Abstract
The aim of this study was to investigate the effect of power density and irradiation time of an argon laser on the physico-mechanical properties of light-cured dental nanocomposites. The composites were cured with 260 mW/cm2 and 340 mW/cm2 power densities at different irradiation times. The degree of conversion (DC), flexural strength, flexural modulus, water sorption, solubility and reaction temperature were measured. The maximum DC (50%), which was achieved after approximately 20 s irradiation, and the reaction temperature rise (20°C) were demonstrated by composite containing 20% filler cured at 340 mW/cm2. The composite with 25% filler cured at 340 mW/cm2 showed the highest flexural strength and modulus, which were 32.2 MPa and 1.89 GPa, respectively. The minimum water sorption (3.8%) and solubility (1.2%) were achieved with the composite containing 25% filler cured at 340 mW/cm2. Finally, the composite with 25% filler cured at 340 mW/cm2 showed higher physico-mechanical properties.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Light-cured restorative composites are prepared by the mixing of organic resin matrix with inorganic fillers. Fillers such as silicon dioxide (silica, SiO2), zirconium dioxide (zirconia, ZrO2), and aluminum trioxide (alumina, Al2O3) of micron or submicron particle size are usually used [1]. The organic matrix is often composed of methacrylate resins, such as 2,2-bis[4-(3-methacryloxy-2-hydroxypropoxy)phenyl] propane (Bis-GMA) and triethylene glycol dimethacrylate (TEGDMA). Bis-GMA is the primary organic ingredient in nearly every commercial restorative resin [2, 3]. Bis-GMA has become a vital monomer for dental restorative composites, due to its superior mechanical strength, less shrinkage, high modulus, and reduced toxicity because of its lower volatility and diffusivity into the tissue. Because of the very high viscosity of Bis-GMA, TEGDMA is added to the resin system to reduce its viscosity in order to enhance filler loading and, as a result, physical and mechanical properties [4, 5].
Recently, dental composites cured by visible light have been used, mostly because they are safer and easier to use than resin composite systems activated by ultra-violet (UV) light [6]. The use of argon laser for the photopolymerization of composite resin restoratives was introduced in the early 1980s [7]. This interest has arisen because the 472 nm wavelength of argon laser is optimal for the initiation of polymerization of composite resins, particularly when the camphorquinone, with broad peak activity in the 470 nm range, is used in dental composite as a photo-initiator [8]. In addition, lasers such as argon laser with its inherent optical characteristics, like generating one wavelength of blue light (i.e., the light is monochromatic), absorption selectivity because of wavelength tunability, coherency, collimation, low beam divergence, and fiber delivery capability, are suitable sources for the polymerization of composite resins, which effectively can provide a larger degree of conversion (DC) of monomers, reduce curing time and enhance physical properties of cured composites [9, 10].
Therefore, the objective of this study was to provide a composite with high physical and mechanical properties and low water sorption and solubility. It was anticipated that composites with methacrylate resin and silica nanofiller could fulfill these requirements. The inorganic phase is nanosized and homogeneously dispersed in the organic matrix. This research involved two parts: (1) preparation and curing of the composites; (2) characterization of the composites.
The inorganic nanoparticles were dispersed in resin to make an organic–inorganic composite. Photo-initiator was then added to the composites to be polymerized by irradiation with laser light. It was expected that such nanoparticles would satisfy the criteria for mechanical strength and hardness, while the organic phase would deliver the required fracture toughness. The physical and mechanical properties of composites, such as flexural strength, flexural modulus, water sorption, solubility and reaction temperature, depend on their resin compositions, filler type and filler content, and degree of conversion. These parameters were studied systematically. For nanocomposite, an improvement in physical properties was expected, due to the increased interfacial interactions between resin and fillers [11]. In this study, visible light-cured dental nanocomposites were developed, based on Bis-GMA, TEGDMA and nanosilica fillers.
Materials and methods
Preparation and curing of nanocomposites
Preparation of resin
We prepared the resin by mixing bisphenol A glycol dimethacrylate (Bis-GMA) and triethylene glycol dimethacrylate (TEGDMA) (Fig. 1) that were obtained from the Rohm company (Rohm GmbH, Chemische Fabrik, 64275 Darmstadt, Germany). The mass ratio of the mixture was 65:35.
Preparation of nanocomposite series A
We prepared a series of nanocomposites by mixing 16 g of resin, 40 ml of acetone and 4 g of SiO2 nanoparticles, with primary particles of size 10 nm, aggregated particles of size 50 nm and agglomerated particles in micrometer size, were supplied by Wacker Chemie AG (Germany). Series A nanocomposites involved 20% filler and 80% resin (by weight). The nanocomposites were made according to Chen et al. [1].
Preparation of nanocomposite series B
We prepared series B nanocomposites by mixing 15 g of resin, 40 ml of acetone and 5 g of SiO2 nanoparticles. The nanocomposite included 25% filler and 75% resin.
The nanocomposites were then placed in a sonication instrument (Bandelin, Sonopuls, HD2200, P150W/300W, AF Frey-35 kHz) for 10 min, to break up the agglomerates of SiO2 particles.
The initiator system used in this experiment was the visible light-initiating system of camphorquinone (CQ) (0.5 wt%) and N,N′-dimethyl amino-ethyl methacrylate (DMAEMA, 0.5 wt%) which were purchased from Fluka (Sigma-Aldrich Chemie GmbH, 82018 Taufkirchen, Germany). Finally, the acetone was completely removed by vacuum.
Curing of nanocomposites
An argon laser (Mellos Griot, 543 series; Carlsbad, CA, USA) at 472 nm, with different irradiation times and power densities, was employed to cure the nanocomposite samples, which were prepared by the molding method with different shapes and diameters. For the reactions at different power densities of laser beam, we selected two densities. The wave number mentioned led to a 340 mW/cm2 output. Meanwhile, we used a filter to obtain another power density (260 mW/cm2).
The flowchart of preparation and characterization of the dental nanocomposites is illustrated in Fig. 2.
Evaluation of nanocomposite
Degree of conversion
To measure the degree of conversion (DC%), we placed each uncured nanocomposite paste between two polyethylene films, pressed to form a very thin film, and the absorbance peaks were obtained by transmission mode of Fourier transform infrared spectrometer (Equinox 55, Bruker Optics, Göttingen, Germany). The samples were then irradiated by the 472 nm wavelength of the argon laser with power densities of 260 mW/cm2 and 340 mW/cm2, measured by a light meter (Coltene-Whaledent, Sussex, UK) for irradiation times of 5 s, 10 s, 20 s, 40 s and 60 s. After each exposure time, the specimens were again scanned for their absorbance peaks. The following equation shows the calculation of DC% [12]:
Flexural strength and flexural modulus
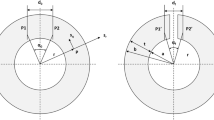
The flexural strength (FS) and flexural modulus (FM) were measured on the bar specimens (length 25 mm, width 2 mm, height 2 mm) with the three-point bending fixture of an SMT-20 universal testing machine (Santam, Tehran, Iran) with a span of 20 mm between supports and loaded to failure point at a crosshead speed of 0.5 mm/min using a 60 N load cell. The specimens were cured at 260 mW/cm2 and 340 mW/cm2 for 45 s and 35 s, respectively. Five specimens for each group were tested, and their mean value was determined. The flexural strength and flexural modulus were calculated from the following equations [13, 14]:
where f is the maximum force (newtons), l the distance between the supports (millimeters), b the specimen width, h the height of the bar (millimeters) and d the deflection under load (millimeters).
Solubility and water sorption
Disc-shaped specimens (1 mm thick and 5 mm in diameter) were prepared in stainless steel molds. The specimens were placed between two glass slides. Five specimens were prepared for each power density, and filler content, and each side of the specimens were irradiated with a 5 mm-diameter laser beam at 260 mW/cm2 and 340 mW/cm2 power densities for 45 s and 35 s, respectively. After irradiation, the weights of the specimens (m1) were measured with a precision of 0.0001 g. Then, the discs were immersed in distilled water for a week at room temperature so that unreacted monomers would be eliminated. After that, the specimens were removed, dried and stored in an oven at 37°C until a constant mass (m2) had been achieved. The solubility (SL) was determined from the following equation [15]:
The specimens were dipped again in distilled water at room temperature so that the water sorption (WS) could be measured, and, after different time periods, they were removed and blotted dry according to the ISO 4049 standard to remove excess water and were then weighed. Their weights were recorded until there were no significant changes in weight.
The value of water sorption was calculated for each specimen from the following equation [15]:
where, WSt denotes water sorption at time t, mt weight at time t and m2 initial weight.
Temperature rise
Five specimens for each case were prepared under the same condition as those for the solubility samples and then cured with different power densities and irradiation times, as mentioned above. For measurement of the temperature change a K-type thermocouple (CHY-502A1 thermometer, Tainan, Taiwan), whose output was connected to a computer to monitor and plot the thermal behavior continuously, was used. The temperature rise was then obtained by subtraction of the ambient temperature from the total temperature, that is equal to the sum of irradiation and chemical reaction temperature.
Statistical analysis
The experimental results were examined by one-way analysis of variance (ANOVA), based on quintuplicate specimens for DC, flexural modulus and flexural strength, solubility and water sorption testing. Multiple pairwise comparisons were further conducted, using Tukey’s test with a significance level of 0.05.
Results
Figure 3 shows the characteristic Fourier transform infrared (FTIR) spectra of uncured and cured specimens at 260 mW/cm2 and 340 mW/cm2 within a wave number range of 1,690–1,570/cm. The quantity of the remaining double bonds was determined by a method described by Ruyter and Gyorosi [16]. Remaining unconverted double bonds were calculated by comparison of the ratio of aliphatic C=C absorption at 1,638/cm to aromatic carbon–carbon absorption at 1,608/cm between cured and uncured specimens (Fig. 3). The absorption of the aromatic carbon–carbon stretching band remains constant during the polymerization reactions and serves as an internal standard. The DC was determined by subtraction of the percentage of residual aliphatic C=C bonds from 100%.
a FTIR spectra of uncured nanocomposite containing 20% filler with a frequency range between 3,900/cm and 400/cm. b FTIR spectra of nanocomposite containing 20% filler cured at 340 mW/cm2, with a frequency range between 3,900/cm and 400/cm. c FTIR spectra of uncured and cured nanocomposites at 340 mW/cm2, involving 20% filler, with a frequency range between 1,690/cm and 1,570/cm
Commercial dental restorative materials are usually polymerized in fewer than 60 s, with a degree of conversion from 40% to 75%. The residual heat of polymerization decreased with longer curing time. The relationship between degree of conversion and irradiation time for specimens cured at 260 mW/cm2 and 340 mW/cm2 and composed of 20% and 25% filler is shown in Fig. 4. The results show that higher resin concentration and power density resulted in a higher degree of conversion. Thus, for maximum conversion (50%) to be achieved, the composite containing 20% filler can be cured after approximately 20 s at 340 mW/cm2.
Figure 5 shows the comparison of stress–strain curves for specimens cured with different power densities and filler content. As shown, a given stress is required for each composite to break down. The results of flexural strength and flexural modulus at different power densities and filler content are shown in Figs. 6 and 7. The figures clearly illustrate that maximum flexural strength and flexural modulus of the cured composites can be achieved by increasing the intensity and percentage of filler.
Solubility and water sorption in dental composites result in the release of unreacted monomers, which lead to toxicity and allergic reactions in patient. Figures 8 and 9 depict the values of solubility and water sorption for specimens cured with different power densities and filler content. As can be seen, the solubility and water sorption decreased as the intensity and filler loading of nanocomposites increased. Therefore, the minimum solubility (1.2%) and water sorption (3.8%) were obtained for the composite containing 25% filler cured at 340 mW/cm2.
Since, polymerization is an exothermic reaction, analysis of the temperature rise during the irradiation process is very important. The amount of temperature change was related to factors such as percentage of resin used in the composition, power density, curing time and degree of conversion. Figure 10 illustrates the temperature rise of the cured nanocomposites with the power densities and filler content used.
Discussion
Dental restorative composites are cured with visible light, because light sources with shorter wavelengths, such as UV, may harm the surrounding tissue. Thus, camphorquinone (CQ) is used as the photo-initiator, which has a maximum light absorption at 470 nm in the visible region. We examined the effects of argon laser intensity and filler loading on the conversion, water sorption and mechanical properties of dental nanocomposites containing nanosilica filler and a mixture of Bis-GMA and TEGDMA as resin and a photo-initiator system including camphorquinone and N,N′-dimethyl amino-ethyl methacrylate.
The two major components of dental composites are the polymer matrix and the filler particles. Changes in composition and chemistry of the constituent monomers and filler can alter the physical properties of the materials. For example, increasing the ratio of TEGDMA to Bis-GMA in a polymethacrylate network was shown to increase water uptake [4–6, 14] and alter the strength and hardness of the material [15]. Soares and Pinheiro found a positive correlation between volume fraction of the filler and diametral tensile strength, irrespective of the chemistry of the polymer matrix [17].
Owing to its high mechanical strength, low volatility, and relatively low polymerization shrinkage, Bis-GMA is the primary component in a majority of commercial dental resins [2]. However, Bis-GMA is also characterized by a very high viscosity and low polymerization conversion. Hence, 20–50 wt% of less viscous dimethacrylates such as TEGDMA are added to improve handling of the dental formulations, as well as to achieve higher DC due to the increase in the mobility of the molecules, as mentioned before [2, 4].
The addition of TEGDMA is also associated with increased volumetric shrinkage due to the higher concentration of double bonds in TEGDMA and increased overall double bond conversion [5]. Bis-GMA/TEGDMA resins also exhibit a high shrinkage stress, which contributes to premature failure or reduced overall performance of the restoration [6, 7].
Colloidal silica nanoparticles were used as fillers. The outer shell of colloidal particles is surrounded by hydroxyl groups [12]. Negative effects could result from too many nucleophilic −OH groups at high concentrations of SiO2, which may react with all of the cationic (electrophilic) photo-initiator. Thus, photo-initiated cationic polymerization of the epoxy resin cannot occur [13]. Therefore, it is not desirable to have high filler loading in the nanocomposite.
It is worth mentioning that Chen et al. demonstrated that, when the content of inorganic fillers was increased, the nanocomposites remain light curable but exhibit low microhardness. This might result from the inadequate concentrations of epoxy to cover all silica nanoparticles evenly [1].
High power density can also result in a high degree of conversion and mechanical strength and low solubility and water sorption. The degree of conversion is a major factor in the physical properties of dental composites and depends on several factors, such as the chemical structure of the dimethacrylate monomers, the polymerization conditions, photo-initiator concentration, power density, light source and light wavelength [17, 18]. In general, a low DC% of composites at a lower light intensity can cause lower free radical formation than when higher light intensity is used. In addition, a low DC% may give inadequate wear resistance and low bonding stability to the tooth surface, which results in clinical problems such as marginal shrinkage [19]. However, the degree of conversion can be increased at high power density and resin content (Fig. 3). The enhanced conversion is reflected in the resultant improvement in physical properties and flexural strengths.
The temperature change is an important factor that should be noticed during the polymerization of dental composites. The rise in temperature indicated that, when the intensity is increased, an increase in total temperature rise during polymerization is seen, which is partly due to radiation and partly due to the reaction (Fig. 9). Therefore, the maximum of DC% and temperature rise occurred when the content of inorganic filler was 20% and the applied power density was 340 mW/cm2. Increasing the intensity and, hence, the cure temperature can increase the mobility of the reacting media and rate of network formation. Thus, these factors can enhance the polymerization rate.
The required stress for each broken-down composite versus strain is shown in Fig. 4. The comparison of the stress–strain curves showed that, with an increase in the density of the light source and filler loading of the nanocomposite, the required stress for each given strain is increased. It should be noted that the shape of the stress–strain curve for such composites is often not unique, as the value of the strain produced depends upon the rate at which the stress is applied.
Since dental composites as restorative materials must possess acceptable mechanical properties to withstand chewing force, the flexural strength test is very important. Figures 5 and 6 illustrate the flexural strengths and flexural moduli of the nanocomposites. High intensity enhances mechanical strength due to increasing of the degree of conversion. High filler loading can also improve the mechanical properties due to hardness of this component.
Other important parameters affecting the physico-mechanical properties of dental composite are solubility (SL) and water sorption (WS). It should be noticed that water is absorbed within the matrix resin and is most affected by the structure and the amount of this phase. Therefore, the evaluation of the solubility and water sorption of dimethacrylate resins is important in understanding their behavior in the composite. Figure 7 depicts the values of solubility of the specimens. It is known that the unreacted monomer can be trapped during polymerization inside the micro-gels between the polymer chains, and it is absorbed into the surrounding network or is trapped in the micropores. The monomer in the micropores is more susceptible to leaching out than the monomer inside the micro-gels. The results confirmed that the values of solubility depend on percentage of degree of conversion, i.e., the low amount of the unreacted monomer and the low solubility value are due to the high DC%. The absorbed water in the composites can act as a plasticizer, and, hence, it reduces their hardness [20]. The investigation of the water sorption of the nanocomposites showed that it follows the same pattern. The results indicated a rapid increase during the first 3 days, and then the curves reached a plateau. As observed in Figs. 7 and 8, increasing the intensity and filler loading was effective in minimizing the solubility and water sorption of the nanocomposites. The results showed that the nanocomposite with 25% nanosilica, which cured at 340 mW/cm2, exhibited the maximum flexural strength and modulus and the minimum solubility and water sorption. Thus, it is evident that the use of high power density and filler loading can provide a composite with higher physical and mechanical properties. Application of the argon laser and choice of an appropriate wavelength that is close to the absorption peak of the initiator can increase the penetration depth of light into the dental composites, reduce the curing time to approximately 20 s at a power density of 340 mW/cm2, and improve the physical and mechanical properties.
Conclusions
A visible light-cured nanocomposite with high strength, low solubility and water sorption, high degree of conversion and low temperature rise was developed. The nanocomposites’ formulations were 80/20 wt% and 75/25 wt% nanosilica filler/resin (65/35 wt% Bis-GMA/TEGDMA). The nanocomposites were irradiated with 260 mW/cm2 and 340 mW/cm2 for 45 s and 35 s, respectively. According to this study, it was found that, by using high power density and filler loading, we improved flexural strength, flexural modulus, solubility and water sorption of the nanocomposites. However, an increase in the power density also increased the maximum temperature rise during polymerization. Furthermore, the developed nanocomposite containing 25% nanosilica that cured at 340 mW/cm2 demonstrated low solubility and water sorption and high strength and is suitable for application as a dental restorative material. Finally, the application of argon laser with optimum power density for the curing of dental composites is very suitable for dentistry due to the lack of side effects for patient and dentist, access to appropriate degree of conversion in a short time, and reduction of the polymerization temperature that can decrease pulp damage.
References
Chen M, Chen C, Hsu S, Sun SH, Su W (2006) Low shrinkage light curable nanocomposite for dental restorative material. Dent Mater 22:138–145
Bowen RL (1962) Patent US 3066112
Bowen RL (1962) Compatibility of various materials with oral tissues. I: The components in composites restorations. J Dent Res 58:1493–503
Sankarapandian M, Shobha H (1997) Characterization of some aromatic dimethacrylates for dental composite applications. J Mater Sci Mater Med 8:465–468
Khosroshahi ME, Atai M, Nourbakhsh MS (2007) Photopolymerization of dental resin as restorative material using an argon laser. Lasers Med Sci . doi:10.1007/s10103-007-0487-1
Sun G, Chae K (2000) Properties of 2, 3 butanedione and 1phenyl-1, 2-propanedione as new photosensitizer for visible light cured dental resin composites. Polymer 41:6202–6212
Blankenau R, Kelsey WP, Kutsch VK (1995) Clinical applications of argon laser in restorative dentistry. In: Miserendino LJ, Pick RM (eds) Lasers in dentistry. Quintessence Publishing, Chicago, pp 217–230
Kelsey W, Blankenau R, Powell G, Barkmeier W (1989) Enhancement of physical properties of resin restorative materials by laser polymerization. Lasers Surg Med 9:623–627
Fleming M, Mailet W (1999) Photopolymerization of composite resin using the argon laser. Clin Pract 65:447–450
Conrado L, Munin E, Zangaro R (2004) Root apex sealing with different filling materials photopolymerized with fiber optic delivered argon laser light. Lasers Med Sci 19:95–99
Giannelis EP (1996) Polymer layered silicate nanocomposites. Adv Mater 8:29–35
Nunes TG, Pereira SG, Kalachandra S (2008) Effect of treated filler loading on the photopolymerization inhibition and shrinkage of a dimethacrylate matrix. J Mater Sci Mater Med 19:1881–1889
Craig R (ed) (1997) Restorative dental materials, 10th edn. Mosby, St. Louis, MO
Lovell L, Lu H, Elliott J, Stanburg J, Bowman C (2001) The effect of cure rate on the mechanical properties of dental resins. Dent Mater 17:504–511
Ogliari F, Ely C, Zanchi C, Fortes C, Samuel S, Demarco F, Petzhold C, Piva E (2008) Influence of chain extender length of aromatic dimethacrylates on polymer network development. Dent Mater 24:165–171
Ruyter IE, Gyorosi PP (1976) An infrared spectroscopic study of sealants. Scand J Dent Res 84:396–400
Soares MA, Pinheiro A (2003) Degree of conversion of composite resin: a Raman study. J Clin Laser Med Surg 6:357–362
Selli E, Bellobono I (1993) Photopolymerization of multifunctional monomers: kinetic aspects, in radiation curing in polymer science and technology, vol. III. Elsevier, Amsterdam, pp 1–32
Barszezewska-Rybarek I, Gibas M, Kurcok M (2000) Evaluation of the network parameters in aliphatic poly urethane dimethacrylate by dynamic thermal analysis. Polymer 41:3129–3135
Atai M, Nekoomanesh M, Hashemi SA, Amani S (2004) Physical and mechanical properties of an experimental dental composite based on a new monomer. Dent Mater 20:663–668
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mirsasaani, S.S., Atai, M.M. & Hasani-Sadrabadi, M.M. Photopolymerization of a dental nanocomposite as restorative material using the argon laser. Lasers Med Sci 26, 553–561 (2011). https://doi.org/10.1007/s10103-009-0699-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-009-0699-7