Abstract
Intravenous laser blood irradiation (ILBI) is widely applied in the treatment of different pathologies including diabetes mellitus. The aim of this study is to evaluate the effects of ILBI on the metabolites of blood in diabetic type 2 patients using metabolomics. We compared blood samples of nine diabetic type 2 patients, using metabolomics, before and after ILBI with blue light laser. The results showed significant decrease in glucose, glucose 6 phosphate, dehydroascorbic acid, R-3-hydroxybutyric acid, l-histidine, and l-alanine and significant increase in l-arginine level in blood and blood sugar in the patients have reduced significantly (p < 0.05). This study clearly demonstrated a significant positive effect of ILBI on metabolites of blood in diabetic type 2 patients. These findings support the therapeutic potential of ILBI in diabetic patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intravenous or intravascular laser blood irradiation (ILBI) with red, UV, and blue light is widely applied in the treatment of different pathologies. Blood irradiation therapy can be administered through a catheter in a vein, usually a vein in the forearm [1]. The medical effects are determined by predominance of systemic healing mechanisms including biostimulative, analgesic, anti-allergic, immunocorrective, antitoxic, vasodilative, antiarrhythmic, antibacterial, antihypoxic, spasmolytic, anti-inflammatory, and other properties [2]. It enlarges the arterio-venous difference of oxygen that testifies the liquidation of a tissue hypoxia and enrichment of oxygenation which is a sign of tissue metabolism normalization and improves oxidation of energy-carrying molecules like glucose, pyruvate, and other substances. In addition, the laser irradiation activates ATP synthesis and energy formation in cells [1]. Intravenous laser therapy reduces glucose, cholesterol, low-intensity, and very low density lipoproteins (VLDL) and stabilizes hormonal and immune system status [3]. It seems that blue light irradiation can increase production of arginine and nitric oxide. Arginine causes the release of various hormones such as insulin, glucagon, growth hormone, prolactin, and adrenal catecholamines [4].
As ILBI influences the whole organism it can be a proper therapeutic modality in complex diseases like diabetes mellitus. Diabetes is a pathological and metabolic state caused by inadequate transport and breakdown of glucose. It demonstrates a low serum ratio of insulin to glucagon and high levels of fatty acids. The liver produces glucose while other tissues use ketones and fatty acids instead of glucose. Gluconeogenesis increases in the livers and secretes large amounts of VLDLs and fatty acid accumulation in droplet form. These fatty acids are oxidized by the liver which produces acetone, acetoacetate, and beta- hydroxybutyrate. Muscle glycogen almost disappears and its protein is broken down to support gluconeogenesis [3].
Understanding this complex molecular pathway and the effect of ILBI on it may be helped by the recent advent of technologies for comprehensive metabolic analysis termed metabolomics which studies the global metabolic changes in biological systems [5]. This technique uses comprehensive analytical methods to study metabolites, metabolism, and other small molecules in cells and tissues at the same time. This technique uses multiple high-throughput technologies including nuclear magnetic resonance (NMR), mass spectrometry (MS), and molecular nano-sensors (MNS), along with chemometric data analysis for generating and interpreting profiles of metabolism in complex biological systems. It can provide biomarkers for disease sub types and hence can help in diabetes research [6]. Metabolomics can provide some advantages in diabetes research specially that it can estimate vary but one current source which is Human Metabolome Database (HMDB) [7]. In this method, metabolites are extracted from different biological matrices like tissues, blood, and urine. There are two major instrument platforms for measuring the level of metabolites in these samples, NMR and MS [5].
Many diseases including diabetes have been monitored and even checked with NMR [6]. We previously used this method for screening of thalasssemia patients and quantification some hematological parameters [8] and detection of metabolic changes during immunization [9].
In this study, for the first time we used NMR to evaluate the effects of ILBI on blood metabolites in diabetic type 2 patients.
Materials and methods
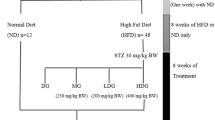
After approval of the ethics committee of research projects, nine diabetic type 2 patients (five males: mean age, 61.14 years; four females: mean age, 60 years) referred to the laser clinic of Milad Hospital who agreed to participate in our study were selected. After completing the consent forms, blood sugar was measured using ExiChek Blood Glucose Monitoring System (Exir Company, Iran). Non-fasting venous blood samples were collected in standard 5-ml sodium heparin tubes for metabolomics study before and after the laser therapy. According to our previous study [10], ILBI was applied intravenously (the laser fiber was entered the vein using a catheter) with 1.5 mW, continuous, 405-nm laser therapy apparatus (Azor, Russia) through the venue catheter for 30 min in the large veins of the upper limb. This protocol was designed according to our previous experiments [10]. Blood sugar was checked again and another venous blood samples were collected in standard 5-ml sodium heparin tubes after 30 min after ILBI. Immediately after collection, the samples were stored on ice and centrifuged (4 °C, 10 min at 2,000×g) within 30 min. The plasma samples were stored at −20 °C until analysis and thawed prior to use.
Sample preparation for proton NMR (1HNMR) spectroscopy
Seven hundred microliters of plasma was mixed with 70 μl (10 %) deuterium oxide (D2O) in a 5-mm NMR tube.
NMR data collection
One-dimensional 1HNMR spectra were acquired on a Bruker DRX-500 NMR spectrometer (Bruker, England) operating at 500.13 MHz at 298 k. For each plasma sample, the free induction decay (FID) was weighted by an exponential function with a 0.3-Hz line broadening factor prior to Fourier transformation (FT). Water pre-saturation pulse sequence (D-90-t1-90-tm-90-acquired FID) with relaxation delays 5 s and flip angle 90°, water signals and the broad protein resonances were suppressed by a combination of pre-saturation and the Carr-Purcell-Meiboom-Gill (CPMG)(90-(t-180-tn-acquisition)) (τ = 200, n = 100) pulse sequence [11].
Data reduction
CPMG-NMR spectra were segmented into region of 0.01 ppm width using Mestrec C version 4.7 software. In practice, pseudo-variables were generated by integrating the spectral data into discrete regions about the width of spectral peaks associated with metabolites. The integrated area under the curve for each region (referred to as “bins” or “buckets”) was calculated, and these values served as variables. The region of the spectrum which included the water signal (δ 4.6–4.8) was removed from analysis in both groups to eliminate variation in water suppression efficiency. The area for each segmented region was calculated and the integral values resulted in an intensity distribution and description of the whole spectrum with 1,000 variables prior to chemometric analysis which was normalized by setting it to the total region of each spectrum.
Chemometrics analysis
Partial least square
Partial least square (PLS) was applied after orthogonal signal correction (OSC) filters with spectral data as X matrix and the samples data sets labeled as 0 for normal and 1 for abnormal for Y matrix [12]. PLS was performed with and without OSC and results were obtained with more than 95 % confidence levels.
OSC
OSC filters were developed to remove unwanted variation from spectral data [13]. Matrix X comprises of 1HNMR data of samples before laser and matrix Y as 1HNMR data after laser therapy. OSC subtracts from X, factors that account for as much as possible of the variance in X and are orthogonal to Y. It is important to avoid over fitting after OSC treatment, to prevent poor predictive performance; hence, precise determination of the number of removed OSC factors is very important and here only one factor was removed.
The NMR search link of the HMDB was used to detect the metabolites at the certain chemical shift. It is a freely available electronic database containing detailed information about metabolites found in the human body [14].
Metabolic pathway analysis
It was carried out with MetaboAnalyst 2.0 for pathway analysis and their visualization. These pathways were those in which the differentiating metabolites were analyzed and seen to be participating in [15].
Data analysis
Blood sugar in the patients was compared, using student’s t test and p < 0.05 was considered significant.
Results
PLS following OSC gave very good results and the two groups separated very well. Figure 1 shows score plot and Fig. 2 shows biplot of OSC-PLS of samples before and after laser therapy
Biplot of PLS after OSC showing the differentating metabolites. Odd numbers are samples before laser treatment and even numbers show samples after laser treatment. Using the numbers of differentiating metabolites, the chemical shifts were detected and by using the HMDB testing the metabolites were recognized as indicated in Table 1
Using the numbers of differentiating metabolites, the chemical shifts were detected and by using the HMDB testing the metabolites were recognized as indicated in Table 1. The main metabolites which have changed as can be seen in Table 1 are glucose, glucose-6-phosphate, dehydroascorbic acid, R-3-hydroxybutyric acid, l-histidine, and l-alanine which show a decrease whereas l-arginine shows an increase in plasma levels.
The list of metabolites was entered into the pathway analysis and the impact of pathways is shown in Fig. 3, the size and position of the pathway showing its impact. Larger circles, higher and closer to the Y-axis show their higher impact.
The pathway analysis in Table 2 shows the main pathways in which a change has taken place in descending order. Number of hits indicates the number of metabolites which have changed in the cycle.
The same database using the uploaded data indicates the metabolite responsible for alteration in the different pathways. The three metabolites identified for changes in most of the cycles by the pathway analysis software were d-glucose, beta d-glucose, and glucose-6-phosphate. The cycles which have changed before and after laser treatment due to amino acids of l-histidine, l-alanine, and l-arginine are aminoacyl-tRNA biosynthesis due to involvement of d-arginine and d-ornithine metabolism and amino sugar metabolism. The aminoacyl-tRNA biosynthesis which is active during protein synthesis delivers amino acids to ribosomes.
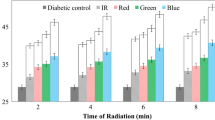
The cycles involved in glycolysis, pentose phosphate pathway, starch, and sucrose metabolism, galactose metabolism and synthesis, and degradation of ketone bodies which are involved in the diabetes cycle have also altered. d-hydroxybutyrate is seen to cause a change in synthesis and degradation of ketone bodies. This is evident as blood sugar in the patients have reduced significantly, p < 0.0018 by student’s t test (mean before LLLT = 190 ± 17 and mean after LLLT = 165 ± 20) as shown in Fig. 4.
l-Arginine and l-proline metabolism which are involved in the urea cycle also show a change.
Discussion
Our study seems to indicate that intravenous laser treatment seemed to be effective in diabetic patients. Of the main cycles effected by ILBI was the pentose phosphate pathway, the glycolysis, or the gluconeogenesis pathway, starch, and sucrose metabolism; which were affected by the three main metabolites involved: d-glucose, beta d-glucose, and glucose-6-phosphate, all of which are involved in glycolysis. d-Hydroxybutyrate is involved in synthesis and degradation of ketone bodies which has been reported in diabetes [14]. Similarly, galactose metabolism has been seen to be affected by our treatment and it has been reported to be involved with insulin secretion [16] and effecting retinopathies [17].
Though dehydroascorbic acid was not detected by the Metaboanalyst software, its level has changed in our therapy. However, dehydroascorbic acid has been reported to be high in diabetic individuals and our therapy has shown a reduction in its level [18]. The tRNA aminoacyl cycles have been modified by the laser therapy as well as biosynthesis of l-histidine and metabolism of l-alanine and l-arginine.
The effect of ILBI on three amino acids, histidine, alanine, and arginine is indicated in our research. This has resulted in a change in aminoacyl-t-transferase activity in the blood. Histidine is endogenously synthesized in brain, skeletal muscles, and liver [19] and is an important amino acid involved in diabetes. A report on association of glycemia and genetic risk for hyperglycemia in type 2 diabetes with amino acid levels was carried out in Finland in the population-based Metabolic Syndrome in Men (METSIM) study. The levels of branched-chain, aromatic amino acids and alanine increased and the levels of glutamine and histidine decreased with increasing glycemia, reflecting at least in part, insulin resistance [20]. Our laser therapy has shown altered levels of histidine, alanine, and arginine along with low sugar levels. This has resulted in altered aminoacyl-tRNA biosynthesis.
Another study has shown the association between elevated serum alanine aminotransferase activity and diabetes in Mexican men [21]. Alanine aminotransferase, an enzyme like other aminotransferases of transaminases, is important in the production of various amino acids, measuring the concentrations of various transaminases in the blood, diagnosing, and tracking many diseases. A study has reported elevated alanine aminotransferase in both type 1 and type 2 diabetes patients [22].
Carnosine is a dipeptide made of histidine and alanine and when taken along with histidine orally has been shown by Japanese researchers to delay diabetic deterioration in mice and protect human low-density lipoprotein against oxidation and glycation [23]. A study of the effects of carnosine on insulin and glucagon secretion was carried out in the dog by IV and oral consumption of carnosine and histidine and beta alanine. The results suggest that the increased pancreatic hormonal secretion observed was not due to carnosine “per se” but was mediated instead by its histidine content. A protein named histidine phosphatase regulates glucose and mitochondrial fuel-induced insulin secretion in pancreatic β cells [22].
Arginine, another amino acid detected by our method, is a well-known antioxidant especially in diabetic patients with atherosclerotic peripheral arterial disease of lower extremities [24]. It has been shown to be involved in diabetes since the early 1970s when glucose was given with different amino acids. The effect of arginine with glucose on plasma insulin was greater than that of leucine or histidine with glucose. It was suggested that the synergism resulted from the stimuli acting directly on the pancreatic beta cells [14]. Its oral effect was tested long term on glucose metabolism and though it did not reduce the incidence of diabetes it significantly increased regression to normal glucose tolerance [25].
Arginine causes the release of various hormones such as insulin, glucagon, growth hormone, prolactin, and adrenal catecholamines. Recent studies have showed that blue and red light irradiation can increase production of arginine and nitric oxide [5].
ILBI which was pioneered in Russia refers to blood irradiation through an intravenous needle or transcutaneously venous radiation. The most common used wavelengths include 890, 630, 650, and recently 450 nm. According to the Russian studies ILBI increases oxygen content and reduces the partial pressure of carbon dioxide. It eliminates tissue hypoxia, stimulates oxygenation, normalizes tissue metabolism, and activates the non-specific mechanisms of anti-infectious immunity. It reduces content of C-reactive protein, raises activity of complement, increases the plasma level of immunoglobulins (IgA, IgM, IgG), decreases thrombocyte aggregation ability, and activates fibrinolysis which enhances peripheral circulation [26]. Earlier, Lebed’kov et al. studied the effect of ILBI on the blood lipid and phospholipid components in patients with diabetes mellitus. They showed that laser irradiation of blood significantly affects blood components in a complex treatment of diabetes mellitus [27]. Ramadawon used ILBI in combination with low-level laser therapy and acupuncture laser therapy to control blood sugar in diabetic patients [28]. Arginine causes the release of various hormones such as insulin, glucagon, growth hormone, prolactin, and adrenal catecholamines. Recent studies have showed that blue and red light irradiation can increase production of arginine and nitric oxide [4]. Mittermayr et al. showed that blue laser light can facilitate the release of nitric oxide and affect tissue perfusion [29]. In our previous studies, we showed the effect of low-level laser therapy on neuropathy and wound healing in diabetic type 2 patients [10, 30]
We used metabolomics to evaluate the effect of intravenous laser treatment in diabetic patients for the first time, which seemed to be effective, as the metabolites and the cycles which were detected with NMR were effective in diabetes; even though we have to highlight the few number of cases. Furthermore on this topic, there is a great lack of data from literature and further studies are needed. However, further studies with larger sample size are needed to corroborate this theory.
References
Gasparyan L (2003) Laser Irradiation of the blood. Laser Partner-Clinixperience 1–4
Moshkovska T, Mayberry J (2005) It is time to test low level laser therapy in Great Britain. Postgrad Med J 81:436–441
Makela AM (2004) Theoretical backgrounds for light application in diabetes. Laser, Florence
Makela AM (2005) Role of l-arginine in the biological effects of blue light. Laser, Florence
Fiehn O (2002) Metabolomics—the link between genotypes and phenotypes. Plant Mol Biol 48:155–171
Wei H, Pasman W, Rubingh C et al (2012) Urine metabolomics combined with the personalized diagnosis guided by chinese medicine reveals subtypes of pre-diabetes. Mol Mol Biosyst 8:1482–1491
Bain JR, Stevens RD, Wenner BR et al (2009) Metabolomics applied to diabetes research. Diabetes 58:2429–2443
Arjmand M, Kompany-Zareh M, Vasighi M et al (2010) Nuclear magnetic resonance-based screening of thalassemia and quantification of some hematological parameters using chemometric methods. Talanta 81:1229–1236
Zamani Z, Arjmand M, Tafazzoli M, Gholizadeh A, Pourfallah F et al (2011) Early detection of immunization: a study based on an animal model using 1H nuclear magnetic resonance spectroscopy. Pak J Biol Sci 14:195
Kazemi-Khoo N (2006) Successful treatment of diabetic foot ulcers with low-level laser therapy. Foot 16:184–187
Stepišnik J, Lasič S, Mohorič A et al (2006) Spectral characterization of diffusion in porous media by the modulated gradient spin echo with CPMG sequence. J Magn Reson 182:195–199
Wold S, Sjöström M, Eriksson L (2001) PLS-regression: a basic tool of chemometrics. Chemometrics Intellig Lab Syst 58:109–130
Fearn T (2000) On orthogonal signal correction. Chemometrics Intellig Lab Syst 50:47–52
Floyd J Jr, Fajans S, Pek S et al (1970) Synergistic effect of essential amino acids and glucose upon insulin secretion in man. Diabetes 19:109–115
Xia J, Psychogios N, Young N, Wishart DS (2009) Metabo analyst: a web server for metabolomic data analysis and interpretation. Nucleic Acids Res 37:W652–W660
Ercan N, Nuttall F, Gannon M, Redmon J, Sheridan K (1993) Effects of glucose, galactose, and lactose ingestion on the plasma glucose and insulin response in persons with non-insulin-dependent diabetes mellitus. Metabolism 42:1560–1567
Kowluru RA, Tang J, Kern TS (2001) Abnormalities of retinal metabolism in diabetes and experimental galactosemia. VII. Effect of long-term administration of antioxidants on the development of retinopathy. Diabetes 50:1938
Banerjee A (1982) Blood dehydroascorbic acid and diabetes mellitus in human beings. Ann Clin Biochem 19:65
Boldyrev AA, Severin SE (1990) The histidine-containing dipeptides, carnosine and anserine: distribution, properties and biological significance. Adv Enzyme Regul 30:175–188
Stančáková A, Civelek M, Saleem NK et al (2012) Hyperglycemia and a common variant of GCKR are associated with the levels of eight amino acids in 9,369 Finnish men. Diabetes 61(7):1895–1902
Meltzer AA, Everhart JE (1997) Association between diabetes and elevated serum alanine aminotransferase activity among Mexican Americans. Am J Epidemiol 146:565–571
Kamath V, Kyathanahalli CN, Jayaram B, Syed I, Olson LK et al (2010) Regulation of glucose-and mitochondrial fuel-induced insulin secretion by a cytosolic protein histidine phosphatase in pancreatic β-cells. Am J Physiol Endocrinol Metab 299:E276–E286
Lee Y, Hsu C, Lin M, Liu K, Yin M (2005) Histidine and carnosine delay diabetic deterioration in mice and protect human low density lipoprotein against oxidation and glycation. Eur J Pharmacol 513:145–150
Jabłecka A, Bogdański P, Balcer N et al (2012) The effect of oral l-arginine supplementation on fasting glucose, HbA1c, nitric oxide and total antioxidant status in diabetic patients with atherosclerotic peripheral arterial disease of lower extremities. Eur Rev Med Pharmacol Sci 16:342
Ld M, Setola E, Lucotti PCG et al (2012) Effect of a long term oral l-arginine supplementation on glucose metabolism: a randomised, double blind, placebo controlled trial. Diabetes Obes Metab 14:893–900
Brill G, Gasparyan L, Makela A (2008) 122 Modification in relationships in the system endothelial cell blood platelet by low level laser irradiation. Photodiagn Photodyn Ther 5:S40–S41
Lebed’kov E, Tolstykh P, Marchenko L et al (1998) The effect of the laser irradiation of the blood on its lipid and phospholipid components in diabetes mellitus. Voenno-medit͡sinskiĭ zhurnal 319:37
Ramdawon P (1999) Bioresonance information laser therapy of diabetes mellituse a first clinical experience of the hypoglycemic effect of low level laser terapy and its perspectives. Paper presented at North American Laser Therapy Association Conference; 1999 Oct; Rockville, Washington D.C., USA.
Mittermayr R, Osipov A, Piskernik C et al (2007) Blue laser light increases perfusion of a skin flap via release of nitric oxide from hemoglobin. Mol Med 13:22
Khamseh ME, Kazemikho N, Aghili R et al (2011) Diabetic distal symmetric polyneuropathy: effect of low-intensity laser therapy. Laser Med Sci 26(6):831–835
Acknowledgment
We wish to acknowledge the Bahsaz Laser Instruments Co. Ltd, laboratory staff of Milad Hospital, the Organic Chemistry unit of Sharif University of Technology, Dr. Ehsan Mostsfavi, Dr. Saber Esmaili, and Morteza Mehrjoo for their supports and comments.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kazemi Khoo, N., Iravani, A., Arjmand, M. et al. A metabolomic study on the effect of intravascular laser blood irradiation on type 2 diabetic patients. Lasers Med Sci 28, 1527–1532 (2013). https://doi.org/10.1007/s10103-012-1247-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-012-1247-4