Abstract
In this study a minimally invasive microsurgical approach was used for laser patterned microcoagulation (LPM) to initiate gingival and oral mucosal tissue regeneration. We performed a feasibility assessment and histological examination of laser damage and regeneration in the gingiva and oral mucosa using an animal model. The study animals comprised 18 healthy rabbits which were treated in vivo with single pulses from a diode laser at a wavelength of 980 nm and a power of up to 20 W applied to the gingival and oral mucosa at multiple time points. Biopsies were stained with hematoxylin and eosin, nitroblue tetrazolium chloride and picrosirius red, and evaluated by two pathologists blinded to the parameters and date of laser exposure. Histological analysis revealed that the continuity of the epithelial basal cell layer had been reestablished by 1–2 days after LPM, and complete epithelial regeneration had occurred by 7–12 days. A pronounced reactive inflammation developed in the column area 1 day after treatment. High activity of fibroblasts producing new collagen participated in the formation of a network of new thin-wall blood vessel. By the 28th day the tissue structure was almost completely restored with a similar increase of vascularity, and there were no signs of scarring. By the 90th day, tissue structure was completely restored, indicating complete healing. A single LPM treatment induces a wound healing response in the oral mucosa, showing the potential of LPM for the initiation of oral mucosa and gingival regeneration. Complete healing observed in 3 months after treatment with no keratinization change or scar tissue formation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Periodontal soft-tissue regeneration is one of the most important objectives in periodontal therapy. In periodontal plastic surgical procedures, coverage of the exposed root with soft tissues and improvements in surgical techniques have been shown to reduce recession height after periodontal surgery. In this study a minimally invasive microsurgical approach using laser patterned microcoagulation (LPM) was used to initiate gingival and oral mucosal tissue regeneration. The ultimate goal of the research was to create a new minimally invasive and cost-effective treatment device and procedure for initiating gingival regeneration and regrowth. In this study we performed a feasibility assessment and histological evaluation of laser-assisted formation and regeneration of the gingiva and oral mucosa using an animal model.
The LPM treatment concept is similar to that of fractional photothermolysis [1] and lattice of optical islets [2], which have been successfully applied in dermatology [1, 3–5] and ophthalmology [6]. The creation of microscopic thermal wounds representing islets of tissue damage surrounded by spared normal tissue has been shown to greatly enhance the regenerative capacity of the tissue, resulting in completely scar-free tissue self-repair. The scar-free repair occurs even when the thermally damaged volume is as much as 25% of the original superficial tissue volume [7]. Fractional photothermolysis has been used commercially since 2004 for the treatment of facial wrinkles, acne scars, surgical scars, melasma and photoirradiated skin. It has become very popular because of the low levels of tissue damage and associated side effects due to the combined high efficacy and minimal invasiveness of the procedure. Millions of patients with skin conditions and tens of thousands of patients with ophthalmic conditions have been treated during the last years with minimal complications and side effects [5]. However, to the best of our knowledge, this type of laser treatment has never been applied to oral soft tissues.
Oral tissues are known to have even greater regenerative potential than skin [8] because of higher vascularization and metabolism. Thus, we hypothesized that the gingiva will show fast, scar-free regeneration and a potential volume increase in response to treatment involving the creation of a pattern of thermal microwounds analogous to those leading to the rapid recovery of skin. Possible applications of LPM treatment of soft oral tissues include the management gingivitis and gingival recession, stimulation of the growth and regrowth of interdental and interimplant papillae, conversion of gingival biotype from thin to thick, stimulation of the regeneration of alveolar bone and periodontal ligament, and treatment of scars and localized hyperpigmentation. Potentially, it could also be used to augment the treatment of periodontal disease by stimulating gingival growth and improving periodontal attachment in patients with moderate and severe periodontitis. LPM treatment is characterized in terms of the topology and size of the microcoagulated islets and the geometry of the microcoagulated spot pattern including the distance between them. These parameters should be carefully optimized for safe and effective treatment. The aim of the present study was to demonstrate oral tissue response to the LPM treatment on the animal model.
Materials and methods
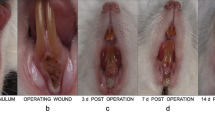
The animals included in the study comprised 18 healthy New Zealand rabbits (16 males 6–8 months old and two females 5 months old). One rabbit was treated after death, and 17 rabbits were treated in vivo and monitored over the period 1 to 90 days. Laser-induced microscopic coagulation zones (MCZ) were formed in rows (usually two or three MCZ in a row depending on the available gingival space on the rabbit’s maxilla apically from the incisors; Fig. 1). The animals were anesthetized with 3 mg/kg of the muscle relaxant Rometar (Interchemie, Castenray, The Netherlands) administered by intramuscular injection.
To obtain information about the immediate MCZ profile and healing response to the laser treatment in the gingiva and oral mucosa, multiple procedures were performed at different time points at several sites. After the last treatment animals were killed by injection of 100 mg/kg of Zoletil 50 (Vibrac Laboratories, Carros, France) and the treated areas of gingiva and oral mucosa excised and submitted for histology. A maximum of four treatments per animal were performed and specimens for histology were obtained at 1 h and 1, 5, 12, 30 and 90 days after laser treatment.
Laser system
The laser wavelength was selected based on computer simulation of light propagation and soft tissue coagulation using a previously described methodology [2]. The target size of the column-like MCZ was 0.2–0.5 mm in diameter and 1–2 mm in depth. This size of the MCZ can be obtained by laser radiation in the spectral range with weak (about 0.4 cm−1) or moderate (about 15 cm−1) absorption of water as the primary chromophore in the wavelength range 950–1,860 nm excluding the range 1,400–1,520 nm around the strong peak of water absorption. We selected 980 nm because it has a peak absorption in water at a relatively low value and because it can be generated with high power by compact, reliable and cost-effective diode lasers, so that the same laser could be used for surgery and for the LPM treatment if proven effective. A diode laser operating at a wavelength of 980 nm and generating up to 20 W of power was used in this study. Each column was created by contact application of a transparent tip with diameter of 400 μm and irradiating the tissue through the tip with a single rectangular pulse. The thermal relaxation time of a column with a diameter of 0.5 mm in soft tissue is about 160 ms [9]. For selective coagulation of a target MCZ, the pulse width has to be shorter than or comparable to the thermal relaxation time of the MCZ. In this study we used a rectangular pulse with a peak power of 20 W and pulse durations of 80, 120, 150 and 250 ms. The pulse energies were accordingly 1.6, 2.4, 3.0 and 5.0 J, resulting in fluences at the tip of 1.23, 1.91, 2.4 and 4 kJ/cm2, respectively. In addition, these parameter ranges were confirmed by numerical simulation using a previously described methodology [2] and experiments with column formation in ex-vivo soft tissue.
Histology
For each irradiation regime at least two MCZs with a column-like shape were formed. The area of the first column was removed from the specimen, fixed in 10% formaldehyde and embedded in paraffin. Serial sections of thickness 3 μm were then prepared and stained with hematoxylin and eosin (H&E) and picrosirius red (PSR) for histological analysis. The second column was processed separately for the preparation of frozen sections which were stained with nitroblue tetrazolium chloride (NBTC) for evaluation of viability. NBTC staining was performed as described by Hukki et al. [10]. PSR staining together with polarization microscopy was performed to detect collagen fibers [11].
Two pathologists experienced in oral soft-tissue pathology and laser treatment evaluated the sections independently. They qualitatively assessed cellular inflammatory infiltration, reepithelialization, and fibroblast activity. No quantitative assessments were performed.
Results
Immediately after LPM, for all exposure times (80–250 ms) epithelial and connective stroma proteins showed coagulation, with the stratum corneum layer being intact in the majority of cases (Figs. 2a and 3a). The zone of laser damage could be seen in histological specimens with all three types of staining (Figs. 2, 3, 4 and 5). The immediate effect of laser irradiation on tissue is best observed in NBTC-stained specimens [12, 13]. The NBTC stain revealed loss of viability in the epithelium and the submucosa after LPM and showed the broadest area of thermal damage in the column, associated with inhibition of oxidative enzymatic activity, with high contrast, which allowed measurement of the size of the laser column with high accuracy. Figure 2a shows a column 1.3 × 0.4 mm in size formed with an exposure time of 120 ms. The column width varied from 0.4 to 0.7 mm, and the depth from 1.1 to 1.8 mm with all exposure times. The column size appeared to increase with increasing laser pulse duration.
Healing of laser-induced MCZ columns (NBTC stain). a 1 h after irradiation with a pulse of 120 ms: the column borders in the epithelium and connective tissue are distinct, and tissues are devitalized. b 1 day after irradiation with a pulse of 80 ms: the column borders are smeared due to inflammatory cell infiltration. c 7 days after irradiation with a pulse of 150 ms: new epithelium has invaginated into the column area, and the column borders in the connective tissue are hardly distinguishable due to new collagen fiber formation (a 0.95 × 1.6 mm, b 0.95 × 0.98 mm, c 0.95 × 1.26 mm)
Healing of laser-induced MCZ columns after irradiation with a pulse of 150 ms (H&E stain). a 1 h after irradiation: the epithelium and connective tissue fibers show coagulation. b 5 days after irradiation: new epithelium has invaginated into the column area, and inflammatory infiltration, active fibroblasts and thin-walled vessels are seen. c 12 days after irradiation: new epithelium and unorganized collagen fibers are seen. d 28 days after irradiation: no signs of cellular infiltration are apparent, but minor edema is present. e 90 days after irradiation: no signs of inflammation are seen (0.95 × 0.98 mm)
Stages in healing of laser-induced MCZ columns after irradiation with a pulse of 150 ms. a Day 1, leukocytic infiltration (H&E stain). b Day 2, re-epithelialization: the epithelium has invaginated into the defect area (NBTC stain); c Connective tissue regeneration: active fibroblasts and thin-wall vessels are seen (H&E stain). d Day 12, reconstruction: new epithelium with signs of parakeratosis and new unorganized collagen fibers are seen (on the left old epithelium and horizontally oriented collagen fibers under the epithelium are present) (0.39 × 0.39 mm)
Healing of laser-induced MCZ columns after irradiation with a pulse of 150 ms (picrosirius red stain under polarized light). a Day 2: the area is well defined, little red color is present due to loss of collagen, the epithelium has peeled off, and subepithelial clefting is seen. b Day 4: the area with no red color has diminished appreciably. c Day 12: the area with no red color is hard to distinguish, indicating column healing and new collagen formation; the epithelial surface is white in color, typical of free keratin, which indicates increased keratinization. d Day 28: collagen formation is complete. d Day 90: the column is no longer visible (0.95 × 0.98 mm)
Wound healing occurs in successive and overlapping stages: inflammation, proliferation, and regeneration [8, 14, 15]. Healing of laser-induced wounds also follows this pattern [1, 4, 12]. In the following sections we discuss specific features of wound healing in the oral mucosa after laser irradiation.
Inflammatory stage of healing
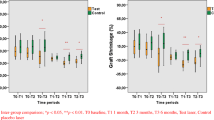
The inflammatory stage was observed beginning 1 day after treatment with all pulse durations (80–250 ms). An inflammatory cellular infiltration consisting of neutrophils, macrophages, and lymphocytes (Figs. 2b and 4a) with an intensity proportional to the laser pulse duration appeared. One day after laser treatment the amount of neutrophils was highest with the pulse duration of 250 ms. Maximum inflammatory activity was observed during days 2–4, after which the intensity of the cellular infiltration slowly decreased coming back to the baseline level by the day 12 of observation (Fig. 3c). By the day 28 cellular infiltration was absent, but minor edema could still be seen (Fig. 3d). By day 90 no inflammatory signs could be seen.
Proliferative stage of healing
The first signs of epithelial regeneration, such as basal cell activity, lateral propagation and invagination of epithelium into the column area were already present on days 1–2 after irradiation with pulses of short and moderate duration (80–150 ms). In NTBC-stained specimens the newly formed epithelium could be seen above devitalized connective tissue as early as 1 day after irradiation with a pulse of 80 ms (Fig. 2b) or on day 2 after treatment with a pulse of 150 ms (Fig. 4b). In one column created with a pulse of 150 ms, the old epithelium had peeled off by day 2 and there were no signs of re-epithelialization (Fig. 5a). On days 5–7 reactive epithelial hypertrophy was seen, indicating enhanced proliferation of the basal and prickle cell epithelial layers (Figs. 3b and 2c). By day 12 signs of para- and hyperkeratosis were observed in the formed epithelium after irradiation with longer duration pulses (250 and 150 ms; Fig. 4d). On days 7–12 after irradiation there were no signs of dyskeratosis or spongiosis in the new epithelium. The new epithelium was fully formed by days 21–28 (Fig. 3d).
Connective tissue regeneration started with enhanced fibroblast proliferation that was first observed on day 3 after irradiation with a pulse of 80 ms, on day 4 with 120 ms, and on day 5 with 150 and 250 ms (Fig. 4c). Thin young collagen fibers were arranged chaotically up to the day 12, and young connective tissue was filled with newly formed thin-walled blood vessels (Fig. 4d).
The collagen coagulation zone was filled with newly formed collagen. While exact determination of the collagen type would have required special immunohistochemical staining [16, 17], it is very likely, based on PSR staining and the thickness of the collagen fibers, that this was type I collagen. PSR-stained sections of type I collagen under polarized light look red, yellow or yellow–red [11, 18–21]. Dye molecules bind with type I collagen at the level of their tertiary structure making the majority of tissues look pink under transmitted white light. Under polarized light type I collagen manifests its birefringent features [20, 21]. Coagulated collagen loses its ability to depolarize light, and hence gives no color in polarization microscopy, appearing as a black zone instead. In the course of time after laser damage, the area of connective tissue fiber coagulation diminished in the column area but was still observed as late as day 12 following irradiation with short and moderate pulse durations (80–150 ms) (Figs. 5a–c). By day 28 formation of new collagen in the column area had finished, and by day 90 healing was complete and the column could not be visualized histologically (Figs. 5d, e).
The regeneration stage includes organization and ordering of fibers and connective tissue cells. When incisional wounds heal this stage begins on days 4–5 and lasts 1 to 12 months according to data from different authors [15, 22]. For LPM-type injury, by day 12 (Fig. 4d) and even by day 28 (Fig. 3d) after irradiation with a pulse of 150 ms, the collagen fibers under the epithelium still do not have a regular orientation as was present before irradiation. However, by day 90 all connective tissue collagen had formed, as is shown by the red color in Fig. 3e, with the classical type of collagen fiber distribution as in nonirradiated gingival tissues.
Discussion
Detailed histological evaluation of the effect of fractional photothermolysis on human skin has been performed in several studies [1, 3, 4, 12, 23–26]. The scope of the problems discussed includes starting time of the different healing stages after laser irradiation, and the possible development of undesirable side effects, such as intradermal fibrosis and hypopigmentation, that are known to occur after skin ablative resurfacing with the CO2 and Er:YAG laser [12, 23–26].
This study is pioneering in the use of LPM in the oral mucosa and gingiva. Previous studies have shown that the stage of inflammation and re-epithelialization of nonirradiated oral mucosal wounds is shorter than that of skin wounds [8]. The goal of this research was to assess the mucosal healing following laser irradiation for different times and the possible development of side effects of LPM, such as epithelial dyskeratosis and spongiosis which are features of epithelial cell and subepithelial fibrotic degeneration resulting from inflammation. Histological analysis of the laser coagulation zone following irradiation with pulses of 80–150 ms revealed that 1 h after irradiation the epithelium was destroyed, the collagen was completely disorganized, and there were no signs of tissue viability within the coagulation columns (Figs. 2a, 3a). The epithelial layer was also destroyed, which is different from observations reported for non-ablative fractional skin treatment [4].
By days 1–2 after LPM, newly formed epithelial cells had replaced the thermally damaged cells (Figs. 2b, 4b) thus eliminating the nonvital area (initially visualized with viability stain) that was evident 1 h after LPM (Fig. 2a). This finding explains the minimal risk of infection, oozing or macroscopic crusting with this new treatment modality. By days 7–12 after LPM normalization of the epithelium was apparently complete with no residual dyskeratosis, spongiosis or subepidermal clefting (Figs. 2c, 3c, 4d). Based on the duration of the healing process, it has been suggested [12] that the interval between successive skin treatments should be at least 1 week. Since the rate of healing is similar, we believe that a similar time should be allowed between successive treatments of the oral mucosa or gingiva. Many reports of studies assessing histological skin healing after fractional treatment discuss the formation of epidermal necrotic debris [1, 3, 4, 12, 23–26]. Much attention has been paid to migration of the debris on the skin surface and the role in melanin washout. We did not observe similar migration of necrotic epithelial masses in the oral mucosal epithelium, which could be explained by a lower content of keratin in the tissue that contributed to holding such masses in the column area.
A pronounced reactive inflammation had developed in the column area 1 day after treatment, which enhances disorganization of injured collagen [27] (Fig. 4a). This may explain why the largest column recorded in the PSR-stained specimens under polarized light was observed only on day 2 after laser treatment (Fig. 5a). The intensity of cellular infiltration had reduced appreciably by day 12 of observation (Fig. 3c).
High activity of fibroblasts producing new collagen and forming a network of new thin-walled blood vessels was seen on day 5 (Fig. 4c). In this study tissue healing and regeneration was confirmed not only by the appearance of viable epithelial cells with NBTC staining, but also by the red color of restored collagen under polarized light with PSR staining of the column site. By day 12 new collagen had formed at all levels of structural organization, which was confirmed by its polarization properties (Fig. 5c), but in the subepithelial layer it had not yet become oriented horizontally (Fig. 5d). Keratinization processes differentiate new epithelium and these are signs of para- and hyperkeratosis. We were able to see enhanced functional activity of epithelial cells, including intensive keratohyalin and keratin synthesis resulting in para- and hyperkeratosis. Abundant new blood vessels was also observed.
By day 28 the tissue structure was restored almost completely, a slight increase in the number of small vessels was observed in the subepithelial layer with mild edema, and no signs of scarring were apparent. By day 90 the tissue structure was restored completely. No signs of dyskeratosis or spongiosis were seen in the epithelium and no signs of scarring were seen in the submucosa. Thus healing of the oral mucosa was complete.
Conclusion
A single LPM treatment induced a wound healing and regeneration response in the oral mucosa, which allows us to conclude that LPM is a promising method for treating degenerative diseases of the oral soft tissues. The size of the LPM laser columns in the oral mucosa increased with increasing pulse duration and reached a maximum depth-to-width ratio of 1.8 by 0.6 mm with a pulse of 150 ms. Exposure times may vary depending on the clinical application. The duration of healing suggests that LPM should not be repeated earlier than in 1 week after the first treatment to avoid complications associated with incomplete epithelial and stromal healing. Monitoring of the tissue structure over 3 months after LPM showed no signs of dyskeratosis and spongiosis in the epithelium and no signs of scarring in the submucosa.
References
Manstein D, Herron GS, Sink RK, Tanner H, Anderson RR (2004) Fractional photothermolysis: a new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg Med 34(5):426–438
Altshuler G, Smirnov M, Yaroslavsky I (2005) Lattice of optical islets: a novel treatment modality in photomedicine. J Phys D Appl Phys 38(15):2732–2747
Geronemus RG (2006) Fractional photothermolysis: current and future applications. Lasers Surg Med 38(3):169–176
Jih MH, Kimyai-Asadi A (2008) Fractional photothermolysis: a review and update. Semin Cutan Med Surg 27(1):63–71
Moretti M (2008) Fractional skin rejuvenation: a major new technology category. Medical Insight, Aliso Viejo, CA
Paulus YM, Jain A, Gariano RF, Stanzel BV, Marmor M, Blumenkranz MS, Palanker D (2008) Healing of retinal photocoagulation lesions. Invest Ophthalmol Vis Sci 49(12):5540–5545
Bedi VP, Chan KF, Sink RK, Hantash BM, Herron GS, Rahman Z, Struck SK, Zachary CB (2007) The effects of pulse energy variations on the dimensions of microscopic thermal treatment zones in nonablative fractional resurfacing. Lasers Surg Med 39(2):145–155
Szpaderska AM, Zuckerman JD, DiPietro LA (2003) Differential injury responses in oral mucosal and cutaneous wounds. J Dent Res 82(8):621–626
Altshuler GB, Anderson RR, Manstein D, Zenzie HH, Smirnov MZ (2001) Extended theory of selective photothermolysis. Lasers Surg Med 29(5):416–432
Hukki J, Lipasti J, Castren M, Puolakkainen P, Schroder T (1989) Lactate dehydrogenase in laser incisions: a comparative analysis of skin wounds made with steel scalpel, electrocautery, superpulse–continuous wave mode carbon-dioxide lasers, and contact Nd:YAG laser. Lasers Surg Med 9(6):589–594
Junqueira LC, Bignolas G, Brentani RR (1979) Picrosirius staining plus polarization microscopy, a specific method for collagen detection in tissue sections. Histochem J 11(4):447–455
Laubach HJ, Tannous Z, Anderson RR, Manstein D (2006) Skin responses to fractional photothermolysis. Lasers Surg Med 38(2):142–149
Sherwood ME, Flotte TJ (2007) Improved staining method for determining the extent of thermal damage to cells. Lasers Surg Med 39(2):128–131. doi:10.1002/lsm.20450
Burns JA, Kobler JB, Heaton JT, Lopez-Guerra G, Anderson RR, Zeitels SM (2007) Thermal damage during thulium laser dissection of laryngeal soft tissue is reduced with air cooling: ex vivo calf model study. Ann Otol Rhinol Laryngol 116(11):853–857
Baranoski S, Ayello EA (2008) Wound care essentials: practice principles, 2nd edn. Lippincott Williams & Wilkins, Philadelphia
Romanos GE, Schroeter-Kermani C, Hinz N, Wachtel HC, Bernimoulin JP (1991) Immunohistochemical localization of collagenous components in healthy periodontal tissues of the rat and marmoset (Callithrix jacchus). II. Distribution of collagen types IV, V and VI. J Periodontal Res 26(4):323–332
Romanos GE, Schroeter-Kermani C, Hinz N, Wachtel HC, Bernimoulin JP (1992) Immunohistochemical localization of collagenous components in healthy periodontal tissues of the rat and marmoset (Callithrix jacchus). I. Distribution of collagen types I and III. J Periodontal Res 27(2):101–110
Ramachandran GN, Reddi AH (1976) Biochemistry of collagen. Plenum, New York
Fratzl P (2008) Collagen: structure and mechanics. Springer, New York
Kesler G, Koren R, Kesler A, Kristt D, Gal R (2000) Differences in histochemical characteristics of gingival collagen after ER:YAG laser periodontal plastic surgery. J Clin Laser Med Surg 18(4):203–207
Matteini P, Rossi F, Menabuoni L, Pini R (2007) Microscopic characterization of collagen modifications induced by low-temperature diode-laser welding of corneal tissue. Lasers Surg Med 39(7):597–604
DiPietro LA, Burns AL (2003) Wound healing: methods and protocols. Humana, Totowa
Kim BJ, Lee DH, Kim MN, Song KY, Cho WI, Lee CK, Kim JY, Kwon OS (2008) Fractional photothermolysis for the treatment of striae distensae in Asian skin. Am J Clin Dermatol 9(1):33–37
Allemann IB, Kaufman J (2010) Fractional photothermolysis – an update. Lasers Med Sci 25:137
Hantash BM, Bedi VP, Kapadia B, Rahman Z, Jiang K, Tanner H, Chan KF, Zachary CB (2007) In vivo histological evaluation of a novel ablative fractional resurfacing device. Lasers Surg Med 39(2):96–107
Hantash BM, Bedi VP, Chan KF, Zachary CB (2007) Ex vivo histological characterization of a novel ablative fractional resurfacing device. Lasers Surg Med 39(2):87–95
Woolley DE, Evanson JM (1980) Collagenase in normal and pathological connective tissues. Wiley, Chichester
Acknowledgments
This work was supported by the Russian Federation State Contract no. 02.740.11.5149, and grant no. 10-02-01175 of the Russian Foundation for Basic Research. The authors are grateful to Gregory Altshuler, Dr.Sc., for stimulating and helpful discussions.
Conflicts of interest statement
Felix Feldchtein is an employee of Dental Photonics, a commercial company marketing laser patterned microcoagulation treatment.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Romanos, G.E., Gladkova, N.D., Feldchtein, F.I. et al. Oral mucosa response to laser patterned microcoagulation (LPM) treatment. An animal study. Lasers Med Sci 28, 25–31 (2013). https://doi.org/10.1007/s10103-011-1024-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-011-1024-9