Abstract
The purpose of this study was to compare the compositional changes and microhardness of the cavity floor prepared by erbium, chromium:yttrium–scandium–gallium–garnet (Er,Cr:YSGG) laser irradiation with those of the conventional bur-prepared cavity. A total of 16 extracted human molar teeth (with no carious lesions or repairs) were selected for this study. On the buccal and lingual (palatal) surfaces of each tooth, cavities (diameter 3 mm, depth 2 mm) were prepared with an Er,Cr:YSGG laser system (Waterlase MDTM, USA) and high-speed turbine. The cavities were cross-sectioned and subjected to atomic analysis by scanning electron microscopy–energy dispersive X-ray spectrometry (SEM-EDX) and Vickers hardness test. Statistical analyses were performed with t-tests. Surface characteristics of the prepared cavities were also investigated by SEM. No significant differences were found between the calcium/phosphorus (Ca/P) ratio and Vickers hardness of laser- and bur-prepared cavities. The SEM observation revealed that the lased cavity surface was irregular, and there was also an absence of smear layer; the orifices of dentinal tubules were exposed. Microhardness measurement of the cavity floor confirmed that the Er,Cr:YSGG laser produced a clean-cut surface of the cavity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since the development of the ruby laser by Maiman in 1960, several types of lasers, such as carbon dioxide (CO2) and neodymium:yttrium–aluminum–garnet (Nd:YAG) lasers, have been introduced into the dental clinic, to remove carious dental hard tissues or to prepare cavities, in anticipation of replacing the high-speed dental drill. For the determination of a method without any thermal side effects, the potential application of the erbium:yttrium–aluminum–garnet (Er:YAG) and erbium, chromium:yttrium–scandium–gallium–garnet (Er,Cr:YSGG) lasers have been introduced because of preparation without thermal side effects. Thus, their application in the dental clinic has been expected. These lasers can ablate enamel and dentine due to their highly efficient absorption in both water and hydroxyapatite [1].
The ability of Er:YAG laser to remove enamel and dentine was found to be comparable with that achieved with the conventional dental drill [2, 3]. It produces minimal thermal damage to the pulp or surrounding tissues, especially when irradiation is accompanied by a continuous water spray [4–6]. Histological studies in animals have shown that the pulp’s response to the Er:YAG laser appears to be similar to the response to a high-speed hand piece [7]. On the other hand, the Er,Cr:YSGG) laser has been shown to be effective for soft-tissue surgery as well as for cutting enamel, dentine and bone. When dental hard tissues were irradiated by the Er,Cr:YSGG laser accompanied with a water spray, not only could the temperature be suppressed, but cutting efficiency could also be increased [8, 9].
Histological studies have shown that no pulpal inflammatory responses could be identified when Er,Cr:YSGG laser was used with a water spray [10–12]. Surface alterations of the enamel and dentine after Er,Cr:YSGG laser irradiation showed that these surfaces were associated with micro-irregularities, and there was also the absence of a smear layer [9]. From those results, it can be considered that Er,Cr:YSGG laser irradiation is a favourable technique in the removal of carious dentine or for cavity preparation, because it does not damage the dental pulp or surrounding tissues. However, there are few reports on the compositional changes and microhardness of the cavity floor prepared by Er,Cr:YSGG laser irradiation.
Therefore, this study was performed to compare the compositional changes and Vickers hardness of the cavity floor prepared by Er,Cr:YSGG laser irradiation with that of the conventional bur-prepared cavity. Surface characteristics of the prepared cavities were also investigated by light microscopy (LM) and scanning electron microscopy (SEM).
Materials and methods
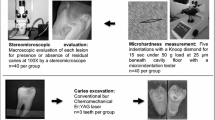
A total of 16 extracted human molar teeth with no carious lesions were used for this study. On the buccal and lingual (palatal) surfaces of each tooth, two shallow cavities (diameter 3 mm, depth 2 mm) were prepared, one with the laser system and one with a high-speed turbine (Figs. 1 and 2). From these teeth, 16 laser-prepared and 16 bur-prepared cavities were produced.
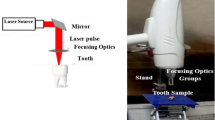
Laser cavities were prepared with an Er,Cr:YSGG laser system (Waterlase MDTM, USA) emitting at a wavelength of 2.78 µm, with a pulse duration of 140 μs and a pulse repetition rate of 20 Hz. The output power could be varied from 0 W to 6 W. The beam spot size was 400 μm. Irradiation was performed according to the manufacturer’s instructions; at the beginning of cavity preparation, we carefully performed laser irradiation in contact mode to remove enamel, with a beam of 6 W at 75% air pressure level and 85% water level (as shown on the laser equipment). As enamel removal progressed and the treated cavity floor became deeper and closer to the underlying dentine layer, we reduced the power to 3 W (33.9/J cm2) at 50% air level and 75% water level.
The control sites were prepared with a high-speed turbine with a no. 3411 diamond bur. The following experiments were performed during and after cavity preparation: assessment during cavity preparation; atomic analysis, and Vickers hardness measurement of the cavity floor.
Sixteen laser-prepared and 16 bur-prepared cavities were cross-sectioned perpendicularly to the tooth axis through the middle of the treated cavity; one half was used for atomic analysis by scanning electron microscopy–energy dispersive X-ray spectrometry (SEM-EDX) and the other half was used for the Vickers hardness test.
For the SEM-EDX, cut sections were fixed with a 10% formalin solution for 48 h and then immediately perfused with a phosphate-buffered solution of pH 7.3 at room temperature and rinsed with distilled water. The samples were dehydrated through a graded ethanol series (80%, 95% and 100%) for 24 h at each concentration, and then the irradiated areas were flattened as much as possible by polishing. They were sputter-coated with a carbon-coating device (HUS- 5 GB) and were examined by SEM-EDX at 25 kV accelerating voltage, tilt angle of 90°, and ×40 magnification.
For Vickers hardness measurement of the cavity floor, cross-sectional surfaces were polished. As obtaining a Vickers hardness measurement of the cavity surface was impossible, recordings were obtained below the cavity floor; the hardness of the subsurface at a point 30 μm below the cavity floor was used as that of the cavity floor. The Vickers hardness number (VHN) was measured in each treated cavity by the application of a 25 g load for 15 s by means of a hardness tester. The mean of the measurements was used as the VHN of cavity floor dentine, and statistically significant differences between the VHN of the laser and bur groups were determined by t- test.
Cross-sections of laser and bur cavities were examined by SEM. Specimens were dehydrated in a graded series of aqueous ethanol (80%, 95% and 100% ethanol) for 24 h in each solution, coated with a layer of AU, and observed by SEM at 20 kV.
Results
The results of atomic analysis showed that the quantities of phosphorus (P weight %) and calcium (Ca weight %) were reduced in the laser-treated cavity floor compared with those in the bur-prepared cavity floor. (Table 1). However, no significant differences were found between the Ca/P ratio of laser and bur cavities (P = 0.7). Furthermore, there were no significant differences in the VHN of lased and bur-prepared cavity floor) P = 0.068) (Table 1).
The SEM observation showed a scaly appearance or irregular surface due to micro-irregularities after laser irradiation (Fig. 3). In addition, there was an absence of smear layer; the orifices of dentinal tubules were exposed. In bur-prepared cavities SEM revealed a relatively flat appearance, and the surface was almost covered with a debris-like smear layer. Dentinal tubule orifices were plugged (Fig. 4).
Discussion
Cavity preparation was begun with laser irradiation in contact mode, with a maximum energy density of 6 W (67.9 J/cm2). Cutting the enamel by laser has a lower efficiency than cutting the dentine, because there is less water and organic content in enamel structures [9, 13]. When the treated cavity floor became deeper and closer to the underlying dentine layer, we reduced the power to 3 W (33.9/J cm2). In the clinic it is possible to reduce the time by increasing the energy densities; in particular, the output power can be increased for cutting the dentine, but it may increase the risk of thermal damage and was therefore avoided for this study.
No pulpal inflammatory responses could be identified in Er,Cr:YSGG laser irradiation with a water spray, as reported in previous histological studies [14, 15]. Clinical reports also showed that, when the use of a bur was compared with the use of a laser system, patients felt less pain during cavity preparation, and, in some cases, anaesthesia was not needed [16].
SEM-EDX revealed that the quantities of Ca or P in the lased areas were increased significantly when compared with those in bur preparation. It is likely that, during the laser irradiation, an increase in Ca or P was achieved because organic components evaporated; these changes have been ascribed to an increase in temperature in the irradiated area [17].
However, no significant difference between the Ca/P ratio of lased and bur cavities were found in our study. Therefore, it can be considered that one can achieve minimal heat-induced changes in dentine components after Er,Cr:YSGG irradiation with a water mist [17].
Microhardness measurement of the cavity floor confirmed that Er,Cr:YSGG laser produces clean-cut surfaces of the cavity. No statistically significant differences were found in the microhardness of laser and bur cavity floor. These results corresponded with those in a previous study using the Er:YAG laser [12]. An increase in Knoop hardness of the cavity floor caused by fusion of the dental hard tissues after CO2 and Nd:YAG laser irradiation has been reported in previous studies [18, 19]. The laser cavity surface had a marked resistance to artificial secondary caries when compared with mechanical removal. On the other hand, due to the increase in temperature, higher energy densities of laser irradiation actually decreased the microhardness of the dental hard tissues significantly. This condition has been said to be unsuitable for improving the properties of dental hard tissues [20]. It has also been reported that an increase in temperature during laser irradiation results in some major thermal side effects, such as melting, cracking of enamel or dentine, and an increase in the pulpal temperature [21–23]. The results of SEM in the laser cavities showed some particular characteristic features. The lased cavity surface was irregular, and there was an absence of smear layer; the orifices of the dentinal tubules were exposed. Typically, these structures were similar to the surfaces after Er:YAG or Er,Cr:YSGG laser irradiation and have previously been described as scaly or flaky, or as an irregular surface [2–4]. It is believed that micro-irregularity is associated with the microexplosion effects proposed as the mechanism of hard tissue ablation with Er:YAG laser or Er,Cr:YSGG laser [1]. Bur-prepared cavities, on the other hand, showed a relatively flat appearance and exhibited a debris-like smear layer, which might interfere with adhesion, wetting, penetration and hardness of the prepared cavity.
Conclusions
Based on the results of atomic analysis in our study, the quantities of P (P weight %) and Ca (Ca weight %) were reduced in the laser cavity floor compared with those in the bur treatment. However, no significant differences were found between the Ca/P ratio of laser- and bur-prepared cavities. Furthermore, there were no significant differences in the VHNs of lased and bur cavity floors. SEM observation showed a scaly appearance or irregular surface due to micro-irregularities after laser irradiation. In the bur-prepared cavities, SEM revealed a relatively flat appearance. Thus, this suggests that cavities can be prepared with laser in the clinic.
References
Wigdor HA, Walsh JT Jr, Featherstone JD, Visuri SR, Fried D, Waldvogel JL (1995) Laser in dentistry. Lasers Surg Med 16:103–133. doi:10.1002/lsm.1900160202
Hibst R, Keller U (1989) Experimental studies of the application of the Er:YAG laser on dental hard substances, I. Measurement of the ablation rate. Lasers Surg Med 9:338–344. doi:10.1002/lsm.1900090406
Keller U, Hibst R (1989) Experimental studies of the application of the Er:YAG laser on dental hard substances, II. Light microscopic and SEM investigations. Lasers Surg Med 9:345–351. doi:10.1002/lsm.1900090406
Hossain M, Nakamura Y, Yamada Y, Kimura Y, Matsumuto N, Matsomuto K (1999) Ablation depths and morphological changes in human enamel and dentin after Er:YAG laser irradiation with or without water mist. J Clin Laser Med Surg 17:105–109
Burkes EJ Jr, Hoke J, Gomes E, Wolbarsht M (1992) Wet versus dry enamel ablation by Er:YAG laser. J Prosthet Dent 67(6):847–851. doi:10.1016/0022-3913(92)90599-6
Visuri SR, Walsh JT Jr, Wigdor HA (1996) Erbium laser ablation of dental hard tissue: effect of water cooling. Lasers Surg Med 18:294–300. doi:10.1002/(SICI)1096-9101(1996)18:3<294::AID-LSM11>3.0.CO;2-6
Sonntag KD, Klitzman B, Burkes EJ, Hoke J, Moshonov J (1996) Pulpal response to cavity preparation with the Er:YAG and Mark III free electron lasers. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 81:695–702. doi:10.1016/S1079-2104(96)80076-X
Eversole LR, Rizoiu IM (1995) Preliminary investigations on the utility of an Er, Cr:YSGG laser. J Clin Dent Assoc 23:41–47
Hossain M, Nakamura Y, Yamada Y, Kimura Y, Matsumuto N, Matsomuto K (1999) Effects of Er, Cr:YSGG laser irradiation in human enamel and dentine: ablation and morphological studies. J Clin Laser Med Surg 17:155–159
Eversole LR, Rizoiu I, Kimmel AI (1997) Pulpal response to cavity preparation by an Er, Cr:YSGG laser powered hydrokinetic system. J Am Dent Assoc 128:1099–1106
Rizoiu I, Kohanghadosh F, Kimmel AL, Eversole IR (1998) Pulpal thermal responses to an erbium,chromium: YSGG pulsed laser hydrokinetic system. Oral Surg Oral Med Oral Pathol Oral Radiol Endo 86:220–223
Aoki A, Ishikawa I, Yamada T, Otsuki M, Watanabe H, Tagami J, Ando Y, Yamamoto H (1998) Comparison between Er:YAG laser and conventional technique for root caries treatment in vitro. J Dent Res 77:1404–1414. doi:10.1177/00220345980770060501
Li ZZ, Code JE, Van de Merwe WP (1992) Er:YAG laser ablation of enamel and dentin of human teeth: determination of ablation rates at various fluence and pulse repetition rates. Lasers Surg Med 12:625–630. doi:10.1002/lsm.1900120610
Zach L, Cohen G (1965) Pulp response to externally applied heat. Oral Surg Oral Med Oral Pathol 19:515–530. doi:10.1016/0030-4220(65)90015-0
Eversole LR, Rizoiu I, Kimmel AI (1997) Pulpal response to cavity preparation by an Er, Cr:YSGG laser powered hydrokinetic system. J Am Dent Assoc 128:1099–1106
Hadley J, Younge DA, Eversole LR, Gornvein JA (2000) A laser-powered hydrokinetic system for caries removal and cavity preparation. J Am Dent Assoc 131:777–785
Rohanizadeh R, LeGeros RZ, Fan D, Jean A, Daculsi G (1999) Ultrastructural properties of laser-irradiated and heat-treated dentin. J Dent Res 78):1829–1835. doi:10.1177/00220345990780121001
Marquez F, Quitana E, Roca I, Salgado J (1993) Physical-mechanical effects of Nd:YAG laser of sound dentin and enamel. Biomaterials 14:313–316. doi:10.1016/0142-9612(93)90124-K
Konishi N, Fried D, Staninec M, Featherstone JD (1999) Artificial caries removal and inhibition of artificial secondary caries by pulsed CO2 laser irradiation. Am J Dent 12:213–216
Kuramoto M, Matson E, Turbino ML, Marques RA (2001) Microhardness of Nd:YAG laser irradiated enamel surfaces. Braz Dent J 12(1):31–33
Frentzen M, Koort HJ (1990) Lasers in dentistry: new possibilities with advancing laser technology. Int Dent J 40:323–332
Wigdor H, ABT E, Ashrafi S, Walsh JT (1993) The effect of laser on dental hard tissues. J Am Dent Assoc 124:65–70
Israel M, Cobb CM, Rossmann JA, Spencer P (1997) The effect of CO2, Nd:YAG and Er:YAG lasers with and without surface coolant on tooth root surfaces: an in vitro study. J Clin Periodontol 24:595–600. doi:10.1111/j.1600-051X.1997.tb00235.x
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shahabi, S., Zendedel, S. Atomic analysis and hardness measurement of the cavity prepared by laser. Lasers Med Sci 25, 379–383 (2010). https://doi.org/10.1007/s10103-009-0692-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-009-0692-1