Abstract
Atrophic facial scars which commonly occur after inflammatory acne vulgaris can be extremely disturbing to patients both physically and psychologically. Treatment with fractional laser devices has become increasingly popular, but there has been disappointment in terms of effectiveness. The objective of this study was to assess the safety and efficacy of ablative full-face resurfacing on atrophic acne scars in the Korean population. A total of 22 patients, aged 25–44 years, underwent a new modality of resurfacing combining both short-pulsed and dual-mode erbium:yttrium–aluminum garnet (Er:YAG) laser. The patients had Fitzpatrick skin types ranging from III to V. Photographs were taken before and up to 6 months after treatment. Results were evaluated for the degree of clinical improvement and any adverse events. Degree of improvement was graded using a four-point scale: poor (1) = <25 %, fair (2) = 25–50 %, good (3) = 51–75 %, and excellent (4) = >75 %. Based on the blinded photo assessments by two independent reviewers, clinically and statistically significant mean improvement of 3.41 was observed (one-sample Wilcoxon signed rank test, P < 0.001). Complete wound healing occurred between 6 and 9 days. Erythema occurred in all patients and lasted longer than 3 months in two patients (9.1 %). Postinflammatory hyperpigmentation occurred in ten patients (45.5 %) and lasted longer than 3 months in one patient (4.5 %). One patient experienced mild hypopigmentation (4.5 %). Mild to moderate acne flare-up occurred in five patients (22.7 %). No other adverse effects were observed. A new modality of Er:YAG laser resurfacing combining short-pulsed and dual-mode Er:YAG laser is a safe and very effective treatment modality for atrophic facial acne scars in Asians with darker skin tones.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Atrophic acne scars are the result of a deviation in the orderly pattern of healing and can cause significant psychosocial distress. With the huge cosmetic discomfort felt by patients, the demand for therapeutic intervention is high. Among the various treatment options, laser resurfacing has been acknowledged as a precise, well-tolerated procedure with clinically demonstrable efficacy. Accordingly, the last 20 years has seen a dramatic evolution in laser treatment of acne scars, spanning ablative and non-ablative technologies, to the current popularity of fractional laser scar revision.
Since their first introduction in 2004 [1], ablative fractional laser devices have been expected to offer the potential benefits of full-surface ablative skin resurfacing while minimizing risk and recovery time. However, fractional resurfacing, in reality, does not reach the efficacy of conventional ablative laser treatment, especially in more severe grades of scarring [2, 3]. Besides, the benefits of fractional lasers are not sufficient under efficacious parameters. Safety is still a concern in Asians with relatively high melanin content, postinflammatory hyperpigmentation, in particular, after fractional laser treatments [3–5].
Bearing such features in mind, the authors felt that it is necessary to reevaluate the safety and efficacy of ablative full-face resurfacing on atrophic acne scars in Asians. Ablative full-face laser skin resurfacing has been the gold standard for atrophic acne scars for nearly two decades. Nevertheless, it has an undesirable adverse event profile compared to fractional laser treatments. In order to make the ablative full-face resurfacing more effective and safer, we combined both short-pulsed and dual-mode erbium:yttrium–aluminum garnet (Er:YAG) lasers to treat moderate to severe acne scars in Asian patients. Our objectives were to determine the safety and efficacy of this new therapeutic modality.
Materials and methods
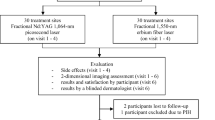
A retrospective review was conducted on consecutive ablative Er:YAG laser (Contour TRL, Sciton Inc, Palo Alto, CA) treatments which were performed between December 2009 and December 2012 on patients with acne scar. Informed consent was obtained from all patients, and the study was approved by the hospital’s medical ethics committee. The study protocol conformed to the guidelines of the 1975 Declaration of Helsinki. A total of 22 Korean patients (17 females and 5 males) with skin type III–V were included in this study. Only moderate to severe atrophic facial acne scars (ice pick, rolling, and box scar) were included in this review. The mean age of the patients was 30 years old (range 25–44) (Table 1). Information regarding herpes simplex virus (HSV) history was elicited from each of the patients before the laser treatments. Prophylactic antiviral therapy was given to the patients prior to the laser treatment.
After thoroughly cleansing their faces, a thick layer of topical EMLA cream (AstraZeneca, Sweden) was applied for an hour before the procedure. Air cooling (MAcURAY, KTMAX Inc., Korea) was provided during the procedure to minimize discomfort. For those with severe acne scars or with extensive involvement were given an option of tumescent anesthesia or local nerve block. Following laser treatment, closed dressings with Vaseline gauze (first 2 to 3 days) and polyurethane foam (DuoDERM CGF, ConvaTec Inc., USA) (the following 5 to 7 days) were applied to soak up the exudates. When the exudates dried up, the patients were routinely recommended to apply Cicaplast (La Roche-Posay, France) and Comfeel Barrier Cream (Coloplast Inc., Denmark) to the face. Also to decrease postoperative edema, orally administered prednisolone (10 mg once a day for 5 days) and a vial of dexamethasone injection (5 mg on the very day of laser treatment) were prescribed.
The Contour TRL Er:YAG laser used includes both short-pulsed (MicroLaserPeel, up to 50 μm of ablation) and dual-mode (up to 200 μm of ablation per pass, with or without variable depth coagulation) Er:YAG lasers built into the same device. For patients treated in our practice, we combined the short-pulsed Er:YAG laser resurfacing and dual-mode Er:YAG laser resurfacing. We first focused our treatments on the small areas with depressed acne scars. The dual-mode Er:YAG laser was used under the settings of 70 μm of ablation (17.5 J/cm2) with 50 % spot overlap (spot size of 4 mm) and 70 μm of coagulation. The scanner was modified within a range of 8 × 8–30 × 30 mm, according to the individual scar size. Each area received approximately three to five passes. After this procedure, a final pass of 25 μm of ablation mode at 6.25 J/cm2 was used on atrophic scars to remove the necrotic tissue. This step is believed to allow faster re-epithelialization, produce less crusting, and shorten the duration of erythema. The final procedure was short-pulsed Er:YAG laser resurfacing (settings at level 1 with 10 μm of ablation, 30 × 30 mm scanner), with one pass over the whole face. All patients received a single session of the new modality of Er:YAG laser resurfacing.
The results of the laser treatment was evaluated for the degree of clinical improvement, duration of erythema, pigmentary change, and any adverse events at 2 weeks, 1, 3, and 6 months following laser treatment. Clinical documentation was obtained by sequential photographs using identical camera settings, lighting, and patient positioning. The improvement in acne scars and overall skin texture were assessed by photo evaluation according to the following scales: poor (1) = <25 %, fair (2) = 25–50 %, good (3) = 51–75 %, and excellent (4) = >75 %. Two independent medical evaluators were involved in the photo evaluation process. Statistical analysis was performed using Minitab Statistical Package, version 15.1.20.0 (Minitab, Inc, State College, PA). For statistical testing, two-sided one-sample Wilcoxon signed rank test was used, and P values <0.05 were considered statistically significant.
In addition, a patient satisfaction score (1, not satisfied; 2, somewhat satisfied; 3, highly satisfied) was recorded after completion of treatment.
Results
The results of the blinded photo assessments indicated clinically and statistically significant mean improvement of 3.41 in scarring (P < 0.001). The majority of patients (19/22; 86 %) had an improvement of >50 % after a single session of laser treatment where 12 patients (55 %) achieved a significant improvement of >75 % (Table 2, Figs. 1 and 2).
The average time to re-epithelialization was 6 to 9 days. Posttreatment erythema (average duration of 1 month) was present in all patients. In two patients, it lasted longer than 3 months (9.1 %). Postinflammatory hyperpigmentation occurred in ten patients (45.5 %) mostly 2 to 4 weeks after treatment and lasted longer than 3 months in one patient (4.5 %). One patient experienced mild hypopigmentation (4.5 %). Mild to moderate acne flare-up occurred in five patients (22.7 %). No other adverse effects, such as scarring, bacterial infection, HSV outbreaks, or contact dermatitis was observed (Table 3). The acne-free areas ablated superficially by the short-pulsed Er:YAG laser normalized within a week and were free from prolonged erythema and postinflammatory hyperpigmentation.
The patient satisfaction assessment showed “somewhat satisfied” for six patients (27.3 %) and “highly satisfied” for 16 patients (72.7 %).
Discussion
Ablative full-face laser skin resurfacing with CO2 and Er:YAG lasers was the gold standard for atrophic acne scars for nearly two decades [6–9]. However, with the development of fractional laser devices, full-face laser skin resurfacing had been pushed out of the limelight. Now, after years of practice, it is becoming clear that fractional laser resurfacing cannot reach the efficacy of conventional ablative laser resurfacing even after repeated sessions of treatment [2, 3]. Accordingly, dermatologists are taking renewed interest in ablative non-fractional lasers for atrophic facial acne scars [2, 10–12]. Although effective, ablative full-face resurfacing has an undesirable adverse event profile compared to fractional laser treatments. In order to make the ablative full-face resurfacing more effective and safer, we attempted a new modality of Er:YAG laser resurfacing combining both short-pulsed and dual-mode Er:YAG lasers.
Ablative laser resurfacing removes skin tissue, layer by layer, thereby reducing skin irregularities. The heating of the tissue also causes collagen shrinkage and promotes neo-collagenesis. The Er:YAG laser, with a 2,940-nm wavelength, is highly absorbed by water, so it is almost totally absorbed by a very thin, superficial layer of skin and can be used for precise and superficial tissue ablation. The main advantages of the Er:YAG laser are the precise depth control, rapid healing, less postoperative morbidity, and fewer complications compared to the CO2 laser. However, because of limited residual thermal damage, intraoperative hemostasis is difficult to achieve. Moreover, because the thermal effects of short-pulsed Er:YAG irradiation are substantially less than those of CO2, the rates of intraoperative and postoperative collagen contraction are attenuated as well. In order to address the shortcomings of conventional Er:YAG laser resurfacing, a variety of newer laser systems has attempted to combine the precise ablation of a short-pulsed Er:YAG laser with some of the controlled thermal effects seen with the CO2 laser. One of these systems is the dual-mode Er:YAG laser which has two Er:YAG laser heads that provide both short-pulsed ablative and long-pulsed sub-ablative coagulative components [13]. Contour TRL, which we have used, allows the user to adjust the depth of ablation and coagulation independently. By modulating the laser’s energy to deliver supra-ablative pulses, the laser is able to vaporize up to 200 μm per pass with precision. For coagulation, sub-ablative laser energy is delivered in a train of pulses that heat the tissue to a selectable depth without vaporizing it. The pulses can be delivered as purely ablative (short pulse) or ablative and coagulative (dual mode), with the ablative component being immediately followed by a coagulative component [13].
In our new modality, Er:YAG laser resurfacing with short-pulsed and dual-mode Er:YAG lasers, the dual-mode application was strictly limited to the scars. The scar-free areas of the face were ablated superficially with the short-pulsed Er:YAG laser with minimal patient discomfort.
Patients treated with the new modality of Er:YAG resurfacing showed significant improvements on their atrophic facial acne scars with a clinically and statistically significant mean improvement of 3.41 (between good (50–75 %) and excellent (>75 %) improvement) in scarring after just a single session of laser treatment (P < 0.001). The findings were comparable to those in previous studies with the dual-mode Er:YAG laser [14–16] and significantly higher than that reported with fractional resurfacing (both ablative and non-ablative) alone or in combination with other lasers [3, 17, 18].
Complications, such as postinflammatory hyperpigmentation, prolonged erythema, hypopigmentation, and acne flare-up, were all present following the new modality of Er:YAG resurfacing. The incidence of the complications was comparable to that of former resurfacing studies with prolonged erythema (lasting for more than 3 months) in two patients (9.1 %) and postinflammatory hyperpigmentation in ten patients (45.5 %) [14–16, 19]. However, we believe the patient discomfort to be much lower with our new modality of Er:YAG resurfacing as the dual-mode Er:YAG laser is applied only focally to the atrophic scars. Accordingly, 72.7 % of our patients replied that they were highly satisfied with the overall treatment at their final follow-up at 6 months.
Concomitant or early intervention minimizes the risk of prolonged erythema and postinflammatory hyperpigmentation related to ablative full-face resurfacing. Prophylactic hydroquinone and rigorous sun protection are extremely helpful and should be recommended routinely. However, caution should be made when prescribing topical tretinoin, as it has a potential to aggravate facial erythema. In cases where the risk of complication is high (e.g., severe grade of scarring or extensive involvement, etc.) various preventive measures such as lasers (vascular lasers or low-fluence Q-switched Nd: YAG laser), skin care, and oral medication can be added to lower patient discomfort.
Although dark skin tone is considered a risk factor for hyperpigmentation following ablative laser therapy, our study results have shown that it is not of great concern, with most fading within 3 months. Sriprachya-anunt et al. [20] have shown slightly contradictory results from ours where postinflammatory hyperpigmentation occurred in 68 % of patients lasting for an average of 3.8 months after ablative full-face resurfacing. We believe the variance stems from the difference in latitude between San Diego, CA (where the study of Sriprachya-anunt et al. was performed) and Korea as well as the difference in living habits between the population (Hispanics vs Korean)—vigorous sun protection is performed at all times in Korea. There is also high possibility that our patients applied various “whitening” agents during the 6-month period either knowingly or unknowingly, since it is easily accessible and is included in a wide range of cosmetic products—this may have allowed the postinflammatory pigmentation to fade more quickly.
The authors conclude that the new modality of Er:YAG resurfacing with dual-mode Er:YAG laser and short-pulsed Er:YAG laser is an optimal combination with great efficacy and safety in patients with darker skin tones. The results revealed significant improvement and good patient acceptance. Continued research and advances in ablative technology should further enhance the ability to achieve minimal-risk scar effacement.
References
Manstein D, Herron GS, Sink RK, Tanner H, Anderson RR (2004) Fractional photothermolysis: a new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg Med 34:426–438
Huang L (2013) A new modality for fractional CO2 laser resurfacing for acne scars in Asians. Lasers Med Sci 28:627–632
Yeung CK, Chan NP, Shek SY, Chan HH (2012) Evaluation of combined fractional radiofrequency and fractional laser treatment for acne scars in Asians. Lasers Surg Med 44:622–630
Chan NP, Ho SG, Yeung CK, Shek SY, Chan HH (2010) The use of non-ablative fractional resurfacing in Asian acne scar patients. Lasers Surg Med 42:710–715
Chan HH, Manstein D, Yu C, Shek S, Kono T, Wei WI (2007) The prevalence and risk factors of post-inflammatory hyperpigmentation after fractional resurfacing in Asians. Lasers Surg Med 39:381–385
Alster TS, West TB (1996) Resurfacing of atrophic facial acne scars with a high energy pulsed carbon dioxide laser. Dermatol Surg 22:151–155
Alster TS (2000) Cutaneous resurfacing with Er:YAG lasers. Dermatol Surg 26:73–75
Ratner D, Tse Y, Marchell N, Goldman MP, Fitzpatrick RE (1999) Cutaneous laser resurfacing. J Am Acad Dermatol 41:365–389
Alster TS, Hirsch R (2003) Single-pass CO2 laser skin resurfacing of light and dark skin: extended experience with 52 patients. J Cosmet Laser Ther 5:39–42
Kutlubay Z, Gokdemir G (2010) Treatment of atrophic facial acne scars with the Er:YAG laser: a Turkish experience. J Cosmet Laser Ther 12:65–72
Sobanko JF, Alster TS (2012) Management of acne scarring. Part 1: a comparative review of laser surgical approaches. Am J Clin Dermatol 13:319–330
Goodman GJ (2011) Treatment of acne scarring. Int J Dermatol 10:1179–1194
Zachary CB (2000) Modulating the Er:YAG laser. Lasers Surg Med 26:223–226
Jeong JT, Park JH, Kye YC (2003) Resurfacing of pitted facial acne scars using Er:YAG laser with ablation and coagulation mode. Aesthetic Plast Surg 27:130–134
Tanzi EL, Alster TS (2012) Treatment of atrophic facial acne scars with a dual-mode Er:YAG laser. Dermatol Surg 28:551–555
Woo SH, Park JH, Kye YC (2004) Resurfacing of different types of facial acne scar with short-pulsed, variable-pulsed, and dual-mode Er:YAG laser. Dermatol Surg 30:488–493
Sardana K, Garg VK, Arora P, Khurana N (2012) Histological validity and clinical evidence for use of fractional lasers for acne scars. J Cutan Aesthet Surg 5:75–90
Ong MW, Bashir SJ (2012) Fractional laser resurfacing for acne scars: a review. Br J Dermatol 166:1160–1169
Tanzi EL, Alster TS (2003) Single-pass carbon dioxide versus multiple-pass Er:YAG laser skin resurfacing: a comparison of postoperative wound healing and side-effect rates. Dermatol Surg 29:80–84
Sriprachya-anunt S, Marchell NL, Fitzpatrick RE, Goldman MP, Rostan EF (2002) Facial resurfacing in patients with Fitzpatrick skin type IV. Lasers Surg Med 30:86–92
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, S.J., Kang, J.M., Chung, W.S. et al. Ablative non-fractional lasers for atrophic facial acne scars: a new modality of erbium:YAG laser resurfacing in Asians. Lasers Med Sci 29, 615–619 (2014). https://doi.org/10.1007/s10103-013-1372-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-013-1372-8