
Maintaining the standard indications and guidelines of LLLT (like maintaining Helsinki declaration guidelines of clinical trials, using non-toxic chemical agents (if needed), considering non-hazardous energy density during procedure, paying attention to the safety of both the examiners and patients, and preparing follow-up courses after intervention).
-
Performing at least one standard test to evaluate the clinical effects or side effects of LLLT
Exclusion criteria
-
Case reports
-
Animal studies
-
In vitro studies
-
Studies with missing data
-
Repeatedly published studies; the last version was included
-
Studies in languages other than English
-
Studies with Jadad score of < 3 (for eliminating the risk of biases)
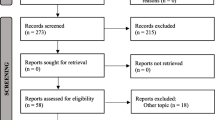
The initial literature search yielded 1804 articles (PubMed, n = 116/Scopus, n = 764/Web of Science, n = 20/ProQuest, n = 904), of which 989 articles remained after removing the duplicates. After initial screening based on the title and abstract, four studies [20,21,22,23] were found eligible to be reviewed (Fig. 1).
Data extraction
The full-text of all articles was reachable for initiating the review process. The following data were collected for each study: author, year, study design, participants (age, gender), diagnosis, details of the administered laser, monitoring tests before and after LLLT, and clinically significant outcomes. After gathering information, the possibility of preparing a meta-analysis was judged by an independent statistician and epidemiologist. As the collected data were vastly heterogeneous, no meta-analysis was prepared.
Results
A total of 1804 articles were included in the study after the initial search, and 989 articles remained after removing the duplicates, of which four studies were eligible to be screened. The full texts of these articles were gathered, and the ones fulfilling the inclusion criteria were taken into account. Relying on the modified Jadad scale (Table 2), three studies with a score of 5 [20, 22, 23] and one with a score of 4 [21] were included for reviewing. None of the studies included were highly potential for risk of bias.
All of the reviewed studies were RCTs on a total of 110 patients, aged ranging from 6 to 33 years (Table 3). Regarding the clinical problem, two studies focused on patients with transverse maxillary deficiency [20, 22], one on Cl I or II malocclusion [23] and one on any kind of RME treatment need [21] (Table 3). One study tried surgical approach alongside RME [20], and the others used non-surgical treatments [21,22,23].
Regarding the treatment methods (Table 4), all of the studies irradiated the palate at 10 [21], 3 [20], or 4 [22] points around MPS; also, one study irradiated 4 intra-suture and 2 extra-suture points in one of their study groups [23]. All studies used the diode laser for irradiation with the applied wavelength varying from 660 to 830 nm, and output range of 40–100 mW. The highest applied energy on the palatal mucosa was 420 J/cm2 [20], and the lowest was 100 J/cm2 [21].
The exposure time was different amongst the studies; Angeletti et al. irradiated LLLT for 84 s in each point (3 points overall, 3 × 84 = 252 s) [20], Garcia et al. used LLLT for 60 s in the intra-suture points (4 × 60 = 240 s) and 30 s in the extra-suture points (2 × 30 = 60 s) [23], and Ferreira et al. used LLLT for 20 s per defined point (4 × 20 = 80 s) [22].
The rate of RME was different amongst the included studies. Two of them administered one full turn screw opening after installation and two half turns daily, until achieving overcorrection [21, 22]. One of them activated the screw a quarter turn (0.20 mm), twice a day, until achieving 50% transversal overcorrection [23], and the last one opened the screw 1.6 mm inter-operatively and twice a day after 4 days’ latency [20]. Cepera et al. found improved MPS opening and accelerated bone regeneration [21]. Angeletti et al. stated that bone regeneration after LLLT following the SARPE approach caused significant mineralization [20]. Both Garcia et al. [23] and Ferreira et al. [22] indicated that LLLT resulted in a better healing process following RME.
Discussion
The data regarding the clinical success of LLLT after RME, relative to either the radiation dose or the number of sessions, seemed to lack validation, since most of the released articles are animal studies [24, 25]. Therefore, the present study tried to comprehensively review valuable clinical studies on this scope.
LLLT has provided several positive impacts on orthodontic science, such as analgesic effects during the orthodontic maintenance phase, better healing of scars caused by orthodontic appliances, and accelerating bone repair [13, 15, 26,27,28]. An in vitro study on biostimulatory effect of LLLT on human osteoblasts showed rapid increase in vascular endothelial growth factor [27]. Also, another study observed an increase in proliferation and phenotypic expression of osteoblast cells (derived from MPS) after LLLT [29]. During the progressive stages of wound stabilization and healing, many cellular and biochemical pathways are potential recipients being activated by low-level laser photonic energy at wavelengths between 600 and 1400 nm [13].
Relying on gathered information from the current review study, the null hypothesis was rejected, since LLLT improved both wound healing and bone regeneration of MPS during and after RME.
Most included studies were on children, except for one study which included youths (18–33 years old) [20]. In adult patients, the MPS is much more mature, with higher integration and interdigitating, so RME is more susceptible to failure; therefore, a surgical-associated approach with RME is required [30]. Angeletti et al. [20] observed the effects of LLLT on bone regeneration in the mid-palatal anterior suture after surgically assisted RME. They used GaAlAs laser (power = 100 mW, wavelength = 830 nm) in eight treatment sessions, with 48-h intervals, on 3 points in MPS (energy density per point = 140 J/cm2). The reason of using GaAlAs laser was based on released animal studies that showed this laser device increased fibroblast proliferation and the amount of osteoid formation during RME [15, 31]. They used digital radiographs (occlusal and periapical) for measuring optical density (OD) of the bone. Although, these radiographs are acceptable for observation [31], cone beam computed tomography (CBCT) seems to be more appropriate. By CBCT, superposition of tissues can be avoided, and the density is more stable and reliable [3]. Back to Angeletti et al.’s study, they claimed that LLLT caused significant increase in bone regeneration after surgically assisted RME.
Ferriera et al. observed the effect of LLLT on bone regeneration of MPS after RME with the aid of CBCT [22]. They administered the Hyrax expander appliance that was activated one full turn after installation, and two half turns daily. All reviewed studies used this expander appliance, as it facilitates LLLT, by not having any acrylic base on the palatal mucosa that interferes with the irradiation process. Ferriera et al. applied LLLT (power = 70 mW, wavelength = 780 nm) with 35 J/cm2 dose on 4 points of the MPS, twice a week in the first month, and once a week in the second month (total applied dose = 140 J/cm2). After 12 sessions of LLLT, the bone regeneration of MPS was evaluated by measuring OD of the prepared CBCT. They scheduled a 4-month retention period, which is in the appropriate range required for new bone formation (3–6 months) [32]. In summary, their final results showed significant improvement in bone regeneration of MPS.
In another study, conducted by Cepera et al. [21], the role of LLLT on bone regeneration of MPS was evaluated after RME. The expansion protocol was one full turn screw opening on the first day, and a half turn daily. The applied LLLT device was adjusted on 780-nm wavelength and 40-mW power (similar to Ferriera et al. [22]), with 10 J/cm2 density, at 10 points located around the MPS. The LLLT sessions were defined as follows: stage 1: days 1–5 of activation; stage 2: at screw locking, on 3 consecutive days; stage 3, 4, and 5: 7, 14, and 21 days after stage 2. The retention phase was 90 days in this study (about 3 months). They used occlusal radiographs for measuring the OD, and the analyzed data showed that LLLT improved opening of the MPS and the bone regeneration process [21]. The interpretation of OD at different stages of LLLT revealed that: during stage 1 to 2, OD of the LLLT group was significantly lower than the control group, which suggests facilitation in opening the MPS. This result was consistent with Sasaki et al.’s study who claimed that laser accelerates opening of the suture [33]. Also, another animal study showed that LLLT has a paramount role in bone regeneration of MPS, especially in the initial phase that can accelerate suture opening [15]. LLLT may stimulate the osteoblast cells and lead to reduced unwanted buccal orthodontic movements of the supporting tooth [34]. During stages 2–3 and 3–4, no significant differences were found between the test group and controls. During the last phase of the experiment, stages 4–5, higher OD was found in the laser-treated group, meaning higher level of bone regeneration [21].
Garcia et al. observed the influence of LLLT on the repair of MPS after RME [23]. They applied LLLT with 660-nm wavelength, 100 -W power, and 332-mW/cm2 energy [23] that were different from previous studies [21, 22]. They irradiated 4 points along the MPS for 60 s and each side of the suture for 30 s [23]. Also, seven LLLT sessions were scheduled on days 1, 7, 14, 28, 42, 56, and 70 of the retention phase. They traced CBCT radiographs for measuring OD of MPS [23]. Their quantitative measurements seemed to be more precise than the previously mentioned studies [21, 22]. They measured the following distances: anterior-inferior suture distance, posterior-superior suture distance, and anterior nasal spine suture distance. After separation of MPS, bone resorption, bone regeneration, and fiber rearrangement continue to regain architectural equilibrium [35, 36]. They applied 660-nm wavelength, instead of 780 nm, as Sasaki et al. showed this wavelength can promote mitochondrial enzymes and accelerates tissue repair [33]. However, our reviewer’s search on recently published studies lead to controversial results, as some studies believed 810- [36] or 830-nm [37] wavelengths are more effective in both wound healing and bone regeneration, since they are in the absorption spectrum of cytochrome c oxidase (the candidate mitochondrial chromophore in LLLT) [37]. Garcia et al. [23] did not apply LLLT during the activation phase of expansion, as the patients were younger than Cepera et al.’s study [21], and it was more convenient to irradiate only during the retention phase (seven times in 75 days), similar to Angeletti et al.’s study [20], with eight times irradiation during a retention phase of 39 days. Garcia et al. irradiated the anterior side of MPS more, because the separation seemed to be greater in the triangular-shaped front area, with a wider base at the front portion of the jaw [38]. Nevertheless, a recent systematic review concluded that the available data on MPS opening are not decisive, and it can be parallel or triangular [39]. In summary, their final results revealed that the LLLT group showed more approximation of bone zones in the anterior, posterior, and superior suture with less approximation in the posterior superior suture, than the control group after 75 days.
Conclusion
One of the most important limitations of this was heterogeneity of the included studies, as one was in post-treatment retention, one on young adults as opposed to another on children. Also, there was no consistency of wavelengths, frequency, and mode of application or dosimetry. Although most of the studies on this scope are largely inferential on in vitro and animal studies, the following statements may be concluded at this level of evidences provided by the four RCTs mentioned:
-
LLLT is better to be administered at the initial phase of mid-palatal expansion, if it is applicable, because it has some benefits in increasing the rate of bone remodeling.
-
The wavelength and power of the irradiated laser was different amongst the included studies, but 780 nm was used in two of them.
-
The irradiation points differed amongst reviewed studies, but all of them applied LLLT along the MPS in at least 3 or 4 points.
-
LLLT may also have some benefits in increasing the rate of bone deposition in RME; however, more studies are required to make a determinant decision.
Finally, LLLT may be helpful for RME, since it has no side effects, is financially affordable, and requires a short application time. Nevertheless, applying other wavelengths, power, and energy of LLLT, and surveying other biological responses (like pain and edema) and biological factors, are recommended for future investigations. Also, it would be more desirable to use CBCT instead of conventional radiographs for measurements, as it provides better results.
References
Aloufi F, Preston CB, Zawawi KH (2012) Changes in the upper and lower pharyngeal airway spaces associated with rapid maxillary expansion. ISRN Dent 2012
Jr CM, Alves FEMM, Nagai LHY, Fujita RR, Pignatari SSN (2017) Impact of rapid maxillary expansion on nasomaxillary complex volume in mouth-breathers. Dental Press J Orthod 22:79–88
Franchi L, Baccetti T (2005) Transverse maxillary deficiency in class II and class III malocclusions: a cephalometric and morphometric study on postero-anterior films. Orthod Craniofac Res 8:21–28
McNamara Jr JA, Baccetti T, Franchi L, Herberger TA (2003) Rapid maxillary expansion followed by fixed appliances: a long-term evaluation of changes in arch dimensions. Angle Orthod. 73:344–353
Suri L, Taneja P (2008) Surgically assisted rapid palatal expansion: a literature review. Am J Orthod Dentofac Orthop 133:290–302
Bucci R, D'Anto V, Rongo R, Valletta R, Martina R, Michelotti A (2016) Dental and skeletal effects of palatal expansion techniques: a systematic review of the current evidence from systematic reviews and meta-analyses. J Oral Rehabil 43:543–564
Halicioğlu K, Kiliç N, Yavuz İ, Aktan B (2010) Effects of rapid maxillary expansion with a memory palatal split screw on the morphology of the maxillary dental arch and nasal airway resistance. Eur J Orthod 32:716–720
Silverstein K, Quinn PD (1997) Surgically-assisted rapid palatal expansion for management of transverse maxillary deficiency. J Oral Maxillofac Surg 55:725–727
Romanyk DL, Lagravere MO, Toogood RW, Major PW, Carey JP (2010) Review of maxillary expansion appliance activation methods: engineering and clinical perspectives. J Dent Biomech 2010
Marini I, Bonetti GA, Achilli V, Salemi G (2007) A photogrammetric technique for the analysis of palatal three-dimensional changes during rapid maxillary expansion. Eur J Orthod 29:26–30
Saito S, Shimizu N (1997) Stimulatory effects of low-power laser irradiation on bone regeneration in midpalatal suture during expansion in the rat. Am J Orthod Dentofac Orthop 111:525–532
Moskvin SV (2017) Low-level laser therapy in Russia: history, science and practice. J Lasers Med Sci 8:56–65
Borzabadi-Farahani A, Cronshaw M (2017) Lasers in orthodontics. In: Coluzzi D, Parker S (eds) Lasers in dentistry-current concepts, 1st edn. Springer International Publishing, pp 248–271
Bouvet-Gerbettaz S, Merigo E, Rocca JP, Carle GF, Rochet N (2009) Effects of low-level laser therapy on proliferation and differentiation of murine bone marrow cells into osteoblasts and osteoclasts. Lasers Surg Med 41:291–297
Saito S, Shimizu N (1997) Stimulatory effects of low-power laser irradiation on bone regeneration in midpalatal suture during expansion in the rat. Am J Orthod Dentofac Orthop 111:525–532
Noda M, Aoki A, Mizutani K, Lin T, Komaki M, Shibata S et al (2016) High-frequency pulsed low-level diode laser therapy accelerates wound healing of tooth extraction socket: an in vivo study. Lasers Surg Med 48:955–964
Romão M, Marques M, Cortes A, Horliana A, Moreira M, Lascala C (2015) Micro-computed tomography and histomorphometric analysis of human alveolar bone repair induced by laser phototherapy: a pilot study. Int J Oral Maxillofacl Surg 44:1521–1528
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097
Augestad KM, Berntsen G, Lassen K, Bellika JG, Wootton R, Lindsetmo R-O et al (2011) Standards for reporting randomized controlled trials in medical informatics: a systematic review of CONSORT adherence in RCTs on clinical decision support. J Am Med Inform Assoc 19:13–21
Angeletti P, Pereira MD, Gomes HC, Hino CT, Ferreira LM (2010) Effect of low-level laser therapy (GaAlAs) on bone regeneration in midpalatal anterior suture after surgically assisted rapid maxillary expansion. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 109:e38–e46
Cepera F, Torres FC, Scanavini MA, Paranhos LR, Capelozza Filho L, Cardoso MA et al (2012) Effect of a low-level laser on bone regeneration after rapid maxillary expansion. Am J Orthod Dentofac Orthop 141:444–450
Ferreira FNH, Gondim JO, Neto JJSM, Santos PCF, Pontes KMF, Kurita LM et al (2016) Effects of low-level laser therapy on bone regeneration of the midpalatal suture after rapid maxillary expansion. Lasers Med Sci 31:907–913
Garcia VJ, Arnabat J, Comesaña R, Kasem K, Ustrell JM, Pasetto S et al (2016) Effect of low-level laser therapy after rapid maxillary expansion: a clinical investigation. Lasers Med Sci 31:1185–1194
de Braekt MM, van Alphen FA, Kuijpers- Jagtman AM, Maltha JC (1991) Effect of low level laser therapy on wound healing after palatal surgery in beagle dogs. Lasers Surg Med 11:462–470
Rosa CB, Habib FAL, de Araújo TM, Aragão JS, Gomes RS, Barbosa AFS et al (2014) Effect of the laser and light-emitting diode (LED) phototherapy on midpalatal suture bone formation after rapid maxilla expansion: a Raman spectroscopy analysis. Lasers Med Sci 29:859–867
Grassi FR, Ciccolella F, D'Apolito G, Papa F, Iuso A, Salzo AE et al (2011) Effect of low-level laser irradiation on osteoblast proliferation and bone formation. J Biol Regul Homeost Agents 25:603–614
Parenti SI, Checchi L, Fini M, Tschon M (2014) Different doses of low-level laser irradiation modulate the in vitro response of osteoblast-like cells. J Biomed Opt 19:108002
Soleimani M, Abbasnia E, Fathi M, Sahraei H, Fathi Y, Kaka G (2012) The effects of low-level laser irradiation on differentiation and proliferation of human bone marrow mesenchymal stem cells into neurons and osteoblasts—an in vitro study. Lasers Med Sci 27:423–430
da Silva APRB, Petri AD, Crippa GE, Stuani AS, Stuani AS, Rosa AL et al (2012) Effect of low-level laser therapy after rapid maxillary expansion on proliferation and differentiation of osteoblastic cells. Lasers Med Sci 27:777–783
Aloise AC, Pereira MD, Hino CT, Gragnani Filho A, Ferreira LM (2007) Stability of the transverse dimension of the maxilla after surgically assisted rapid expansion. J Craniofac Surg 18:860–865
Takeda Y (1988) Irradiation effect of low-energy laser on alveolar bone after tooth extraction. Experimental study in rats. Int J Oral Maxillofac Surg 17:388–391
Pereira MD, Prado GPR, Abramoff MMF, Aloise AC, Ferreira LM (2010) Classification of midpalatal suture opening after surgically assisted rapid maxillary expansion using computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 110:41–45
Sasaki A, Touma Y, Ishino Y, Tanaka E, Aoyama J, Hanaoka K et al (2003) Linear polarized near-infrared irradiation stimulates mechanical expansion of the rat sagittal suture. Luminescence 18:58–60
Garib DG, Henriques JFC, Janson G, Freitas MR, Coelho RA (2005) Rapid maxillary expansion—tooth tissue-borne versus tooth-borne expanders: a computed tomography evaluation of dentoskeletal effects. Angle Orthod 75:548–557
Amid R, Kadkhodazadeh M, Ahsaie MG, Hakakzadeh A (2014) Effect of low level laser therapy on proliferation and differentiation of the cells contributing in bone regeneration. J Lasers Med Sci. 5:163–170
Barbosa D, Villaverde AGJB, Loschiavo Arisawa EÂ, RAd S (2014) Laser therapy in bone repair in rats: analysis of bone optical density. Acta Ortop Bras 22:71–74
Gupta A, Dai T, Hamblin MR (2014) Effect of red and near-infrared wavelengths on low-level laser (light) therapy-induced healing of partial-thickness dermal abrasion in mice. Lasers Med Sci 29:257–265
Wehrbein H, Yildizhan F (2001) The mid-palatal suture in young adults. A radiological-histological investigation. Eur J Orthod 23:105–114
Liu S, Xu T, Zou W (2015) Effects of rapid maxillary expansion on the midpalatal suture: a systematic review. Eur J Orthod 37:651–655
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study followed the PRISMA guideline, and no ethical approval was required.
Rights and permissions
About this article
Cite this article
Davoudi, A., Amrolahi, M. & Khaki, H. Effects of laser therapy on patients who underwent rapid maxillary expansion; a systematic review. Lasers Med Sci 33, 1387–1395 (2018). https://doi.org/10.1007/s10103-018-2545-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-018-2545-2