Abstract
Acupuncture using laser needles is a new totally painless stimulation method which has been described for the first time. This paper presents an experimental double-blind study in acupuncture research in healthy volunteers using a new optical stimulation method. We investigated 18 healthy volunteers (mean age±SD: 25.4±4.3 years; range: 21–30 years; 11 female, 7 male) in a randomized controlled cross-over trial using functional multidirectional transcranial ultrasound Doppler sonography (fTCD; n=17) and performed functional magnetic resonance imaging (fMRI) in one volunteer. Stimulation of vision-related acupoints resulted in an increase of mean blood flow velocity in the posterior cerebral artery measured by fTCD [before stimulation (mean±SE): 42.2±2.5; during stimulation: 44.2±2.6; after stimulation: 42.3±2.4 cm/s, n.s.]. Mean blood flow velocity in the middle cerebral artery decreased insignificantly. Significant changes (p<0.05) of brain activity were demonstrated in the occipital and frontal gyrus by fMRI. Optical stimulation using properly adjusted laser needles has the advantage that the stimulation cannot be felt by the patient (painless and no tactile stimulation) and the operator may also be unaware of whether the stimulation system is active. Therefore true double-blind studies in acupuncture research can be performed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
A new noninvasive laser needle system has been developed and used for the first time in acupuncture research [1, 2]. This new optical stimulation technique has the advantage that the stimulation is absolutely painless. Moreover laser needle acupuncture allows us to stimulate appropriate acupoint combinations simultaneously and with higher radiation doses than is possible with commercially available low-level hand held laser equipment.
The laser radiation of eight laser diodes is coupled into eight optical fibers and the laser needles are arranged at the distal ends of the optical fibers. Due to the direct contact between the laser needles and the skin, no loss of intensity occurs and the laser power which affects the acupoints can be determined exactly [1, 2].
The aim of this study was to provide evidence of specific effects of laser needle acupuncture by stimulating a combination of vision-related acupoints of traditional Chinese medicine. Quantification of cerebral effects of stimulation was performed using functional multidirectional transcranial Doppler sonography (fTCD) in a randomized controlled double-blind cross-over study design. We also performed functional magnetic resonance imaging (fMRI) measurements in one volunteer using a block design.
The dynamics of the metabolic mechanism that regulates cerebral blood flow has already been studied in normal human subjects using fTCD [3, 4]. Blood flow velocity in the posterior cerebral artery (PCA), supplying the visual cortex, increased by 16.4% in response to light stimulation of the retina.
The method of fTCD has also been used in previous studies in acupuncture and laser needle research to investigate specific changes in blood flow velocities of different cerebral arteries [1]. Functional magnetic resonance is sensitive to subtle regional changes in the blood oxygenation level from increased neuronal activity during a specific task or stimulation. It has been successfully used to map the sites of brain activations during needle and low-level laser acupuncture [5, 6, 7, 8, 9]. These studies report increase (positive activation) and decrease (negative activation) of the blood oxygenation level dependent (BOLD) signal. However, fMRI has not been used up to now during laser needle stimulation.
Materials and methods
Painless laser needles
For our experiments eight acupuncture points were chosen and irradiated simultaneously. The laser needles used in this study emit red light in cw-mode with an output power of 30–40 mW per laser needle (wavelength: 685 nm). The fiber core diameter used in this study was about 500 μm. The time of irradiation was 20 min (fTCD measurements) resulting in an energy density of about 4.6 kJ/cm2 at each acupoint and a total sum of 36.8 kJ/cm2 for all acupoints. The laser needles were fixed onto the skin using plaster stripes but were not pricked into the skin.
Functional multidirectional transcranial Doppler sonography
Transtemporal Doppler sonographic examinations of the PCA and the middle cerebral artery (MCA) were performed simultaneously and continuously to determine alterations of cerebral blood flow velocities [4]. A Multi-Dop T unit (DWL Electronic Systems, Sipplingen, Germany) including two 2 MHz probes were used in a multidirectional ultrasound probe holder construction. Under acoustic control, the angle and position of the probes were adjusted until the greatest possible signal amplitude was reached. Alterations in the blood flow velocities of both arteries were registered continuously and simultaneously. In addition blood pressure was measured noninvasively before and after stimulation (Cardiocap CC-104, Datex, Hoevelaken, The Netherlands).
Functional magnetic resonance imaging
Functional magnetic resonance imaging was performed using a 1.5 Tesla whole body system (Intera, Philips Medical Systems, Best, the Netherlands). Functional images sensitive to blood oxygen dependent contrast were acquired with a T2* weighted gradient echo with single shot echo planar readout (flip angle 90°, TE 50 ms, FOV 250 mm, matrix 96×96 interpolated to 128×128). Thirty axial slices with a slice thickness of 4 mm were imaged. A total of 144 volume images were obtained continuously with a repetition time of 5 s per volume.
Participants
We investigated 18 healthy volunteers (mean age±SD: 25.4±4.3 years; range: 21–30 years; 11 female, 7 male) using fTCD (n=17) and one volunteer using fMRI (27 years, female). The study protocol was approved by the institutional ethics committee of the University of Graz (11-017ex00/01) and all 18 participants gave written informed consent. None of the subjects were under the influence of centrally active medication. All persons were free of neurological or psychological disorders including the absence of visual deficits. An honorarium was given for participation.
Experimental design and procedure
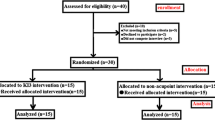
Eight vision-related distal acupoints [6, 7, 10] on both sides and eight placebo points were tested using two schemes (fTCD measurements), each in one session in a randomized controlled double-blind cross-over study design (Fig. 1). The same acupoints were used for the fMRI investigation. The acupuncture scheme was selected by an expert in traditional Chinese medicine. In addition we have seen in several test measurements that needle stimulation of this acupuncture scheme led to alterations of blood flow velocity in the PCA.
The acupoints were cleaned with alcohol. Then the laser needles were put in contact with the skin and fixed by plaster stripes. During the experiments the subjects were in a relaxed and comfortable position on a bed in our laboratory (fTCD measurements) or lying in the scanner (fMRI investigation). For the fTCD investigations we started randomly with either acupoint or placebo stimulation.
Acupoints
Hegu (LI 4)
Location: on the dorsum of the hand, between the first and second metacarpal bones, in the middle of the second metacarpal bone on the radial side. Indications: headache, redness, swelling and pain of the eye.
Zusanli (S 36)
Location: 3 cun below Dubi (S 35), one finger-breadth from the anterior crest of the tibia. Indications: gastric pain, abdominal distension, vomiting, diarrhea, dysentery, has tonification effect.
Kunlun (B 60)
Location: in the depression between the tip of the external malleolus and tendo calcaneus. Indications: headache, neck rigidity, dizziness.
Zhiyin (B 67)
Location: on the lateral side of the small toe, about 0.1 cun lateral to the corner of the nail. Indications: headache, pain in the eye, nasal obstruction, epistaxis, malposition of fetus.
Evaluated parameters
The mean blood flow velocity (vm) in the PCA and the MCA were evaluated simultaneously and continuously at different measurement points (a–e in Fig. 2a) [10]. Each person was studied while performing stimulation on vision-related acupoints and placebo points. The interval between the fTCD experiments was 20–30 min and the subjects were instructed to keep their eyes closed during the whole fTCD experiment.
Similarly, during fMRI investigations the subject could not see whether the laser was off or on. The fMRI study used a block design with alternating 1 min resting condition (‘R’) and 1 min activation condition (‘A’) (Fig. 2b). The experiment started with ‘R’ followed by the laser needle acupuncture condition (‘A’). A total of six ‘R’ and six ‘A’ intervals were registered. Altogether the fMRI data acquisition took 12 min.
Statistical analysis
The fTCD data before (a), during (b–d), and after (e) laser needle acupuncture (Fig. 2a) were tested with Kruskal–Wallis one-way ANOVA on ranks (SigmaStat, Jandel Scientific, Erkrath, Germany). The criterion for significance was p<0.05.
The fMRI data were analysed using SPM 99 (SPM 99, Wellcome Department of Imaging Neuroscience, London, UK). All volumes from the subject were realigned using the first volume as a reference and resliced using sinc-interpolation. The functional images were spatially normalized to a standard echo-planar template in Talairach space.
Functional data were spatially smoothed with a 6 mm full-width (at half maximum) isotropic kernel. A boxcar waveform convolved with a synthetic haemodynamic response function was used as the reference waveform. A t-test was performed to identify regions showing significantly higher activation during the activation condition versus the resting condition. For significantly activated regions, a statistical threshold p<0.05, corrected at the cluster level for multiple comparisons, was used.
Results
The results of the alterations of mean blood flow velocities in the PCA and MCA before, during, and after laser needle and placebo acupuncture are summarized in figure 3.
Mean blood flow velocity (vm) of the posterior cerebral artery (PCA) and the middle cerebral artery (MCA) before (a), during (b–d), and after (e) stimulating vision-related acupoints (A) and placebo points (B) with laser needles in 17 healthy volunteers. Note the trend towards an increase (+2.5 cm/s) in vm in the PCA during acupoint stimulation
The results showed a trend towards an increase of vm (insignificant changes) in the PCA during (b–d) laser needle acupuncture at vision-related acupoints (Fig. 3A, upper panel). At the same time only minor changes in vm were seen in the MCA (Fig. 3A, lower panel). The maximum amplitude of vm in the PCA was detected with a delay of 20–60 s after the initial stimulus by the laser needles [mean±SE, acupoint stimulation, PCA: 42.2±2.5 before (a), 44.2±2.6 during (b–d), 42.3±2.4 cm/s after (e)]. Stimulation at placebo points did not increase vm of the PCA and of the MCA (Fig. 3B); rather there was a trend towards a small decrease of mean values of the mean vm in both arteries [mean±SE, placebo point stimulation, PCA: 42.9±2.6 before (a), 41.7±2.6 during (b-d), 42.1±2.8 cm/s after (e)].
The mean arterial blood pressure before and after laser needle acupuncture was almost identical (76.7±7.6 SD vs. 75.8±6.8 mmHg). Significant changes in brain activation were found in the occipital lobe and in the frontal lobe (Figs. 4, 5) (Table 1).
Discussion
Recent scientific and technological progress especially regarding the application of modern brain function monitoring systems has truly revolutionized acupuncture. The usage of advanced exploratory tools such as fTCD or fMRI provides insights and attempts to shine scientific light upon the most spectacular of the eastern medical procedures [3, 4]. Recently it has attracted interest that the brain is the key to acupuncture’s and laser puncture’s effects. New experimental constructions to measure ultrasound, light and bioelectrical processes can reproducibly demonstrate effects of stimulation of acupoints in the brain [1, 2, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21].
The new laser needle system has been described for the first time in scientific literature within this journal [1]. In addition, previous studies from our group show that the new optical stimulation with laser needles can elicit reproducible cerebral effects which are in the same order with respect to the maximum amplitude of the mean blood flow velocity as compared to needle acupuncture [1]. The stimulation performed within this study could not be felt by the patient. The operator was also unaware of whether the stimulation was active, and therefore a true double-blind study was performed. Moreover, at the moment there is no other laser system commercially available that could be used at eight or more standard acupuncture points simultaneously.
The effectiveness of unconventional complementary medical methods, such as laser puncture, has previously been documented mainly as single cases. There are many theoretical and clinical studies concerning laser puncture in scientific literature [1]. To our knowledge, laser acupuncture has not been studied in cases where more than one acupoint at a time was stimulated. In our experiment, we tested four acupoints (four on each side of the body) with laser needle acupuncture, and measured the alterations of brain activations using fTCD and fMRI.
In this study, we were not able to separate significant specific cerebral effects of blood flow velocity during laser needleacupuncture using fTCD. However, there was a trend of an increase in vm during laser needle stimulation of visual acupoints in the PCA. Similar significant effects have been reported after manual needle acupuncture [11, 13, 14, 15, 16]. Previous results also show that different modes of manual acupuncture stimulation differentially modulate cerebral blood flow velocity [20].
In addition to fTCD we used for the first time fMRI in a healthy volunteer during laser needle stimulation of the same vision-related acupoints as used for the fTCD measurements. Bilateral stimulation of the acupoints produced bilateral positive activation over the frontal cortex. A time-logged increase of the BOLD signal was also seen at the left superior occipital gyrus (Brodmann area 19). Apparently the stimulation of vision-implicated acupoints (Kunlun, Bladder 60 and Zhiyin, Bladder 67) activated the visual cortex. These findings are in accordance with other fMRI acupuncture studies. Cho et al. [7] reported that needling of acupoints (Bladder 60, 65, 66 and 67) on the foot created activation in the visual cortex similar to actual visual stimuli. Needling of non-acupoints on the foot 2–5 cm away from the vision-related acupoints as control caused no activation in the occipital lobes [7].
In traditional needle acupuncture, treatment points are located at different depths and hence needle insertion is different. This is of particular importance with the points we selected because Zhiyin requires a very shallow needle insertion relative to Zusanli. With the laser needle stimulation the acupoints will receive different energy doses because of their different depths. It is possible that the effects seen with fTCD and fMRI could be due to stimulation of one of the points. Further investigation on this topic is necessary.
Li et al. [6] recently found that the application of conventional or electro-acupuncture over four vision-implicated acupoints on the right foot can modulate the activity of specific brain sites. Negative and positive activations were seen using fMRI during conventional acupuncture while positive activations, similar to our results of laser needle stimulation, only were observed during optical stimulation and electro-acupuncture. The authors also found bilateral activations in frontal cortices [6].
It has been demonstrated using fMRI that needle acupuncture [7] and laser puncture [9] of the vision-related acupoint Zhiyin (Bladder 67) activates the visual cortex of the human brain. As a further study on the effect of this acupoint stimulation on the visual cortex, Lee et al. [22] examined c-Fos expression in binocularly deprived rat pups. Interestingly, acupuncture stimulation of Bladder 67 resulted in a significant increase in the number of c-Fos-positive cells in the primary visual cortex, while acupuncture stimulation of other points are less important for visual function and had no significant effect on c-Fos expression in the primary cortex.
Other studies have shown effects of acupuncture needle manipulation of Large Intestine 4 [we also used this acupoint (Hegu) in our scheme as a general point of activation] on a network of cortical and subcortical limbic and paralimbic structures [5]. We did not find the same significant effects in our fMRI experiment. In this context it is important to mention that laser needle acupuncture allows, for the first time, totally painless acupuncture stimulation. Therefore, the differences between needle acupuncture which always includes pain stimulation, and a painless acupuncture stimulation technique can be examined.
Conclusion
Using the new laser needle acupuncture method we were able to stimulate multiple vision-associated acupuncture points at the same time. The results showed insignificant increases in cerebral blood flow velocity of the PCA after stimulation of vision-related acupoints on the foot. At the same time blood flow velocity in the MCA showed minor changes. Stimulation at placebo points did not show increases in blood flow velocity in both arteries. The fMRI results of a healthy volunteer after laser needle stimulation of the same acupoints showed significant changes in occipital and frontal brain areas. Both techniques, fTCD and fMRI, can be used to study cerebral effects of laser needle acupuncture in a complementary way.
References
Litscher G, Schikora D (2002) Cerebral vascular effects of non-invasive laserneedles measured by transorbital and transtemporal Doppler sonography. Lasers Med Sci 17:289–295
Litscher G, Schikora D (2002) Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture. Spectroscopy 16:335–342
Aaslid R (1987) Visually evoked dynamic blood flow response of the human cerebral circulation. Stroke 18(4):771–775
Sturzenegger M, Newell DW, Aaslid R (1996) Visually evoked blood flow response assessed by simultaneous two-channel transcranial Doppler using flow velocity averaging. Stroke 27(12):2256–2261
Hui KKS, Liu J, Makris N, Gollub RL, Chen AJW, Moore CI, Kennedy DN, Rosen BR, Kwong KK (2000) Acupuncture modulates the limbic system and subcortical gray structures of the human brain: evidence from fMRI studies in normal subjects. Hum Brain Map 9:13–25
Li G, Cheung RTF, Ma QY, Yang ES (2003) Visual cortical activations on fMRI upon stimulation of the vision-implicated acupoints. Neuroreport 14:669–673
Cho ZH, Chung SC, Jones JP, Park JB, Park HJ, Lee HJ, Wong EK, Min BI (1998) New findings of the correlation between acupoints and corresponding brain cortices using functional MRI. Proc Natl Acad Sci USA 95:2670–2673
Cho ZH, Oleson TD, Alimi D, Niemtzow RC (2002) Acupuncture: the search for biologic evidence with functional magnetic resonance imaging and positron emission tomography techniques. J Altern Compl Med 8:399–401
Siedentopf CM, Golaszewski SM, Mottaghy FM, Ruff CC, Felber S, Schlager A (2002) Functional magnetic resonance imaging detects activation of the visual association cortex during laser acupuncture of the foot in humans. Neurosci Lett 327:53–56
Litscher G, Schikora D (2002) Effects of new noninvasive laserneedles on brain function. Proceedings of the International Federation for Medical and Biological Engineering 2:996–997
Litscher G (2002) Computer-based quantification of traditional Chinese-, ear- and Korean hand acupuncture: needle-induced changes of regional cerebral blood flow velocity. Neurol Res 24:377–380
Litscher G, Wang L, Wiesner-Zechmeister M (2000) Specific effects of laserpuncture on the cerebral circulation. Lasers Med Sci 15:57–62
Litscher G (2001) High-Tech Akupunktur. Pabst, Lengerich
Litscher G, Wang L, Yang NH, Schwarz G (1999) Computer-controlled acupuncture. Quantification and separation of specific effects. Neurol Res 21(6):530–534
Litscher G, Wang L, Yang NH, Schwarz G (1999) Ultrasound-monitored effects of acupuncture on brain and eye. Neurol Res 21(4):373–377
Litscher G, Yang NH, Schwarz G, Wang L (1999) Computer-controlled acupuncture. A new construction for simultaneous measurement of blood flow velocity of the supratrochlear and middle cerebral arteries. Biomed Techn 44(3):58–63
Litscher G, Schwarz G, Sandner-Kiesling A, Hadolt I (1998) Robotic transcranial Doppler sonography probes and acupuncture. Int J Neurosci 95(1–2):1–15
Litscher G, Schwarz G, Sandner-Kiesling A, Hadolt I, Eger E (1998) Effects of acupuncture on the oxygenation of cerebral tissue. Neurol Res Suppl 1:28–32
Litscher G, Wang L (2000) Cerebral near infrared spectroscopy and acupuncture - results of a pilot study. Biomed Technik 45(7–8):215–218
Bäcker M, Hammes MG, Valet M, Deppe M, Conrad B, Tölle TR, Dobos (2002) Different modes of manual acupuncture stimulation differentially modulate cerebral blood flow velocity, arterial blood pressure and heart rate in human subjects. Neurosci Lett 333:203–206
Litscher G (2003) Cerebral and peripheral effects of laserneedle-stimulation. Neurol Res 25:722–728
Lee H, Park HJ, Kim SA, Lee HJ, Kim MJ, Kim CJ, Chung JH, Lee H (2002) Acupuncture stimulation of the vision-related acupoint (Bl-67) increases c-Fos expression in the visual cortex of binocularly deprived rat pups. Am J Chin Med 30:379–385
Acknowledgements
The authors thank Eva Maria Huber (Department of Biomedical Engineering and Research in Anesthesia and Critical Care, Medical University of Graz, Austria), Martin Kronbichler (Department of Psychology, University of Salzburg, Austria) for supporting this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Litscher, G., Rachbauer, D., Ropele, S. et al. Acupuncture using laser needles modulates brain function: first evidence from functional transcranial Doppler sonography and functional magnetic resonance imaging. Lasers Med Sci 19, 6–11 (2004). https://doi.org/10.1007/s10103-004-0291-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-004-0291-0