Abstract
Blastocystis sp. is the most common intestinal parasite isolated in humans. The aim of the study was to describe the risk factors associated to Blastocystis sp. detection. A case-control retrospective study was carried out at Vall d’Hebron University Hospital (Barcelona, Spain), which receives all fecal samples collected in Barcelona at primary care level. Eligible patients were patients older than 18 years in whom three consecutive stool samples were examined for parasitic diagnosis from January to December 2017. Positive patients for Blastocystis sp. were assigned as cases whereas negative patients were assigned as controls. Overall, 4174 patients were eligible for the study, from whom 724 (17.3%) had Blastocystis sp. detection. From these, 170 cases (Blastocystis sp. positive) and 170 controls (Blastocystis sp. negative) were randomly selected for inclusion. One hundred and twenty-six (37.1%) of them were immigrants, and 171 (50.3%) patients had traveled out of Spain the year before. The majority of individuals had jobs with no direct contact with other people (health personnel, teachers, and caregivers) (85.6%), and 29.4% were in usual contact with animals. Regarding clinical information, 68.2% of patients presented digestive symptoms, 3.5% presented an immunosuppressant condition, and 6.5% were infected by other intestinal parasites. Variables associated to Blastocystis sp. detection were being born in Africa, having traveled abroad, and working in direct contact with other people. Having other intestinal parasitic infections had a protective value. Our study provides new insights into the epidemiology of Blastocystis sp. in industrialized countries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Blastocystis sp. is the most common intestinal parasite isolated in humans, with up to one billion humans colonized [1,2,3]. Transmission can occur from human to human, human to animal, or animal to human [4]. Recent studies based on the comparison of the nuclear small subunit rRNA gene show that Blastocystis has an extensive molecular diversity, with up to 17 genetic distinct ribosomal lineages described [5].
Blastocystis sp. distribution around the world is not homogeneous, as prevalence can vary from up to 10% in developed countries to 50–60% in developing countries [6]. The highest prevalence ever observed was seen in Senegal, in the year 2014 [7]. Moreover, differences in subtype distribution have been observed regarding geographic distribution [8]. This large variance may be due to misreporting and misdetection in some clinical laboratories, which suggests that prevalence may be higher than recorded in some studies [9]. The high prevalence in developing countries is usually related to poor hygiene practices and to consumption of contaminated food or water [10]. In addition, recent studies have also strongly related its distribution to the socioeconomic and geographic situation. However, developed countries also show high prevalence rates of detection. Animals have been suggested as the sources of infection since genetic similarity has been demonstrated [11]. Immigrants, travelers, and people who live in close contact with animals are also susceptible to be detected with Blastocystis sp.
Nowadays, there is a growing recognition about Blastocystis sp. pathogenic potential, although its virulence mechanisms are not fully understood [1]. However, no consensus has been reached yet, and many authors still put doubt on the Blastocystis sp. role in human disease, making its real human health impact uncertain [12, 13]. Even so, it is accepted to be a potential pathogen for immunocompromised people.
Transmission is mostly accepted to happen fecal-orally both by direct or indirect ways, like contact with infected people or animals or through the ingestion of contaminated water, respectively [14]. Foodborne transmission has also been reported as a source of infection. However and even if detected in asymptomatic patients, it is thought to cause gastrointestinal symptoms including diarrhea, abdominal pain, flatulence, dyspepsia, or vomiting [8]. Moreover, cutaneous manifestations such as chronic urticaria have been reported and have been associated to blastocystosis, especially in patients with irritable bowel syndrome (IBS) [15,16,17].
Despite its prevalence and all consequences associated to Blastocystis sp. infection, current knowledge about this organism in Spain is scarce. However, Blastocystis sp. zoonotic transmission risk has been recently studied for individuals in the Basque Country [18] and for HIV-positive children in Madrid [19].
Therefore, the main objective of the present study was to determine the risk factors associated to Blastocystis sp. detection in symptomatic and asymptomatic patients in Barcelona, Spain.
Methods
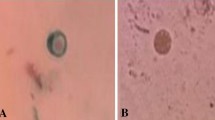
A retrospective case and control study was performed at the Vall d’Hebron University Hospital, a tertiary hospital included in the International Health Program of the Catalan Health Institute (PROSICS, Barcelona, Spain). The hospital receives all stool samples collected in Barcelona at primary care level. After consulting the Microbiology Department registry, 34,158 stool samples were registered at the hospital database from January to December 2017. Eligible patients were those older than 18 years old in whom three consecutive stool samples had been examined for parasitic diagnostic for any reason (gastrointestinal symptoms, eosinophilia, and screening of asymptomatic carriers) and those who had not received any previous treatment. Only patients with three stool samples were selected because of an agreement with earlier studies that state the need for multiple stool examinations with microscopy before reporting a negative result for Blastocystis sp. [20]. A total of 12,522 samples fulfilled the inclusion criteria, which corresponds to 4174 patients. From this, 724 (17.3%) were infected with Blastocystis sp. (see Fig. 1). During the study period, the diagnosis of intestinal parasites, including Blastocystis sp., was performed by microscopic examination of concentrated stool samples using a commercial dispositive (Midi Parasep SF, APACOR, England).
To calculate the sample size for a case-control study, a proportion of 50% of cases exposed to risk factors of Blastocystis sp. detection was selected, whereas a proportion of 35% was selected for controls. The ratio among cases (at least one positive stool examination for Blastocystis sp.) and controls (all three stool samples negative for Blastocystis sp.) was 1:1; the power of the study was established at 80% with a confidence level of 95%. With the previous data, a sample size of 170 cases and 170 controls was obtained, which were randomly selected from the 4174 included participants.
Based on reviews of the literature on intestinal parasitic infections, we developed a standardized questionnaire to determine the demographic and clinical characteristics of patients, in order to be able to later assess the correlation between the questionnaire’s answers and potential detection risk factors (Supplementary material) [13, 15,16,17, 21]. It included questions regarding date of inclusion, age, sex, origin, type of work, type of environment, travels, regular contact with animals, and gastrointestinal symptoms. Jobs were subdivided into two categories, depending on the presence of direct contact with other people or not. Hospital personnel, teachers, restaurant workers, and caregivers were included in the first group. The questionnaire also included questions about clinical issues such as number of positive stools, diabetes mellitus, immunosuppression, and coinfection with other parasites, which were obtained by looking at the medical record of patients. All questions were asked related to the moment of the stool sampling. As it has been demonstrated that Blastocystis sp. can persist for months and colonize the gut [22], questions referring to previous travels took into account those done from 2016 until when stool sampling was done.
Eligible patients were contacted by telephone, and after a brief description of our research, they gave their oral consent to participate in the project. Contact telephones were obtained from the electronic medical record at our institution. The study protocol was reviewed and approved by the Ethics Committee of the Vall d’Hebron University Hospital (reference number PR (AG) 99/2018).
IBM SPSS software platform version 15 was used to perform the statistical analysis. Categorical data were presented as absolute numbers and proportions, and continuous variables were expressed as means and standard deviations (SD) or medians and interquartile ranges (IQR) depending on the distribution. The Kolmogorov-Smirnov test was used to evaluate the normal distribution of variables. Intergroup differences for continuous parameters were assessed by the Mann-Whitney U test if they did not present a normal distribution. The χ2 test or the Fisher exact test, when appropriate, was used to compare the distribution of categorical variables. Multivariate logistic regression analysis was made to identify factors associated to Blastocystis sp. detection. Variables were entered in the model if p < 0.20 on univariate analysis. Results were considered statistically significant if the two-tailed p value was < 0.05.
Results
The epidemiological characteristics of patients are summarized in Table 1. A total of 340 individuals aged 18 to 88 were interviewed in this study with an overall mean age of 46.7 ± 18.24 years, and most of them were females (60.6%). The majority of the participants lived in Barcelona city (95.9%), whereas the rest lived mainly in the surrounding areas. One hundred and twenty-six (37.1%) of participants were immigrants and had been living in Spain for 11 years on average. Among them, the majority of immigrants came from America, encompassing 69 (54.8% among immigrants) patients. Specifically, 54 (15.9%) came from South America, 14 (4.1%) from Central America, and 1 (0.3%) from North America. Twenty-four (7.1%) immigrants came from Asiatic countries and 16 (6.9%) from European countries. Finally, 17 (5%) patients came from Africa.
Most of the people did not have direct contact with people at work (n = 291, 85.6%). Only four (1.2%) people were in contact with the rural environment (villages with less than 10,000 inhabitants). Regarding daily life, 100 (29.4%) patients were in usual contact with animals, 70 (20.6%) of them with dogs and 28 (8.2%) with cats. Other pets included birds (n = 6, 1.8%), rabbits (n = 7, 2.1%), turtles (n = 2, 0.6%), fishes (n = 1, 0.3%), hamsters (n = 3, 0.3%), and chickens (n = 3, 0.3%). In addition, 171 (50.3%) patients traveled abroad during the year before the stool sampling. The most visited continent was Europe, with 66 (38.6% among all destinations) individuals, followed by 62 (18.9%) visitors to America and 34 (10%) to Asia.
Clinical characteristics of patients are summarized in Table 2. Most of the patients presented digestive symptoms (n = 232, 68.2%), and only 22 (6.5%) of participants were infected with other intestinal parasites, mainly Endolimax nana (n = 9, 2.6%) and Giardia lamblia (n = 6, 1.8%). Others included Dientamoeba fragilis (n = 4, 1.2%), Entamoeba coli (n = 3, 0.9%), Entamoeba histolytica/Entamoeba dispar (n = 3, 0.9%), Strongyloides stercoralis (n = 2, 0.6%), and Enterobius vermicularis (n = 1, 0.3%). Twenty-five (7.4%) patients were diabetic, and 12 (3.5%) presented an immunosuppressant condition; among these, most patients had HIV infection (n = 6, 1.8%). There were 14 (4.1%) patients with a diagnosis of irritable bowel syndrome.
After doing the multivariate analysis, the variables associated to Blastocystis sp. detection were coming from Africa (OR 5.216, p = 0.012), having traveled abroad (OR 1.932, p = 0.004), and working with the public (OR 2.654, p = 0.004). Moreover, being infected by other parasites resulted to be a protective factor (OR 0.370, p = 0.046).
Discussion
We retrospectively studied 340 patients, divided into cases and controls, whose stool samples were analyzed at the Vall d’Hebron University Hospital during year 2017. We used standardized questionnaires and medical records with the aim to gather information to detect risk factors related to Blastocystis sp. detection. Most of the samples belonged to Spanish women who lived in Barcelona and did not work directly with the public. Among all the variables studied, we found out being African, working with the public, and traveling to other countries significantly increase the risk of having a positive detection for Blastocystis sp. Moreover, being infected by other parasites was found out to be a protective factor. In addition, IBS patients had a lower Blastocystis carriage rather than non-IBS patients. However, no consensus has been reached for this fact, as there are studies which suggest correlation and studies which refuse it [23].
Throughout these lines, it has been stated that the public health burden of Blastocystis sp. is still underestimated, and so there is an interest in performing large-scale epidemiological surveys in industrialized countries. Parasitological studies in developed countries are not common. In Spain, studies regarding Blastocystis sp. detection are limited [15, 24, 25] and focused on specific population groups [26]. Up to date, only one molecular-based study has been conducted in asymptomatic population in Spain [18].
Regarding our study, only people from Africa were reported to have a stronger risk of detection. A higher incidence, however, not significant, was also seen among people coming from Central America. No differences were stablished regarding living in Spain.
A story of recent travel has been stated to be a risk factor to detect the parasite, with those in tropical and subtropical destinations being at increased risk [27]. Among all possible destinations, we found out Southern American and African countries had a higher risk of detection, even if it was not significant enough. It is interesting to point out that immigrants coming from Africa and people traveling to Africa are both at a higher risk to get infected. However, the latter is not statistically significant.
Age has sometimes been stated as a risk factor, usually describing children in developing countries as the most prevalent group [6]. Children were not included in our study, but, even if it was not statistically significant, younger adult age groups were at a higher risk, in accordance with a study conducted in France. However, the prevalence could be overestimated by fact that young people usually travel more [27].
Some studies have associated Blastocystis sp. detection to female gender [28], relating it to differences on the jobs but also to environmental, ecological, economical, and cultural factors [29]. In our case, women presented a higher prevalence of detection than men, but it was not statistically significant.
Contact with animals has been stated to be a risk factor for Blastocystis sp. detection [9, 30, 31] but not in our case. However, most of the studies which have proven this fact have been conducted in developing countries, where animal hygienic conditions and treatment may be different. In these studies, population is mostly rural and is in contact with livestock animals, whereas, in our case, dogs and cats were the main pets reported. A study performed in Spain suggested that dogs and cats do not play a relevant role as a natural source of human infections [17]. The fact that the present study was conducted by using samples which had been analyzed in Barcelona conditioned the origin of our samples, so most people came mostly from an urban environment. This finding makes it difficult to evaluate this variable and limits our study. Therefore, our results are based on an urban population, from an industrialized country.
We found out that people working with other people were at a higher risk than those who did not. The occupations that were taken into account (hospital personnel, caregivers, teachers, and restaurant workers) can be related to working with groups of people who are at a higher risk to be positive for Blastocystis sp., meaning that the risk of those surrounding them may also be increased. Therefore, not taking the adequate prevention may significantly increase the risk of having a positive isolate. Unfortunately, from all the participants, almost no one worked in contact with animals or in the rural (only two people did), so we cannot make any elucidation regarding this possible risk factor.
Blastocystis sp. pathogenicity has been one of the main controversial issues regarding this parasite. Even so, this was not a significant factor to consider in our study. Curiously, the same number of participants among cases and controls reported presence of digestive symptoms. However, some studies suggest that pathogenicity may be related to different Blastocystis sp. subtypes, and it has also been demonstrated that these subtypes vary geographically [21, 32]. Interestingly, ST4 has been suggested to be more pathogenic than other Blastocystis subtypes [32].
Extensive research shows that immunosuppression and use of immunosuppressive drugs increase the risk of detecting Blastocystis sp. [6, 28, 33]. However, in this study, no correlation was found among these factors. Some studies have stated that [20] Blastocystis sp. may be linked to irritable bowel syndrome (IBS), but this association was not observed in our case. A significantly lower prevalence of Blastocystis sp. was reported among patients who were infected by other parasites than those who were not. Enteric pathogen infection by different parasites has commonly been detected in different studies [23, 34]. Although in our study the presence of other parasites acted as a protective factor, it could be the result of a bias due to the fact that all participants were patients asked for coproparasitological examination, with a higher chance to find a pathogen, rather than if they had been randomly selected from population. Furthermore, infection by other parasites could produce changes in the intestinal flora that could hinder Blastocystis sp. colonization.
Given its retrospective nature, our study presents some limitations. Firstly, conventional microscopic methods were used for diagnosis rather than molecular methods even though there has been stated a relatively low sensitivity of estimation of the presence or absence of Blastocystis [35]. Besides, the small sample size could also be a limiting factor, but the power of the study was high enough to show differences among cases and controls. In addition, it is not known if patients were already infected before traveling. Moreover, the immigrant population group had been living in Spain for a long time and therefore could have acquired the infection in Spain. However, this cannot be confirmed, as the incubation period is not clearly known. Finally, recall bias was identified during the telephonic interviews (mostly related to traveling or to the presence of digestive symptoms); however, it only affects a small percentage of participants.
The results of the present study suggest that African people, recent traveling, and working with the public are risk factors for acquiring Blastocystis sp. On the other side, being infected by other intestinal parasite was a protective factor. Our study provides new insights into the epidemiology of Blastocystis sp. in industrialized countries in an urban population. Further research including molecular and epidemiological studies should be done. This would help to map prevalence and subtype distribution and to clarify the importance of risk factors depending on the area and would improve intervention strategies that could help to mitigate Blastocystis sp. transmission.
References
Barbosa CV, Barreto MM, De Jesus AR, Sodré F, D’avila Levy CM, Mauro J et al (2018) Intestinal parasite infections in a rural community of Rio de Janeiro (Brazil): prevalence and genetic diversity of Blastocystis subtypes. PLoS One 13:1–12
Dacal E, Saugar J, De Lucio A, De Mingo MH, Robinson E, Köster P et al (2018) Prevalence and molecular characterization of Strongyloides stercoralis, Giardia duodenalis, Cryptosporidium spp. and Blastocystis spp. isolates in school children in Cubal, Western Angola. Parasit Vectors 11:1–18
Liao CW, Chuang TW, Huang YC, Chou CM, Chiang CL, Lee FP et al (2017) Intestinal parasitic infections: current prevalence and risk factors among schoolchildren in capital area of the Republic of Marshall Islands. Acta Trop 176:242–248
Popruk S, Rada Pintong A, Radomyos P (2013) Diversity of Blastocystis subtypes in humans. J Trop Med Parasitol 36:88–97
Kazmarekk A, Gola BE, Zarnoska Prymek H, Rawska A, Janzak D, Lewicki A et al (2017) Genetic diversity of Blastocystis hominis sensu lato isolated from humans in Poland. Przegl Epidemiol 71:539–546
Mohamed AM, Ahmed MA, Ahmed SA, Al-Semany SA, Alghamdi SS, Zaglool DA (2017) Predominance and association risk of Blastocystis hominis subtype 1 in colorectal cancer: a case control study. Infect Agent Cancer 12:21
El-Safadi D, Gaayeb L, Meloni D, Cian A, Poirier P, Wawryniak et al (2014) Children on Senegal river basin show the highest prevalence of Blastocystis sp. ever observed worldwide. BMC Infect Dis 14:1–11
Alfellani MA, Stesnvold CR, Vidal-Lapiedra A, Onuoha ES, Fagbenro-Beyjoku AF, Clark CG (2013) Variable geographic distribution of Blastocystis subtypes and its potential implications. Acta Trop 126:11–18
Heydary-Hengami M, Hamedi Y, Najadi-Asl M, Sharifi-Sarasiabi K (2018) Prevalence of intestinal parasites in food handlers of Bandar Abbas, Southern Iran. Iran J Public Health 47:111–118
Belleza MLB, Cadacio JLC, Borja MP, Solon JAA, Padilla MA, Tongol-Rivera PN et al (2015) Epidemiologic study of Blastocystis infection in an urban community in the Philippines. J Environ Public Health 2015:1–7
Javanmard E, Niyyati M, Ghasemi E, Mirjalali H, Asadzadeh-Aghdaei H, Zali MR (2018) Impacts of human development index and climate conditions on prevalence of Blastocystosis a systematic review and meta-analysis. Acta Trop 185:193–203
Leder K, Hellar ME, Sinclair MI, Fairley CK, Wolfe R (2005) No correlation between clinical symptoms and Blastocystis hominis in immunocompetent individuals. J Gastroenterol Hepatol 20:1390–1394
Sohail MR, Fischer PR (2005) Blastocystis hominis and travelers. Travel Med Infect Dis 3:33–38
Eroglu F, Koltas IS (2010) Evaluation of the transmission mode of B. hominis by using PCR method. Parasitol Res 107(84):841–845
Salvador F, Sulleiro E, Sánchez-Montalvá A, Alonso C, Santos J, Fuentes I et al (2016) Epidemiological and clinical profile of adult patients with Blastocystis hominis infection in Barcelona, Spain. Parasit Vectors 9:1–7
Stensvold CR, Lewis HC, Hammerum AM, Porsbo LJ, Nielsen SS, Olsen KEP et al (2009) Blastocystis: unravelling potential risk factors and clinical significance of a common but neglected parasite. Epidemiol Infect 137:1655–1663
Wawrzyniak I, Poirier P, Viscolgliosi E, Dionigia M, Texier C, Delbac F et al (2013) Blastocystis, and unrecognized parasite: an overview of pathogenesis and diagnosis. Ther Adv Inf Dis 5:167–178
Paulos S, Köster P, Lucio A, Hernández-de-Mingo M, Cardona GA, Fernández-Crespo JC, Stensvold CR, Carmena D (2018) Occurrence and subtype distribution of Blastocystis sp. in humans, dogs and cats sharing household in northern Spain and assessment of zoonotic transmission risk. Zoonoses Public Health 65:993–1002
Del Aguila C, Navajas R, Gurbindo D, Ramos JT, Mellado MJ, Fenoy S, Muóz MA, Subirats M, Ruiz J, Pleniazek NJ (1997) Microsporidiosis in HIV-positive children in Madrid (Spain). J Eukaryot Microbiol 44(6):84–85
Bart A, Wentink-Bonnema EM, Gilis H, Verhaar N, Wassenaar CJ, Van Vugt M et al (2013) Diagnosis and subtype analysis of Blastocystis sp. in 442 patients in a hospital setting in the Netherlands. BMC Infect Dis 13:1–6
Stensvold CR, Clark CG (2016) Current status of Blastocystis: a personal view. Parasitol Int 65:763–771
Beghini F, Pasolli E, Truong TD, Putignani L, Caddiò SM, Segata N (2017) Large-scale comparative metagenomics of Blastocystis, a common member of the human gut microbiome. ISME J 11:2848–2863
Krogsgaard LR, Engsbro AL, Stensvold CR, Nielsen HV, Bytzer P (2015) The prevalence of intestinal parasites is not greater among individuals with irritable bowel syndrome: a population-based case-control study. Clin Gastroenterol Hepatol 13:507–513
González-Moreno O, Domingo L, Teixidor J, Gracenea M (2011) Prevalence and associated factors of intestinal parasitation: a cross-sectional study among outpatients with gastrointestinal symptoms in Catalonia, Spain. Parasitol Res 108:87–89
Ocaña-Losada C, Cuenca-Gómez JA, Cabezas-Fernández MT, Vázquez-Villegas K, Soriano-Pérez MJ, Cabeza-Barrera I et al (2018) Clinical and epidemiological characteristics of intestinal parasite infection by Blastocystis hominis. Rev Clin Esp 218:115–120
Martín-Sánchez AM, Canut-Blasco A, Hernández JR, Montes-Martínez I, Rodriguez JAG (1992) Epidemiology and clinical significance of Blastocystis hominis in different population groups in Salamanca, Spain. Eur J Epidemiol 8:553–559
El-Safadi D, Cian A, Nourrisson C, Pereira B, Morelle C, Bastien P et al (2016) Prevalence, risk factors for infection and subtype distribution of the intestinal parasite Blastocystis sp. from a large-scale multi-center study in France. BMC Infect Dis 16:451–462
Mohtashamipour M, Hoseini SG, Pestehchian N, Yousefi H, Fallah E, Hazratian T (2015) Intestinal parasitic infections in patients with diabetes mellitus: a case-control study. J Anal Res Clin Med 3:157–163
Ghimire A, Bhandaria S, Tandukar S, Amatya J, Bhandari D, Sherchand JB (2016) Enteric parasitic infection among HIV-infected patients visiting Tribhuvan University Teaching Hospital. Nepal BMC Res Not 9:1–5
Punsawad C, Phasuk N, Bunratsami S, Thongtup K, Siripakonuaong N, Nongnaul S (2017) Prevalence of intestinal parasitic infection and associated risk factors among village health volunteers in rural communities of Southern Thailand. BMC Public Health 17:1–9
Salim HR, Kumar GS, Vellayan S, Mak JW, Anuar AK, Init I et al (1999) Blastocystis in animal handlers. Parasitol Res 85:1032–1033
Alfellani MA, Jacob AS, Perea NO, Krecek RC, Taner-Mulla D, Verweij JJ et al (2013) Diversity and distribution of Blastocystis sp. subtypes in non-human primates. Parasitol. 140:966–971
Marcos LA, Gotuzzo E (2013) Intestinal protozoan infections in the immunocompromised host. Curr Opinion Inf Dis 26:295–301
Leelayoova S, Siripattanapipong S, Thathaisong U, Naaglor T, Taamasri P, Piyaraj P et al (2008) Drinking water: a possible source of Blastocystis spp. subtype 1 infection in schoolchildren of a rural community in Central Thailand. Am J Trop Med Hyg 79:401–406
Ramírez JD, Flórez C, Olivera M, Bernal MC, Giraldo JC (2017) Blastocystis subtyping and its association with intestinal parasites in children from different geographical regions of Colombia. PLoS One 12:1–13
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary material
: Standardized questionnaire to determine the demographic and clinical characteristics of patients. (DOCX 14 kb)
Rights and permissions
About this article
Cite this article
Hidalgo, L., Salvador, F., Sulleiro, E. et al. Evaluation of risk factors associated to detection of Blastocystis sp. in fecal samples in population from Barcelona, Spain: a case-control study. Eur J Clin Microbiol Infect Dis 38, 1241–1247 (2019). https://doi.org/10.1007/s10096-019-03532-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-019-03532-z