Abstract
Carpal tunnel syndrome (CTS) is an entrapment neuropathy of the median nerve at the wrist. It is one of the most common peripheral nerve disorders. The cause of idiopathic CTS remains unclear. The diagnosis of CTS is still mainly clinical. Open carpal tunnel release is the standard treatment. The present study was conducted to evaluate the effectiveness of low level laser treatment (LLLT) for CTS in comparison to the standard open carpal tunnel release surgery. Out of 54 patients, 60 symptomatic hands complaining of CTS were divided into two equal groups. Group A, was subjected to LLLT by Helium Neon (He–Ne) laser (632.8 nm), whereas group B was treated by the open approach for carpal tunnel release. The patients were evaluated clinically and by nerve conduction studies (NCSs) about 6 months after the treatment. LLLT showed overall significant results but at a lower level in relation to surgery. LLLT showed significant outcomes in all parameters of subjective complaints (p ≤ 0.01) except for muscle weakness. Moreover, LLLT showed significant results in all parameters of objective findings (p ≤ 0.01) except for thenar atrophy. However, NCSs expressed the same statistical significance (p ≤ 0.01) after the treatment by both modalities. LLLT has proven to be an effective and noninvasive treatment modality for CTS especially for early and mild-to-moderate cases when pain is the main presenting symptom. However, surgery could be preserved for advanced and chronic cases. Refinement of laser tools and introduction of other wavelengths could make LLLT for CTS treatment a field for further investigations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Carpal tunnel syndrome (CTS), an entrapment neuropathy of the median nerve at the wrist, is one of the commonest peripheral nerve disorders with a general prevalence of about 1%. Female preponderance varies from 23:1 to 3:1 [1, 8].
There is an established link between the raised intracarpal canal pressure and clinical CTS. Nerve injury is suggested to arise from the intermittent pressure effects on the median nerve circulation. Raised intracarpal canal pressure may be because of space-occupying lesions that are usually absent in most cases. In idiopathic CTS, the cause of increased canal pressure remains unclear. There seems to be an increase in the connective tissue within the carpal canal, mostly in the form of noninflammatory synovial fibrosis of an unclear mechanism [4].
Recently, there is controversy regarding the role of biochemical and structural processes in the increased connective tissue with CTS. Several studies suggested an increased expression of prostaglandin E2 (PGE2) and vascular endothelial growth factor (VEGF) in synovial tissue biopsy denoting a particular activity in the disease progression [9]. Moreover, an increased expression of matrix metalloprotein-2 in small arterioles was correlated with pain intensity, which clarified that pain may be a more prominent feature of early CTS and not related to the median nerve itself [10].
The mainstay for CTS diagnosis remains the clinical assessment of the patient’s history, with nocturnal paresthesia in the median nerve distribution being the most characteristic symptom. Definite sensory and motor signs are elicited in more advanced cases [2, 16]. Moreover, different clinical tests could be used to establish the diagnosis of CTS with different reported results [4].
Nerve conduction studies (NCSs) can help to confirm the diagnosis of CTS and to exclude other lesions. They had a lower sensitivity when compared with the clinical diagnosis, as 22% of the clinically definite CTS patients had normal NCSs [3, 4, 16, 20].
Imaging modalities are other promising investigations that could be used for the diagnosis of CTS. The most sensitive morphologic finding is the expansion of the median nerve in or just proximal to the carpal tunnel with a cross-sectional nerve surface area >10.03 mm2 [6]. Other investigators confirmed, by the use of ultrasonic measurement, the risk of CTS with a high wrist ratio (>0.7) [12] instead of external wrist dimensions [5]. However, it has not yet been clearly shown that imaging can offer any additional advantage regarding selection of the treatment modality [4].
Treatment of CTS could be categorized into nonsurgical and surgical treatment. Nonsurgical treatment includes the following: nonsteroidal anti-inflammatory drugs (NSAIDs), local steroid injection, and wrist splinting [19]. On the other hand, surgical treatment for CTS means carpal tunnel release. The first open carpal tunnel release is credited to Learmonth in 1929 and it was later popularized by Phalen et al. in the 1950s. Since then, open approach had been the standard treatment for CTS. However, to obviate the complications associated with open approach for carpal canal release, including hypertrophic or painful scars, and the slow return of pinch and grip strength, the endoscopic approach has been introduced by Okutsu et al. [7, 17, 18].
Occasionally, trials of alternative modalities for treatment of CTS are carried out. These include the introduction of low level laser treatment (LLLT) for CTS [11, 15]. Many investigators demonstrated the potential beneficial effects of LLLT. These include enzymatic effects on acetylcholine esterase, stimulation of fibroblast proliferation, absolute increase in microcirculation, and stimulation of RNA, DNA, and ATP synthesis. Collectively, LLLT has proven to have a role in pain influence and inflammatory process in the biotissues [13, 14].
Apart from the definite mechanism of LLLT, it was found of interest to evaluate the effectiveness of low level laser in comparison to the standard open carpal tunnel release surgery for the treatment of CTS.
Patients and methods
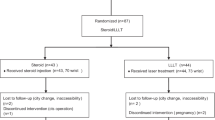
Out of 54 patients, 60 symptomatic hands complaining of CTS were studied. Patients’ data, subjective complaints including history of previous interventions, physical examination, and NCSs were investigated. Patients were divided into two equal groups (A and B). Each group included 27 patients with 30 affected hands taking into consideration that each bilaterally affected patient (n = 6 patients) was included in one treatment group for one hand and in the other treatment group for the contralateral hand.
Group (A), low level laser therapy
Helium Neon (He–Ne) laser (632.8 nm, Level Laser M300) in continuous wave (CW) mode was used. The instrument has 25 prestored programs including a program for CTS. A minimum power of 12 mW has been used. The X–Y dimensions of the area to be treated were measured and the distance between laser head and area to be treated (height) should be accurately fixed at 30 cm. The area to be treated extends from the proximal palmer crease to the distal wrist crease and laterally from the scaphoid tuberosity to the pisiform bone. It was exposed to LLLT through a sweeping computerized scanning at an angle of 30 ± 15°. According to the prestored program for CTS, the instrument will automatically deliver 3 J/cm2 at an automatically measured therapy time. Each patient received 12 treatment sessions at a rate of two sessions/week.
Group (B), open carpal tunnel release surgery
Open surgical decompression was done by an incision that gently curves from the ulner border of the palmaris longus tendon where it crosses the distal wrist crease and extends to the midpalm. The palmer fascia was incised to expose the transverse carpal ligament, which was completely divided vertically at its midpoint. The median nerve was inspected, and neurolysis may be carried out if the nerve was found to be adherent. Finally, only the skin was closed.
-
1.
Before treatment evaluations
-
Patients’ data
These included age (mean values ± SD and range), sex, hand dominance, employment type, medical comorbidities, and smoking. Medical comorbidities included hypertension, diabetes mellitus, thyroid disease, cervical spine disease, and previous hand trauma. Prior treatment and its effectiveness were also reported.
-
Subjective complaints
These included the affected side and duration of symptoms, pain, tingling, numbness, awaking from sleep by symptoms, exacerbation of symptoms by manual effort, and muscle weakness.
-
Objective findings
These included hand and/or wrist scars, Tinel’s sign, Phalen’s sign, decreased light touch sensibility, positive median nerve compression test, and thenar atrophy. NCSs were finally carried out.
-
-
2.
After treatment evaluations
Symptomatic relief, return to light and regular duty, as well as complications including those related to the scars among group B were reported. Once more, NCSs were carried out at the end of the follow up about 6 months after accomplishing the corresponding treatment. Statistical analysis was evaluated by a Pearson Correlation test. Statistical significance was set at p ≤ 0.05.
Results
-
1.
Before treatment
-
Patients’ data
The mean age for all patients was 47.23 ± 6.52 years (range, 31–67 years). It was 49.11 ± 7.23 years (range, 38–67 years) for group A and 42.65 ± 8.05 years (range, 31–63 years) for group B. None of our patients had experienced thyroid and cervical spine diseases as well as previous hand trauma. Table 1 summarizes the patients’ data of all the patients and for each group (A and B) separately.
Regarding the reported treatment modalities, splinting during work, at night, or all over the day was attempted in 15 patients (27.78%). NSAIDs were attempted in 11 patients (20.37%). None of the investigated patients had received prior local corticosteroid injection. All patients who had undergone previous nonoperative treatment had either no improvement or minimal improvement of complaints. Moreover, two patients (3.70%) reported prior open carpal tunnel release on their dominating right side. Their presentations at the present study were for the symptomatic contralateral nondominating left side.
-
Subjective complaints
Forty-five patients (83.33%) had complaints on their right hands and three patients (5.56%) on their left hands. Bilateral symptoms were found in the resting six patients (11.11%). All of those bilaterally affected patients experienced greater symptoms on their dominating right hands. Bilateral procedures were accomplished in six patients (11.11%), on the left side in three patients (5.56%) and on the right side for the resting 45 patients (83.33%). The duration of the presenting symptoms was 32.45 ± 6.12 months (range, 3–120 months). The duration of symptoms among group A was 28.21 ± 7.03 months (range, 6–84 months) and 36.17 ± 4.38 months (range, 3–120 months) among group B. Table 2 shows the subjective complaints on the initial patients’ presentations for all patients and for each group (A and B) separately.
-
Objective findings
All patients underwent an initial physical examination during their first visit after an assessment of their subjective complaints. Scars were noticed on right hands of two patients (3.70%) of previous open carpal tunnel release. Table 3 shows the objective findings for all patients and for each group (A and B) separately.
-
Nerve conduction studies
All patients underwent pretreatment NCSs. Positive NCSs were elicited in 48 affected hands (80%). The resting 12 symptomatic hands (20%) had negative results despite the physical findings consistent with the diagnosis of CTS, and yet, they were included on a clinical basis. Table 3 shows NCSs’ results for all patients and for each group (A and B) separately.
-
-
2.
After treatment
All patients were reevaluated for 6 months after accomplishing the corresponding treatment on monthly based visits. Regarding group A, there were no restrictions neither towards return to work with one-handed duty nor towards return to light duty work. On the contrary, among group B, patients were allowed to return to work with one-handed duty restrictions about 2–3 days after surgery, and after 3 weeks, return to light duty work started. However, regular duty work was accomplished after 6 weeks for both groups after the end of the corresponding treatment. The subjective complaints for both groups were collectively summarized in Table 4. The objective findings including NCSs results for both groups were collectively summarized in Table 5.
Discussion
CTS is an entrapment neuropathy of the median nerve at the wrist. It is one of the most common peripheral nerve disorders. The cause of idiopathic CTS remains unclear. Diagnosis of CTS is still mainly clinical. Open carpal tunnel release is considered the standard treatment modality. However, with the progressive achievements in the field of LLLT, it may get a role for the treatment of CTS, which was the motive for making us investigate toward this field.
Regarding the patients’ data at the present study, female/male ratio was found to be 8/1. The majority of our patients were manually employed. Regarding the correlation between hand dominance and the symptomatic side, the findings of the present study are greatly acceptable with what were frequently reported [1, 2, 4, 8]. The majority of the presenting symptoms in the present study were related to the dominating side. All of the six bilaterally affected patients had experienced greater symptoms on their dominating right hands. Forty-five unilaterally symptomatic patients were on their dominating right hands. The resting three patients were unilaterally symptomatic on the left side from which one patient had left-handed dominance, whereas the other two patients were, after prior surgical release, on their contralateral dominating right side.
Regarding the evaluation of the success of each of the treatment modality, it is important to temper results for each group by its corresponding pretreatment assessment. Although our patients exhibited variable statistically significant results, there was a uniformly high patients’ satisfaction regardless the treatment modality.
Regarding the subjective complaints, almost all our patients had satisfactory outcome at different statistical significance. The only exception reported was regarding muscle weakness. Fortunately, the majority of our patients presented with pain, tingling, and numbness. This was not a surprise as it was frequently reported in previous studies [11, 15]. Moreover, regarding the objective findings including NCSs, almost all our patients had satisfactory results at different statistical significance. The only exception found was regarding thenar atrophy.
The nonsignificant results of the present study regarding muscle weakness and thenar atrophy for patients among group B are the same as for what was previously reported. It was reported that patients with more advanced CTS presenting with muscle weakness and thenar atrophy were associated with less favorable surgical outcomes [7, 17, 18]. The application of this statement also for our results among group A cites a rule that patients with advanced CTS must be cautioned to expect a longer and possibly incomplete neurological recovery regardless of the treatment modality.
It was reported that NCSs have a lower sensitivity result when compared to the clinical diagnosis as 22% of clinically definite CTS patients had normal NCSs [3, 16, 20]. Accordingly, 12 affected hands (20%) in the present study with NCSs findings were included and treated on a clinical basis.
Residual and/or recurrent symptoms after carpal tunnel release may result from the incomplete release of the transverse carpal ligament, fibrous proliferation, scarring within the tunnel, entrapped palmer cutaneous nerve, and painful scar [17]. On the other hand, unrelieved or recurrent symptoms after LLLT may be due to an incomplete control of CTS pain [11]. In the present study, there were three hands (10%) and only one hand (3.33%) among groups A and B, respectively, who experienced residual and/or recurrent symptoms after treatment. The residual and/or recurrent symptoms among group B were not only less frequent than those among group A, but also they were transient, occasional, and markedly attenuated. This was denoted by the disappearance of night awakening and symptom exacerbation among group B rather than among group A.
Finally, the existing controversy regarding the safety of the open approach for carpal tunnel release was noticed to be a personally dependent. Fortunately, the scar-related complications among group B were the only complications. Occasional scar tenderness was reported in three hands (10%), and scar hypersensitivity to touch, cold, and/or heat was reported in only one hand (3.33%).
Conclusion
LLLT has proven to be an effective and noninvasive treatment for early and mild-to-moderate cases of CTS when pain is the main presenting symptom, whereas surgery could be preserved for advanced and chronic cases. Moreover, LLLT may be suggested for treatment of residual pain after surgically released carpal canal.
Refinement of laser tools and introduction of other wavelengths could make LLLT for CTS a field for further investigations. Since then, carpal tunnel release is still the standard treatment for CTS taking into consideration that its complications may be overcome by the introduction of endoscopic approach that should be addressed for further evaluation.
References
Ahn DS, Yoon ES, Koo SH, Park SH (2000) A prospective study of the anatomic variations of the median nerve in the carpal tunnel in Asians. Ann Plast Surg 44:282–287
Bland JDB (2000) The value of the history in the diagnosis of carpal tunnel syndrome. J Hand Surg 25B:445–450
Bland JDB (2001) Do nerve conduction studies predict the outcome of carpal tunnel decompression? Muscle Nerve 24:935–940
Bland JDB (2005) Carpal tunnel syndrome. Curr Opin Intern Med 4(6):578–582
Boz C, Ozmenoglu M, Altunayoglu V (2004) Individual risk factors for carpal tunnel syndrome: an evaluation of body mass index, wrist index and hand anthropometric measurements. Clin Neurol Neurosurg 106:294–299
El Miedany YM, Aty SA, Ashour S (2004) Ultrasonography versus nerve conduction study in patients with carpal tunnel syndrome: substantive or complementary tests? Rheumatology (Oxford) 43:887–895
Ettema AM, Amadio PC, Cha SS, Harrington JR, Harris AM, Offord KP (2006) Surgery versus conservative therapy in carpal tunnel syndrome in people aged 70 years and older. Past Reconstr Surg 118(4):947–958
Geoghegan JM, Clark DI, Bainbridge LC (2004) Risk factors in carpal tunnel syndrome. J Hand Surg 29B:315–320
Hirata H, Nagakura T, Tsujii M (2004) The relationship of VEGF and PGE2 expression to extracellular matrix remodeling of the tenosynovium in the carpal tunnel syndrome. J Pathol 204:605–612
Hirata H, Tsujii M, Yoshida T (2005) MMP-2 expression is associated with rapidly proliferative arteriosclerosis in the flexor tenosynovium and pain severity in carpal tunnel syndrome. J Pathol 205:443–450
Irvine J, Chong SL, Amirjani N, Chan KM (2004) Double-blind randomized controlled trial of low-level laser therapy in carpal tunnel syndrome. Muscle Nerve 30:182–187
Kamolz LP, Beck H, Haslik W (2004) Carpal tunnel syndrome: a question of hand and wrist configurations? J Hand Surg 29B:321–324
Kujawa J, Zavodnik L, Zavodnik I, Bryszewska M (2003) Low intensity near infrared laser radiation induces changes of acetylcholine esterase activity of human erythrocytes. Lasers Surg Med 21(6):351–355
Matson E, Perira AN, Eduardo P, Marques MM (2002) Effect of low power laser irradiation on cell growth and procollagen synthesis in cultured fibroblasts. Lasers Surg Med 31(4):263–267
Naeser MA, Kyumg AEK, Hahn MD, Lieberman BE, Kenneth F, Branco MA (2002) Carpal tunnel syndrome pain treated with low level laser and microamperes transcutaneous electric nerve stimulation. Arch Phys Med Rehabil 83:978–988
Nora DB, Becker J, Ehler JA, Gomes I (2004) Clinical feature of 1,039 patients with neurophysiological diagnosis of carpal tunnel syndrome. Clin Neurol Neurosurg 107:64–69
Rodner CM, Katarincic J (2006) Open carpal tunnel release. Tech Orthop 21(1):3–11
Schmelzer RE, Rocca GJD, Caplin DA (2006) Endoscopic carpal tunnel release: a review of 753 cases in 486 patients. Plast Reconstr Surg 117(1):177–185
Scholten RJPM, de Krom MCTFM, Bertelsmann FW, Bouter LM (1997) Variation in the treatment of carpal tunnel syndrome (Letter). Muscle Nerve 20:1334–1335
Witt JC, Hentz JG, Stevens JC (2004) Carpal tunnel syndrome with normal nerve conduction studies. Muscle Nerve 29:515–522
Acknowledgment
The authors thank Mrs. Reham Shahin for her effort during the primary conduction of LLLT for CTS. Finally, we express our appreciation for the staff of the Clinical Neurophysiology unit, Cairo University, for their cooperation during NCSs.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Elwakil, T.F., Elazzazi, A. & Shokeir, H. Treatment of carpal tunnel syndrome by low-level laser versus open carpal tunnel release. Lasers Med Sci 22, 265–270 (2007). https://doi.org/10.1007/s10103-007-0448-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-007-0448-8