Abstract
Thermal relaxation times were introduced into modern skin-laser science with the inception of selective photothermolysis. As a result, laser pulsewidths were determined according to the thermal relaxation times of the tissue targets. The Arrhenius Damage Integral shows that this approach is incorrect. The important parameter is the time required to induce irreversible protein denaturation within the target. This time is determined by the tissue’s intrinsic structure, not its physical dimensions. This report explains why thermal relaxation times should not be considered when treating many skin conditions with lasers or IPL systems.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Selective photothermolysis (SPT) has been the cornerstone of many modern-day dermatology laser procedures since its inception in 1981 [1, 2]. This theory was constructed at a time when short-pulsed lasers were being developed for vascular conditions. Anderson and Parrish identified the problems with older technology and redefined the concept of acceptable clinical results following laser interventions.
A major part of SPT was the definition of thermal relaxation time (TRT). This was used to determine the maximum allowable pulsewidths to be used on blood vessels while minimising thermal injury to adjacent tissue. The TRT was defined as the time taken ‘for the central temperature of a Gaussian temperature distribution with a width equal to the target’s diameter to decrease by 50 %’ and is calculated (in cylinders as a first approximation) as follows:
Where d is the target diameter (in millimetre) and α is the tissue diffusivity (in square millimetre per second). The theory of SPT proposes that minimal collateral thermal damage is achievable if the laser energy is delivered within this time.
Hence, a pulse of energy is applied to the skin surface with a duration calculated according to the diameter of the target tissue. When considering relaxation times, Anderson and Parrish were solely concerned with minimising collateral thermal damage to the dermis surrounding the target blood vessels.
This definition was extended by Altshuler et al. [3] in 2001 to include hair follicles, under the same principles as SPT, whereby target structures are denatured or destroyed by heat energy diffusing from adjacent light energy-absorbing chromophores in the hair shaft (absorber) rather than by direct absorption in the outer root sheet (target). To their surprise, they found experimentally that selective photothermal damage of hair follicles occurred even for radiant pulse durations five to seven times longer than the TRT of the hair follicle, which they could not explain. Haemoglobin and melanin are the light-absorbing targets in blood vessels and hair, respectively. Their temperatures become elevated and these heat sources conduct thermal energy to the target tissues—the vessel walls and hair germ cells [3]. The authors defined a new time—the ‘thermal damage time’ as the time when the outermost part of the target reaches the target damage temperature through heat diffusion from the heater (tissue), but this heat diffusion model does not explain why selective damage can occur even though the pulse duration is much longer than the TRT of the follicles.
Both reports determine ‘appropriate’ energy pulsewidths according to the relaxation (or damage) times of the targets, based on their diameters. Neither report discusses the requirement that tissues must be maintained at a particular temperature for a particular time. This is an intrinsic requirement to ensure complete and permanent destruction of the target cells.
The Arrhenius damage integral—application to tissue
There are at least two processes which occur during the irradiation of tissue. The first is the thermodynamic heating process which results in a local temperature rise. The second is a chemical process whereby the heated proteins denature resulting in a loss of their integrity.
Below boiling point, temperature-induced damage of tissue typically involves denaturation of the proteins which constitute the tissue. The rate of denaturation is a complicated function of temperature, local pressure, and other environmental parameters. Slow heating of proteins will cause denaturation at a lower temperature than rapid heating of the same proteins. The thermally induced denaturation of human cells starts at temperatures as low as approximately 43 °C [4]. This is due to the thermal rate constants governing the thermodynamic process. An approximation in calculating the amount of tissue damage may be found from the first-order Arrhenius rate theory model, as proposed by Henriques and Moritz [5, 6].
For clarification, this model is based on the well-known physical processes where light energy (in joules) is absorbed by tissue chromophores which results in heat formation leading to local temperature increases (in degrees Celsius). Hence, increasing the incident radiant exposure (commonly known as ‘fluence’ or ‘energy density’) ultimately induces higher temperatures in tissues (for a given pulsewidth). In many cases, there is an almost linear relationship between the incident optical radiant exposure (in joules per square centimetre) and the local temperature rise (ΔT) under the assumption that non-linear processes, such as phase changes like vapourisation etc., are not taking place.
This model asserts that tissue damage can be expressed as a function of a chemical rate process where damage is proportional to the rate of denaturation of proteins, k. The amount of accumulated damage depends on the protein temperature, T, and the heating time, t.
The amount of tissue damage, Ω per unit time Δt, at any point can be calculated from the Arrhenius damage equation as follows:
which in the general case, with time dependent temperature, becomes:
Where ‘Ω’ is the total accumulated tissue damage, ‘t’ is the total denaturation time (i.e. T(τ) ≥ 43 °C for 0 ≤ τ ≤ t), ‘A’ is the frequency of decomposition of the molecules (or damage rate factor, s−1), ‘Ea’ is the activation energy per mole between the native and the denatured states of tissue (in joules per mole), ‘T’ is the tissue temperature (in degrees Kelvin, K) and ‘R’ is the molar gas constant (8.314 J/mol K). This model is based on the tissue molecules absorbing an amount of energy reaching Ea followed by decomposition of the molecules (denaturation) at a rate determined by A. The terms Ea and A are generally known as the ‘Arrhenius parameters’. Denaturation of the proteins cannot begin until the required denaturation temperature has been reached in the tissue, which is achieved when the appropriate amount of energy (the barrier energy Ea) has been delivered to the tissue. The value of Ea has been found to vary considerably between different tissue types.
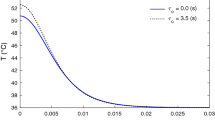
There are several times which are important in this discussion (Fig. 1). The first is the duration of the radiant pulse of light energy—the pulsewidth, tp. This time determines the overall energy input into the absorbing tissues. The second time is the total duration time of the denaturation process within the heated target tissue—‘t’ in Eq. 3. At slow heating rates with “steady-state” thermal conditions, t and tp are approximately equal, and it is fairly straightforward to calculate the damage rate Ω versus time and temperature using the simplified ‘linear’ version of the Arrhenius equation, see Eq. 4 and Discussion below. However, in typical laser/intense pulsed light (IPL) treatments, the thermal process is highly dynamic and transient and the denaturation rate must be calculated with the general Arrhenius equation according to Eq. 3. In the general case, the total denaturation time ttden corresponds to the time when the T > 43 °C. If the peak temperature of the transient process is considerably higher than 43 °C, it may be appropriate to introduce the concept an effective denaturation time teden and corresponding effective (or ‘threshold’) temperature Teden over which, say, 99 % of the denaturation takes place, see Fig. 1. As the denaturation rate accelerates exponentially with increasing temperature, the effective denaturation time can end up being much shorter than the total denaturation time, but still only leading to a 1 % error in the calculated value of the denaturation rate Ω. There exists no simple relationship between the thermal relaxation time tTRT of a heated tissue structure and the effective denaturation time teden for transient heating processes.
Once T ≥ 43 °C in the target tissue, the denaturation process starts up slowly and continues for the total denaturation time ttden. However, the denaturation process accelerates exponentially with increasing temperature, and, therefore, it is useful to introduce the ‘effective’ denaturation temperature, Teden, and corresponding time teden over which most of the denaturation takes place
In some applications (steady state), it may be appropriate to assume that the temperature is constant over the heating period Δt and the first order approximation of Eq. 3 becomes:
This equation describes the rate of denaturation of the tissue as a linear function of time, Δt, and decomposition factor, A, and is exponentially dependent on the tissue temperature, T, and the activation energy, Ea.
The definition of Ω = 1 is taken as being the threshold for irreversible protein denaturation [7], which corresponds to a quantity of 63.2 % cell damage. Hence, once 63.2 % of the cells in a target have been damaged irreversibly, that target is deemed to be incapable of protein re-naturation or regrowth. (Note: Δt is NOT necessarily equivalent to the pulsewidth of the light source in this discussion but is the minimum time that the temperature T is equal or greater than the ‘threshold’ denaturation temperature, Ta, necessary to ensure irreversible denaturation: Ω = 1).
For example at T = 60 °C, the required heating time is approximately Δt = 1 s for human bulk skin, while the required heating time is around 33 ms at a constant temperature of T = 70 °C, which is commonly accepted a ‘standard’ denaturation temperature in the literature for most tissue types.
However, the Arrhenius coefficients vary substantially between different types of tissues. The blood requires much longer heating time (or a higher temperature for a given heating time) to coagulate in comparison with bulk skin. For example, the required temperature for blood coagulation (Ω = 1) is approximately 90.4 °C at Δt = 33 ms, compared with 70 °C for bulk skin, and approximately 88 °C for arterial collagen (see Fig. 2).
Tissue denaturation temperature dependency versus time predicted by the Arrhenius model for bulk skin, blood and arterial collagen. Arrhenius coefficients used for bulk skin (Weaver [9]) Ea = 3.27 × 105 J/mol, A = 1.823 × 1051 s−1, and for blood (Lepock [9]) Ea = 4.55 × 105 J/mol, A = 7.6 × 1066 s−1, and for arterial collagen (Agah [10]) Ea = 4.3 × 105 J/mol, A = 5.6 × 1063 s−1
Arterial collagen denatures at slightly lower temperatures than blood, for a given heating time, leading to a breakdown of the vessel walls before haemoglobin denaturation (Fig. 2). Longer pulsewidths clearly induce perivascular collagen injury [8] which appears to aid the overall result.
An Ω greater than 1 represents a greater percentage of damaged cells; Ω = 2 is 86.5 % cell damage, while Ω = 3 is 95.0 %. Hence an Ω greater than 1 is not undesirable. In a clinical setting, this can be achieved by either increasing the energy applied to the tissues or increasing the pulsewidths, or both.
Tissue denaturation time
The Arrhenius equation (Eq. 4) shows that the denaturation temperature, T, is closely linked to the denaturation time, Δt. In fact, the two parameters are tied—one cannot quote a denaturation temperature without quoting the associated time. One without the other is meaningless—they are an intrinsically coupled pair.
In a clinical setting, this means that merely achieving a desired temperature in a target tissue is not sufficient. That temperature must be maintained for a suitable time, Δt, to ensure irreversible denaturation of the tissue cells and, hence, a permanent clinical result.
This is contrary to the theory of SPT and relaxation times. In SPT, only the thermodynamic process is considered. The denaturation process is not considered, and hence the time which the tissue temperature is maintained is not indicated as important. Instead, the ‘important’ time is the thermal relaxation time, which is merely a function of the target’s diameter and local thermal diffusivity. This relaxation time, which essentially describes the cooling time of an object, has no relation to the tissue’s protein breakdown rate. Instead, the complete temporal, transient temperature history of the target tissue volume has to be considered and calculated using the general expression of the Arrhenius according to Eq. 3.
The thermal relaxation time does not consider the actual physical processes within the tissues. Hence, it cannot be used to determine the most appropriate ‘heating time’ necessary to achieve the desired result. The Arrhenius equation must be used for that purpose, since it links the tissue temperature and the protein destruction rate. In fact, the Arrhenius equation is the most important consideration for any photothermal process, regardless of the energy source (laser, IPL or RF). Note that the Arrhenius equation has no direct dependency on the physical size of the target tissue.
The peak temperature in any absorbing tissue depends on the rate of increase of temperature due to the incoming light energy, and the rate of decrease of temperature due to heat conduction from the tissue. Hence small targets, with inherently rapid heat loss, will not reach high temperatures unless the pulsewidth is very short (tp ≤ TRT), while larger targets will retain their heat energy for longer and subsequently achieve higher temperatures. As a consequence, larger targets will be more likely to achieve Δt and hence irreversible denaturation, given sufficient energy.
Laser treatment of blood vessels
Vessel diameters in PWS typically range from 10 to 300 μm [11] with a commensurate range of TRTs spanning three orders of magnitude from 0.057 to 51 ms (assuming a diffusivity of skin, αs, of 0.114 mm2/s). Pulsed dye lasers were used at the time of the formulation of the SPT theory to treat PWS with typical pulsewidths between 0.0003 and 0.36 ms.
Clinical researchers soon found the limitations of these devices with reports of ‘resistant vessels’ which did not respond to the treatment parameters available [12, 13]. Given the analysis above, this is not surprising. In arterial collagen, denaturation times less than 0.36 ms would require temperatures in excess of 99.4 °C to achieve irreversible thermal denaturation of the vessel walls; blood would require temperatures greater than 101 °C. Instead, the high peak powers of these short pulses typically result in short-lived temperatures at or above boiling point which can induce intravascular cavitation, with subsequent vessel wall rupture and purpura [8]. The early pulsed dye lasers simply could not denature arterial collagen or blood, since they were not capable of generating sufficiently long-lived temperatures in those tissues.
The smallest diameter targets which can be irreversibly denatured may be determined by the applying highest possible temperature in that target tissue, using Eq. 4. In arterial collagen, this is just below 100 °C which corresponds to a denaturation time of 0.296 ms. This time corresponds to the TRT of a vessel diameter of 25.5 μm, meaning that vessels below this diameter cannot be denatured by photothermal exposure.
Hence, it is impossible to destroy such small vessels using the photothermal process. They may only be destroyed by vapourising the vessel walls, but this is not guaranteed, since the vessels may retain the capacity to re-grow.
Consequently, results from the earliest pulsed dye lasers must have been entirely due to the physical destruction of the vessel walls rather than thermal denaturation, a photomechanical process similar to laser tattoo removal.
Modern pulsed dye lasers typically use pulsewidths between 1.5 and 10 ms. These corresponds to a denaturation temperature range of 90.7 to 95.7 °C. Assuming the output pulses are continuous, this range of pulsewidths should be able to denature vessels diameters up to approximately 150 μm, but not above. As with the above situation with small vessel diameters, a pulsewidth of 10 ms cannot denature vessels larger than 150 μm in diameter because of the lack of available time above the threshold temperature for denaturation to progress (see Fig. 2).
It is clear from this analysis that the energy pulsewidth must be calculated according to the absorber/target dimensions to ensure irreversible denaturation, with larger targets requiring longer pulsewidths.
Parlette [8] showed that longer pulses (40–60 ms) yielded better clinical results than shorter pulses (<20 ms) with less purpura and post-inflammatory hyperpigmentation in leg veins up to 1.6-mm diameter treated with an Nd:YAG laser at 1,064 nm. Their histological examination clearly showed contraction of the blood vessels with perivascular collagen damage. The longer pulsewidths resulted in ‘better vessel clearance’ which agrees with the above discussion that longer times are required to ensure irreversible denaturation. The histology did not reveal extensive damage in the surrounding dermis even though the pulsewidths were considerably longer than the TRTs of the smaller vessels.
Current IPL technology routinely uses pulsewidths from typically 5 ms up to 250 ms to successfully treat vascular conditions. There are several clinical reports where IPL systems have been compared with pulsed dye lasers in treatments of PWS, and in many cases, both clinical results and side effects are in favour of IPL sources [14, 15]. These pulsewidths correspond to a denaturation temperature range between 82.7 and 92.5 °C—a more gentle heating regime than with short pulsed lasers and which explains the lack of purpura with IPLs, since intravascular cavitation is avoided. Another benefit of using a ‘long’ pulsed light source is the reduced risk of adverse superficial skin burning in darker skin types if the light source is combined with a means for sufficient parallel skin cooling. Longer pulses allow excessive heat in epidermis to be drained by the heat sink during the pulse. The TRT of 80–100 μm thick epidermis is in the range of 5–10 ms which implies that parallel cooling of skin would be beneficial for pulsewidths longer than 10 ms.
The SPT theory suggests that such long pulsewidths, typically used in treatments with IPLs, should result in excessive collateral tissue damage, yet the clinical results show otherwise [16]. To take advantage of the Arrhenius equation, light-based therapies need to be able to induce constant temperature profiles in absorbing tissues. Such profiles would require complex pulse-forming systems to generate the necessary light pulse with the correct temporal profile.
Conclusion
Thermal relaxation times have been used to determine laser pulsewidths since the concept of SPT was introduced. However, the theory behind TRTs was solely concerned with the diffusion of heat energy from blood vessels into the surrounding dermis.
The Arrhenius equation shows, very clearly, that this is incorrect when considering the destruction of those target vessels. Irreversible denaturation of tissue is only possible when the required temperature is maintained for the required time. The cooling time of the target tissue is irrelevant with smaller vessel diameters when considering the target’s destruction, but become more relevant as the diameters increase. In contrast, energy levels and pulsewidths should be calculated according to the tissue’s intrinsic Arrhenius parameters to ensure irreversible denaturation, and hence successful clinical results.
In reality, the light-absorption profiles, tissue geometry, heat conduction from absorber to target tissues and the light device output temporal profiles all have an effect on this issue. Tissue denaturation will actually begin in the range from 60 to 80 °C, although little damage will occur within acceptable timescales. Clinical results are certainly achievable with current technologies in the range from 80 to 90 °C using properly controlled pulsewidths.
Ideally, technologies could be modified to deliver pulse energies and pulsewidths based on the Arrhenius equation to generate clinically useful temperature/time combinations in tissue which result in good clearance rates while minimising collateral damage.
A deeper analysis of this topic shows that the recommended pulse durations according to the original TRT concept are generally too short to achieve controlled and predictable clinical results. Very short pulse durations often lead to non-linear reactions such as tissue boiling and/or explosive responses that generally induce unexpected side effects and unpredictable clinical results.
References
Anderson RR, Parrish JA (1981) Microvasculature can be selectively damaged using dye laser: a basic theory and experimental evidence in human skin. Lasers Surg Med 1(3):263–76
Anderson RR, Parrish JA (1983) Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. Science 220:524–527
Altshuler GB, Anderson RR, Manstein D, Zenzie HH, Smirnov MZ (2001) Extended theory of selective photothermolysis. Lasers Surg Med 29:416–432
Mark W. Dewhirst, DVM, PhD, Ellen Jones, MD, PhD, Thaddeus Samulski, PhD, Zeljko Vujaskovic, MD, PhD, Chuan Li, PhD, and Leonard Prosnitz, MD. (2003) The Biology of Hyperthermia, Holland-Frei Cancer Medicine, 6th Edition
Henriques FC, Moritz AR (1947) Studies of thermal injury, 1. The conduction of heat to and through skin and the temperature attained therein. A theoretical and an experimental investigation. A J Pathol 23:531–549
Moritz AR, Henriques FC (1947) Studies of thermal injury, 2. The relative importance of time and surface temperature in the causation of cutaneous burns. A J Pathol 23:695–720
Diller KR, Pearce JA (1999) Issues in modelling thermal alterations in tissues. Ann NY Acad Sci 888:153–164
Parlette EC, Groff WF, Kinshella MJ, Domankevitz Y, O’Neill J, Ross EV (2006) Optimal pulse durations for the treatment of leg telangiectasias with a neodymium YAG laser. Lasers Surg Med 38(2):98–105
Thomsen S, Peare JA (2011) Thermal damage and rate processes of biological tissues. In Welch AJ, van Gemert MJC (editors). Optical-thermal response of laser-irradiated tissue, 2nd ed, Chapter 13, page 535).
Agah R (1994) John A Pearce, Ashley J Welch, Massoud Motamedi. Rate process model for arterial tissue thermal damage: Implications on vessel coagulation. Lasers Surg Med 15(2):176–184
Majaron B, Nelson JS. Laser treatment of Port Wine Stains. In Welch AJ, van Gemert MJC (editors). Optical-thermal response of laser-irradiated tissue, 2nd ed, Chapter 23, page 879).
Selim MM, Kelly KM, Nelson JS et al (2004) Confocal microscopy study of nerves and blood vessels in untreated and treated port wine stains: preliminary observations. Dermatol Surg 30(6):892–897
Lanigan SW (1998) Port-wine stains unresponsive to pulsed dye laser: explanations and solutions. Br J Dermatol 139:173–177
Michael Drosner et. al. (2008) Comparison of intense pulsed light (IPL) and pulsed dye laser (PDL) in port-wine stain treatment Medical Laser Application 23 (3): 133–140. (http://www.sciencedirect.com/science/article/pii/S161516150800046X)
Babilas P. et.al. (2010) Split-face comparison of intense pulsed light with short- and long-pulsed dye lasers for the treatment of port-wine stains. Lasers Surg. Med. 42(8): 720–7. http://www.ncbi.nlm.nih.gov/pubmed/20886506
Behrooz Barikbin, Azin Ayatollahi, Somayeh Hejazi, Zahra Saffarian, Sara Zamani. (2011) The Use of Intense Pulsed Light (IPL) for the Treatment of Vascular Lesions, Journal of Lasers in Medical Sciences, 2: 2, Spring
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Murphy, M.J., Torstensson, P.A. Thermal relaxation times: an outdated concept in photothermal treatments. Lasers Med Sci 29, 973–978 (2014). https://doi.org/10.1007/s10103-013-1445-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-013-1445-8