Abstract
The purpose of this study is to characterize Streptococcus suis isolates recovered from human infections regarding serotype distribution, genotypic profile, clinical manifestations, and epidemiology. A total of 668 S. suis isolates recovered from human infections in Thailand were characterized based on serotyping by multiplex PCR and co-agglutination, genotypic profiles by multilocus sequence typing, and PCR for virulence-associated genes, as well as review of medical records. Serotype 2 (94.6%) was predominant, followed by serotype 14 (4.5%), 24 (0.45%), 5 (0.3%), and 4 (0.15%). Multilocus sequence typing analyses revealed seven clonal complexes (CC): CC1 (56.43%), CC104 (31.74%), CC233/379 (5.4%), CC25 (4.5%), CC28 (0.9%), CC221/234 (0.6%), CC94 (0.15%), and two singletons. The CC1 group contained serotype 2 and 14 isolates, while CC25, 28, 104, and 233/379 consisted of serotype 2 isolates only. CC221/234 contained serotype 5 and 24 isolates, whereas the single serotype 4 isolate belonged to CC94. Two singletons contained serotype 5 (ST235) and 2 (ST236) isolates. Our data showed that ST1 isolates were more associated with meningitis than those of other STs (p < 0.001). The major route of infection was shown to be close contact with infected pigs or contaminated raw pork-derived products, including occupational exposure and recent consumption of raw pork products. This study revealed a relatively large number of CCs of S. suis causing human infection in Thailand. Among them, CC1 followed by CC104, with serotype 2 isolates, are predominant. Food safety campaigns and public health interventions would be important for controlling the S. suis infection in humans.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Streptococcus suis, an important zoonotic pathogen, causes invasive infections in humans in close contact with infected pigs or contaminated pork-derived products [1]. The number of reported human cases, especially in Southeast Asian countries, has dramatically increased in the past few years [1, 2]. Currently, 29 serotypes of Streptococcus suis have been recognized [3]. Of these serotypes, serotype 2 is the most prevalent in S. suis human infections, although cases caused by serotypes 4, 5, 9, 14, 16, 21, 24, and 31 have also been reported [1, 2, 4,5,6,7,8]. In a retrospective study that included human field strains recovered from 2006 to 2008 in Thailand, clonal complexes (CC) 1, 25, 28, and 104 were shown to be responsible for human infections, with sequence type (ST) 1 (within CC1) being the most frequently found, followed by ST104 (CC104) [8].
In the present study, an additional 668 S. suis isolates recovered from human infections in Thailand between 2009 and 2012 were further characterized regarding serotype distribution, genotypic profile, and clinical manifestations.
Materials and methods
Bacterial isolates and identification
A total of 668 isolates of S. suis recovered from blood, cerebrospinal fluid (CSF), synovial fluid, or other body fluids were collected from 41 hospitals in 39 provinces distributed in 5 regions (north, northeast, central, east, and south) of Thailand between January of 2009 and December of 2012 [Supplemental file 1]. Presumptive identification and antimicrobial susceptibility of S. suis were carried out in the hospitals where the pathogen was originally isolated and sent us to confirmation. A multiplex PCR assay and the co-agglutination test were used to identify and serotype these S. suis isolates [9, 10].
Genotypic profiles
Multilocus sequence typing (MLST) was performed as described elsewhere [11, 12]. MLST alleles, resulting STs, and the CC were assigned and analyzed using the S. suis MLST database, which can be accessed at https://pubmlst.org/ssuis/. The presence of virulence-associated genes (VAG), including the extracellular protein factor (epf), the muramidase-released protein (mrp), and the suilysin (sly), was determined by PCR as described by Silva et al. [13].
Human cases and statistical analyses
The medical records of 659 cases were reviewed by attending physicians at local hospitals in Thailand using the clinical case record form approved by the Ethics Committee of the Department of Medical Sciences, Ministry of Public Health, Thailand. The medical records of the remaining nine patients were not available. The clinical manifestations of S. suis infections were classified into meningitis, sepsis, septic arthritis, infective endocarditis, and spontaneous peritonitis according to a criteria described elsewhere [8, 14,15,16,17]. Clinical isolates were categorized according to ST and VAG profiles. The association between these categories and two clinical manifestations (meningitis and non-meningitis) was analyzed by Fisher’s exact test with the Stata version 10.0 software (StataCorp, College Station, TX, USA). Data were considered significant at p < 0.01.
Results
Serotype distribution of S. suis isolates
Of the 668 isolates, multiplex PCR and the co-agglutination test with specific antisera revealed 632 isolates of serotype 2 (94.6%), 30 of serotype 14 (4.5%), three of serotype 24 (0.45%), two of serotype 5 (0.3%), and one of serotype 4 (0.15%) (Table 1).
Genotypic profiles of S. suis isolates
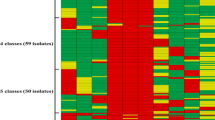
MLST classified 668 isolates into seven CCs and two singleton (Table 1 and Fig. 1). The CCs were identified as follows: CC1 (56.43%), CC104 (31.74%), CC233/379 (5.4%), CC25 (4.5%), CC28 (0.9%), CC221/234 (0.6%), and CC94 (0.15%). The CC1 contained more than 50% of all serotype 2 isolates, with ST1 being the predominant sequence type. Interestingly, CC1 also contained all 30 serotype 14 isolates, with 29 being ST105 and only one belonging to ST11. CC104 was the second most important group with 212 isolates, all serotype 2, with seven different STs. CC25 was composed by 30 isolates, also all serotype 2, with 7 different STs, whereas CC233/379, a newly herein described CC responsible for human infections, included ST233 and ST379, with all isolates also belonging to serotype 2 (Table 1 and Fig. 1). Interestingly, CC233/379 was closely related to CC104, with two locus variants (gki and thrA). Indeed, the allelic profile of CC233/379 is 8-30-5-(72/97)-44-21-75, whereas that of ST104 is 8-30-5-1-44-21-4. CC28 was also composed of serotype 2 isolates belonging to either ST28 or ST382. Isolates belonging to serotypes other than 2 and 14 were distributed in CC94 (serotype 4) and CC221/234 (serotypes 5 and 24). Two isolates could not be attributed to any known CC, belonging to ST235 (serotype 5) and ST236 (serotype 2) (Table 1).
An eBURST analysis of the entire S. suis MLST database (accessed on July 25, 2017). Clonal complexes relevant to human infection in Thailand are circled and labeled. Clonal complexes and the predicted founding STs are indicated by blue dots. The size of the dots is relative to the number of isolates with the respective ST present in the database (Color figure online)
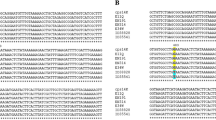
As shown in Table 1, eight VAG profiles were obtained by PCR: epf +/sly +/mrp + (n = 377, 56.4%), epf −/sly +/mrp + (n = 2, 0.3%), epf −/sly +/mrp s (n = 2, 0.3%), epf−/sly−/mrp + (n = 20, 3%), epf−/sly−/mrp * (n = 12, 1.8%), epf−/sly−/mrp ** (n = 4, 0.6%), epf−/sly +/mrp − (n = 248, 37.2%), and epf−/sly−/mrp− (n = 3, 0.4%). Serotype 2 showed six VAG profiles: epf+/sly +/mrp + or epf −/sly+/mrps profiles, mainly found in CC1; epf −/sly−/mrp+ or epf −/sly−/mrp* or epf −/sly−/mrp** profile associated with CC25; epf −/sly−/mrp+ profile found in CC28; and epf−/sly +/mrp− profile associated with CC104 and CC233/379. Serotype 14 (CC1) isolates presented epf +/sly +/mrp + or epf −/sly +/mrps profiles, while serotype 4 (CC94) showed epf −/sly +/mrp +. Finally, two serotype 5 isolates (ST221 and ST235) revealed a epf+/sly +/mrp +, while the VAG profile of isolates of serotype 24 (CC221/234) was epf−/sly−/mrp −.
Isolation sites and dates
Of the 668 isolates, 391 (58.53%) were recovered from patients of the northern region, 140 (20.96%) from patients of the northeastern region, 102 (15.26%) from those of the central region, 30 (4.5%) from those of the east region, and 5 (0.75%) from those of the southern region (Supplemental file 1). The dates of S. suis isolation as well as their relationship with temperature or rainfall are shown in Fig. 2. In 2009, human cases occurred more frequently in September, whereas 1 year later, the peak was between April and June. Human cases in 2011 increased from April to August and in 2012, the peaks were increased from March to May. It is interesting that the peak of human cases in 2010–2012 are, in general, in agreement with rising rainfall (Fig. 2). In general, the mean temperature in the whole of Thailand between 2009 and 2012 was about 27.2 °C (range 23.2–29.1), 27.9 °C (range 25.1–30.8), 26.8 °C (range 24.1–28.4), and 27.7 °C (range 25.4–29.4), respectively. Indeed, no significant changes of temperature during these years could be associated with the number of diagnosed cases (Fig. 2).
Clinical features and relationship with the genotypic profiles of S. suis isolates
The demographic data revealed that S. suis cases were recovered from 134 females (20.3%) and 525 males (79.7%). The mean age was 56.5 years old, and median age was 56 (range 23–92 years old). The clinical features of the 659 human cases of S. suis infection are summarized in Table 2. Meningitis cases (n = 141) were mainly caused by CC1 isolates (n = 118; 83.7%), especially ST1 (n = 106), followed by CC104 (n = 21; 14.9%). Sepsis (n = 501) could be associated with isolates belonging to all CCs and two singletons (ST235 and ST236). CC1 isolates (n = 239) also accounted for 47.7% of the sepsis cases, followed by those of CC104 (n = 187; 37.3%). Infective endocarditis (n = 10) was mainly caused by CC1 isolates (n = 7). Septic arthritis cases (n = 5) were caused by CC1 isolates, whereas CC104 and CC233/379 isolates were associated with spontaneous peritonitis (n = 2) (Table 2).
A total of 423 out of 659 cases had a history of raw pork product consumption (64.2%), 74 cases (11.2%) had an occupation related to pig/pork products (slaughterer/farmer/butcher), and 162 cases (24.6%) did not have any information regarding pig contact or pork consumption. Eighty-four out of the 659 cases were fatal (12.7%), of which 21 cases were assigned to meningitis, 62 cases to sepsis, and one case was associated to infective endocarditis. Regarding antibiotic treatment, 598 patients (90.7%) received third-generation cephalosporin, such as ceftriaxone, 42 patients (6.4%) received penicillin, and 19 patients (2.9%) received both third-generation cephalosporin and penicillin. Susceptibility test by either disk diffusion or E-test (only penicillin) revealed all S. suis isolates including fatal 84 isolates were susceptible to antibiotics used for treatment (penicillin, ceftriaxone, cefotaxime). The characteristic symptom of hearing loss was found in 20.5% (135 cases), mostly associated with meningitis and/or sepsis. Associations of genotypic profiles with the clinical presentation showed that ST1 isolates were associated with meningitis (p < 0.001), whereas the ST104 isolates could be associated with non-meningitis cases (p < 0.001) (Table 3). In addition, VAG profile of epf +/sly+/mrp+ was also associated with meningitis whereas epf −/sly+/mrp− and epf −/sly −/mrp + were associated with non-meningitis (Table 3).
Discussion
Our present data indicate that Thai patients are uniquely infected with a large variety of serotypes, differently from what has been described in other countries/regions [4, 5, 8]. Serotype 2 remained the main serotype causing human infections in Thailand during the period 2009–2012. This study confirms that serotype 14 is also more prevalent in Thailand than in other countries/regions [2, 6]. We also report here a second case of human infection due to a serotype 4 (Tables 1 and 2), this serotype having been described 30 years ago in a case of meningitis in the Netherlands [18]. The serotype 4 isolate in this study was recovered from a sepsis case and belongs to ST94 of CC94, while no information is available for the previous Dutch isolate [18].
MLST genotyping of S. suis collected between 2009 and 2012 also revealed a higher diversity than that observed in our previous study [8]. That study had shown four CCs (CC1 CC25, CC28, and CC104) while this study revealed seven CCs as described previously. CC94 and CC233/379 are newly emerging human infectious clones that have not been reported elsewhere before [2]. To the best of our knowledge, CC104, CC221/234, and CC233/379 are CCs exclusively found in Thailand. The unusual high number of isolates included in this study allowed us to note that S. suis serotype 2 strains isolated from humans in Thailand are much more diverse than previously thought [1, 2]. However, the major S. suis CCs caused human infection in worldwide are restricted to well-recognized CCs, for example, CC1 and CC20 are found in the Netherlands [19]; CC1, CC25, CC28, CC104, and CC221/234 in certain Asian countries (China, Vietnam, Thailand, Japan, Hong Kong, and Cambodia) [2, 5,6,7,8, 20]; CC1 in South America (Argentina) [21]; CC25 in North America (Canada and USA); and CC28 in North America and Japan [2, 20].
Our previous study also revealed that peaks of S. suis human cases occurred during the rainy season between 2006 and 2008 [8], which had also been described in China [22] and Northern Vietnam [23]. The peak in this study changed between years with no clear pattern; however, human cases seem to increase in accordance with rising rainfall, although no cause-effect explanation of such observations could be found. A study in Vietnam also showed a clear association between porcine reproductive and respiratory syndrome virus (PRRSv) outbreaks in pigs and S. suis infection in humans [24]. A highly virulent PRRSv strain was introduced in Thai swine herds in 2008 causing major outbreaks, and the virus was first isolated in 2010 [25]. More studies are needed to evaluate if the introduction of such a virus may have influenced the pattern of S. suis isolation from humans in Thailand.
Oral consumption of raw pork products is the major transmission route of this disease in Thailand. The existence of deep-rooted habitual consumption of raw pork products mainly in the northern part of Thailand may explain the higher number of isolates from these areas. In fact, this is another factor that may influence the peak of infection during the years, since there is, in general, an increase in the frequency of raw pork products consumed by local people during traditional Thai festivals. A recent study confirmed the effectiveness of a food safety campaign for controlling S. suis infection in humans in the Phayao Province of Thailand between January 2011 and December 2011 [26]. The trends of incidence proportion before (2008–2010) and after (2011–2013) the campaign revealed a 3.94/100,000 persons decrease in the trend of incidence proportion after campaign (p < 0.001), with the cost to reduce to an incidence proportion of 1.0/100,000 persons around US$380 [26]. Therefore, a continuous campaign including introducing educational programs in childhood or improve the sanitation of pork processing or additional and alternative public health interventions are needed to decrease or eliminate the disease.
The findings reported herein confirm the association between ST1 strains and meningitis cases, whereas ST104 strains are associated with non-meningitis cases as previously reported [8]. This may indicate that ST1 strains might have an advantage in bacterial survival resisting host immunity, with rapid multiplication in the bloodstream, and high levels of bacteremia, which was already associated with the development of meningitis [27]. In addition, the suilysin, a S. suis hemolysin typically present in ST1 strains, was confirmed to contribute to the development of bacterial meningitis in a mouse model [28].
This study revealed a higher mortality (12.7%) of S. suis cases than in a retrospective study from 2006 to 2008 in Thailand (9.5%) [8]; indeed, a population-based study in Phayao Province in Thailand revealed 16.1% of the case fatality rate, which is even higher [29]. In other countries, the case fatality rates were 2.6% in Vietnam, 18.6% in China, 5% in Hong Kong, and 6.7% in the Netherlands [23, 30]. Globally, the fatality rate of S. suis infection is around 12% [31]. Regarding antibiotic treatment, no relationship between the treatment used and the fatality could be found. Since all S. suis isolates in this study revealed susceptible to antibiotics used for treatment, the cause of death in our patients remains uncertain; however, this may be due to delayed admission, underlying diseases, rapid disease progression, or infection with higher virulence strains of S. suis, although the latter cause remains to be confirmed.
In conclusion, this study revealed a relatively large number of CCs of S. suis causing human infection in Thailand. Among them, CC1 followed by CC104, with serotype 2 isolates, are predominant. Food safety campaigns and public health interventions would be important for controlling the S. suis infection in humans.
References
Gottschalk M, Xu J, Calzas C, Segura M (2010) Streptococcus suis: a new emerging or an old neglected zoonotic pathogen? Future Microbiol 5:371–391
Goyette-Desjardins G, Auger JP, Xu J, Segura M, Gottschalk M (2014) Streptococcus suis, an important pig pathogen and emerging zoonotic agent—an update on the worldwide distribution based on serotyping and sequence typing. Emerg Microbes Infect 3:e45
Okura M, Osaki M, Nomoto R, Arai S, Osawa R, Sekizaki T, Takamatsu D (2016) Current taxonomical situation of Streptococcus suis. Pathogens 24:E45
Kerdsin A, Hatrongjit R, Gottschalk M, Takeuchi D, Hamada S, Akeda Y, Oishi K (2017) Emergence of Streptococcus suis serotype 9 infection in human. J Microbiol Immunol Infect 50:545–546
Hatrongjit R, Kerdsin A, Gottschalk M, Takeuchi D, Hamada S, Oishi K, Akeda Y (2015) First human case report of sepsis due to infection with Streptococcus suis serotype 31 in Thailand. BMC Infect Dis 15:392
Kerdsin A, Oishi K, Sripakdee S, Boonkerd N, Polwichai P, Nakamura S, Uchida R, Sawanpanyalert P, Dejsirilert S (2009) Clonal dissemination of Streptococcus suis serotype 14 in Thailand. J Med Microbiol 58:1508–1513
Kerdsin A, Dejsirilert S, Sawanpanyalert P, Boonnark A, Noithachang W, Sriyakum D, Simkum S, Chokngam S, Gottschalk M, Akeda Y, Oishi K (2011) Sepsis and spontaneous bacterial peritonitis in Thailand. Lancet 378:960
Kerdsin A, Dejsirilert S, Puangpatra P, Sripakdee S, Chumla K, Boonkerd N, Polwichai P, Tanimura S, Takeuchi D, Nakayama T, Nakamura S, Akeda Y, Gottschalk M, Sawanpanyalert P, Oishi K (2011) Genotypic profile of Streptococcus suis serotype 2 and clinical features of infection in humans, Thailand. Emerg Infect Dis 17:836–842
Kerdsin A, Akeda Y, Hatrongjit R, Detchawna U, Sekizaki T, Hamada S, Gottschalk M, Oishi K (2014) Streptococcus suis serotyping by a new multiplex PCR. J Med Microbiol 63:824–830
Gottschalk M, Higgins R, Boudreau M (1993) Use of polyvalent coagglutination reagents for serotyping of Streptococcus suis. J Clin Microbiol 31:2192–2194
King SJ, Leigh JA, Heath PJ, Luque I, Tarradas C, Dowson CG, Whatmore AM (2002) Development of a multilocus sequence typing scheme for the pig pathogen Streptococcus suis: identification of virulent clones and potential capsular serotype exchange. J ClinMicrobiol 20:3671–3680
Rehm T, Baums CG, Strommenger B, Beyerbach M, Valentin-Weigand P, Goethe R (2007) Amplified fragment length polymorphism of Streptococcus suis strains correlates with their profile of virulence-associated genes and clinical background. J Med Microbiol 56:102–109
Silva LM, Baums CG, Rehm T, Wisselink HJ, Goethe R, Valentin-Weigand P (2006) Virulence-associated gene profiling of Streptococcus suis isolates by PCR. Vet Microbiol 115:117–127
Muchart DJ, Bhaganjee S (1997) American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference definitions of the systemic inflammatory response syndrome and allied disorders in relation to critically injured patients. Crit Care Med 25:1765–1795
Goldenberg DL (1998) Septic arthritis. Lancet 351:197–202
Durack D, Lukes AS, Bright DK (1994) New criteria for diagnosis of infective endocarditis: utilization of specific echocardiographic findings. Am J Med 96:200–209
Rimola A, García-Tsao G, Navasa M, Piddock LJ, Planas R, Bernard B, Inadomi JM (2000) Diagnosis, treatment and prophylaxis of spontaneous bacterial peritonitis: a consensus document. Int Ascites Club J Hepatol 32:142–153
Arends JP, Zanen HC (1988) Meningitis caused by Streptococcus suis in humans. Rev Infect Dis 10:131–137
Schultsz C, Jansen E, Keijzers W, Rothkamp A, Duim B, Wagenaar JA, van der Ende A (2012) Differences in the population structure of invasive Streptococcus suis strains isolated from pigs and from humans in the Netherlands. PLoS One 7:e33854
Segura M, Fittipaldi N, Calzas C, Gottschalk M (2017) Critical Streptococcus suis virulence factors: are they all really critical? Trends Microbiol 25:585–599
Callejo R, Zheng H, Du P, Prieto M, Xu J, Zielinski G, Auger JP, Gottschalk M (2016) Streptococcus suis serotype 2 strains isolated in Argentina (South America) are different from those recovered in North America and present a higher risk for humans. JMM Case Rep 3:e005066
Kay R, Cheng AF, Tse CY (1995) Streptococcus suis infection in Hong Kong. QJM 88:39–47
Wertheim HF, Nghia HD, Taylor W, Schultsz C (2009) Streptococcus suis: an emerging human pathogen. Clin Infect Dis 48:617–625
Huong VT, Thanh LV, Phu VD, Trinh DT, Inui K, Tung N, Oanh NT, Trung NV, Hoa NT, Bryant JE, Horby PW, Kinh NV, Wertheim HF (2016) Temporal and spatial association of Streptococcus suis infection in humans and porcine reproductive and respiratory syndrome outbreaks in pigs in northern Vietnam. Epidemiol Infect 144:35–44
Charoenchanikran P, Kedkovid R, Sirisereewan C, Woonwong Y, Arunorat J, Sitthichareonchai P, Sopipan N, Jittimanee S, Kesdangsakonwut S, Thanawongnuwech R (2016) Efficacy of Fostera® PRRS modified live virus (MLV) vaccination strategy against a Thai highly pathogenic porcine reproductive and respiratory syndrome virus (HP-PRRSV) infection. Trop Anim Health Prod 48:1351–1359
Takeuchi D, Kerdsin A, Akeda Y, Chiranairadul P, Loetthong P, Tanburawong N, Areeratana P, Puangmali P, Khamisara K, Pinyo W, Anukul R, Samerchea S, Lekhalula P, Nakayama T, Yamamoto K, Hirose M, Hamada S, Dejsirilert S, Oishi K (2017) Impact of a food safety campaign on Streptococcus suis infection in humans in Thailand. Am J Trop Med Hyg 96:1370–1377
Auger JP, Fittipaldi N, Benoit-Biancamano MO, Segura M, Gottschalk M (2016) Virulence studies of different sequence types and geographical origins of Streptococcus suis serotype 2 in a mouse model of infection. Pathogens 5(3)
Takeuchi D, Akeda Y, Nakayama T, Kerdsin A, Sano Y, Kanda T, Hamada S, Dejsirilert S, Oishi K (2014) The contribution of suilysin to the pathogenesis of Streptococcus suis meningitis. J Infect Dis 209:1509–1519
Takeuchi D, Kerdsin A, Pienpringam A, Loetthong P, Samerchea S, Luangsuk P, Khamisara K, Wongwan N, Areeratana P, Chiranairadul P, Lertchayanti S, Petcharat S, Yowang A, Chaiwongsaen P, Nakayama T, Akeda Y, Hamada S, Sawanpanyalert P, Dejsirilert S, Oishi K (2012) Population-based study of Streptococcus suis infection in humans in Phayao Province in northern Thailand. PLoS One 7:e31265
Ma E, Chung PH, So T, Wong L, Choi KM, Cheung DT, Kam KM, Chuang SK, Tsang T (2008) Collaborative study group on Streptococcus suis infection in Hong Kong Streptococcus suis infection in Hong Kong: an emerging infectious disease? Epidemiol Infect 136:1691–1697
Huong VT, Ha N, Huy NT, Horby P, Nghia HD, Thiem VD, Zhu X, Hoa NT, Hien TT, Zamora J, Schultsz C, Wertheim HF, Hirayama K (2014) Epidemiology, clinical manifestations, and outcomes of Streptococcus suis infection in humans. Emerg Infect Dis 20:1105–1114
Acknowledgments
We thank J. P. Auger for reviewing the manuscript.
Contributors
All authors have read and approved the final article. AK, YA, DT, and KO participated in the conception and design of the study and analysis and interpretation of data. AK, MG, and KO drafted the manuscript. All authors have final approval of the version to be submitted.
Funding
This study was funded by the Japan Society for the Promotion of Science (KAKENHI 21406027) and Japan Initiative for a Global Research Network on Infectious Diseases launched by the Ministry of Education, Science, and Culture of Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics
This study was reviewed and approved by the Ethics Committees of the Department of Medical Sciences, Ministry of Public Health, Thailand. Medical record reviews were conducted by the medical doctors under the protocol approved by the Ethics Committees.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Kerdsin, A., Akeda, Y., Takeuchi, D. et al. Genotypic diversity of Streptococcus suis strains isolated from humans in Thailand. Eur J Clin Microbiol Infect Dis 37, 917–925 (2018). https://doi.org/10.1007/s10096-018-3208-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-018-3208-8