Abstract
We evaluated the application of nucleic acid amplification (NAA) in liquid cultures for the early detection of Mycobacterium tuberculosis. The Cobas TaqMan MTB test, IS6110 real-time PCR, and hsp65 PCR-restriction fragment length polymorphism (RFLP) analysis were used to detect BACTEC MGIT 960 (MGIT) cultures on days 3, 5, 7, and 14. The procedure was initially tested with a reference strain, H37Rv (ATCC 27294). Subsequently, 200 clinical specimens, including 150 Acid Fast bacillus (AFB) smear-positive and 50 AFB smear-negative samples, were examined. The Cobas TaqMan MTB test and IS6110-based PCR analysis were able to detect M. tuberculosis after 1 day when the inoculum of H37Rv was >3 x 10−2 CFU/ml. After a 5-day incubation in the MGIT system, all three NAA assays had a positive detection regardless of the inoculum size. After a 1-day incubation of the clinical specimens in the MGIT system, the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for the Cobas TaqMan MTB assay were 70.2%, 100%, 100%, and 82.3% respectively. For IS6110-based PCR analysis, these values were 63.1%, 100%, 100%, and 78.9%, and were 88.1%, 100%, 100%, and 92.1% respectively for hsp65 PCR-RFLP analysis. After a 3-day incubation, the specificity and PPV were 100% for all three NAA tests; the Cobas TaqMan MTB assay had the best sensitivity (97.6%) and NPV (98.3%). The sensitivity, specificity, PPV, and NPV for conventional culture analysis were 98.8%, 100%, 100%, and 99.1%. Thus, NAA may be useful for the early detection of M. tuberculosis after 3 days in MGIT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2007, the World Health Organization (WHO) issued a policy that recommended use of liquid culture methods for culture and drug susceptibility testing as a standard for tuberculosis (TB) diagnosis and case management [1]. However, Mycobacteria tuberculosis grows slowly, requiring time to be detected by conventional culture methods. BACTEC MGIT 960 liquid culture tubes that contain 7 ml of Middlebrook 7H9 broth supplemented with oleic acid, albumin, dextrose and catalase (BBL MGIT OADC) and BBL MGIT PANTA (an antibiotic mixture of polymyxin B, amphotericin B, nalidixic acid, trimethoprim, and azlocillin) enhance the growth of Mycobacteria [2]. This system can efficiently shorten the turnaround time for growth detection of Mycobacteria from clinical specimens [3]. In Taiwan, approximately 90% of clinical mycobacteriology laboratories use a combination of solid and liquid culture methods for the isolation of Mycobacteria from clinical specimens [4]. Although the time to positivity for mycobacterial detection can be accelerated using liquid culture systems, it did not shorten the time for species identification [5].
Nucleic acid amplification (NAA) methods, which detect targeted sequences directly from clinical specimens, shorten the time of identification of TB [6, 7]. A number of commercial systems have been developed, including the Probe Tec ET system, the Cobas Amplicor MTB test, the CobasTaqMan MTB test, the amplified M. tuberculosis direct test, and Xpert®MTB/RIF. These molecular diagnostic assays are used to test clinical specimens. Although the specificity of the NAA is high in Acid Fast bacillus (AFB) smear-positive specimens (87.5% to 100%), the sensitivity is relatively low (50.0% to 70.8%) in AFB smear-negative specimens [8]. Detecting TB with NAA in a liquid culture medium, which may have the advantages of amplifying nucleic acid targets while diluting inhibitors of amplification, may provide rapid, accurate diagnosis of TB before there is a positive culture signal from the MGIT system. The aim of this study was to evaluate this procedure to determine whether it improves the sensitivity and specificity of NAA tests after a period of incubation in liquid culture. In the first part of the study, we used various inoculum concentrations of a reference strain of M. tuberculosis to determine the smallest inoculum of bacilli for three NAA methods. In the second part of the study, we used clinical samples to evaluate the performance of applying NAA in liquid culture specimens before a positive culture signal was obtained by the MGIT system.
Materials and methods
Evaluation of the culture-enhanced NAA tests with an in-vitro-prepared M. tuberculosis reference strain
A reference strain of M. tuberculosis, H37Rv (ATCC 27294), was cultured on a Lowenstein–Jensen (LJ) slant, and colonies were dispersed in sterile water to obtain a suspension containing approximately 3.0 × 108 CFU/ml. We performed 10-fold serial dilutions from the stock H37Rv strain to obtain inoculum sizes ranging from 3.0 × 108 to 3.0 × 10−2 CFU/ml.
Seven Bactec MGIT 960 culture tubes (Becton Dickinson and Company, Sparks, MD, USA) were inoculated with each suspension (1 ml/tube), and were incubated in a BD Bactec MGIT system (Becton Dickinson and Company, Taipei, Taiwan) at 37°C to evaluate the association between concentration and positive detection in the MGIT system. One of the seven tubes was left in the instrument until a positive result was obtained, to determine the time to positivity in MGIT broth cultures. The six other tubes were removed from the instrument for NAA tests (Cobas TaqMan MTB test, IS6110 real time PCR, and hsp65 PCR-restriction fragment length polymorphism [RFLP]) at days 1, 3, 5, 7, 10, and 14, and an aliquot of 300 μl was removed from each tube. The procedures were repeated thrice.
Clinical specimen processing, culture and identification
The study was approved by the Review Board Committee of Kaohsiung Medical University Hospital, Kaohsiung, Taiwan (IRB No. KMUH-IRB-970369). Two hundred clinical specimens, including 193 respiratory specimens, two cerebrospinal fluid, two pericardial effusion, two urine samples and one pleural effusion sample, were collected from patients with suspected TB at Kaohsiung Medical University Hospital, Kaohsiung, Taiwan, from October to December 2011. The specimens were subjected to subsequent mycobacterial tests, including AFB smear, microscopic examinations, MGIT culture, Cobas TaqMan MTB test, IS6110-based PCR, and hsp65 PCR-RFLP analysis.
Clinical specimens were digested and decontaminated using the N-acetyl-L-cysteine-NaOH method, neutralized with phosphate buffer (67mM XX, pH 6.8), and centrifuged [9]. The auramine–rhodamine fluorochrome staining method was used for microscopic examination; positive microscopy results were identified by the Kinyoun acid-fast staining method [10].
Portions (0.5 ml) of the sediment from each specimen were used to inoculate a LJ tube, a 7H11 agar plate, and Bactec MGIT 960 tube (Becton Dickinson and Company) supplemented with oleic acid, albumin, dextrose, catalase (BBL MGIT OADC), and PANTA Plus (both products from Becton Dickinson and Company) [2].
The MGIT tubes were incubated at 35°C and monitored automatically every 1 h for fluorescence intensity. The tubes were incubated until they were positive or for 42 days. AFB smears from growth-positive MGIT tubes were produced. Colonies from AFB-positive tubes were subcultured onto a LJ tube and a 7H11 agar plate, which were incubated at 37°C for 8 weeks and examined weekly for positive cultures. Mycobacteria isolated from the cultures were identified by morphological and biochemical analyses and were further confirmed by BD MGIT TBc identification test (Becton Dickinson and Company) [11] and PCR-RFLP analysis as previously described [12].
DNA extraction from MGIT medium
An aliquot of 300 μl from each MGIT medium was mixed with 600 μL of cell lysis buffer (Geneaid, Taipei, Taiwan) using a vortex mixer and then incubated at 80°C for 5 min. Thereafter, this specimen was cooled at room temperature, and 300 μl of protein precipitation solution was added followed by centrifugation at 14,000 rpm for 10 min at 4°C. After the supernatant was removed, 800 μl of 100% isopropanol was added, and the solution was centrifuged at 14,000 rpm for 10 min after cooling at 4°C for 2 h. After the supernatant was carefully removed, 600 μl of 70% alcohol was added. Following centrifugation at 14,000 rpm for 10 min at 25°C, the supernatant and residual alcohol were carefully removed. After desiccating the sample, 50 μl of water was added then incubated at 85°C for 10 min. The clarified lysate was stored at −20°C until further use.
NAA assays for analysis of specimens in MGIT media
We used three NAA tests to detect M. tuberculosis in MGIT medium. After the specimens were processed for incubation in the MGIT system, 300-μl aliquots from each sample were collected for detection by NAA assays at days 1, 3, 5, 7, 10, and 14.
-
a.
Cobas TaqMan MTB test
The Cobas TaqMan MTB tests (Roche, Basel, Switzerland) were conducted according to the manufacturer’s instructions, which included two major steps: preparation of specimen DNA and real-time PCR. The assay permits the detection of amplified TB amplicons and an internal control DNA, which are simultaneously amplified and detected. Briefly, 100-μl aliquots of liquefied, decontaminated specimens were mixed with 500 μl of specimen wash solution and centrifuged at 12,500 rpm for 10 minutes. The Cobas TaqMan 48 analyzer determined the cycle threshold value (C T ) for the M. tuberculosis DNA, and confirmed that the C T values of the internal positive and negative control DNA were within the normal ranges. The internal control DNA was used to detect polymerase inhibitors that might be present in the specimens [7, 13].
-
b.
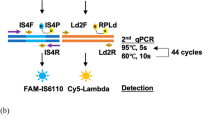
IS6110-based PCR
IS6110-based PCR is a useful genotyping method for tuberculosis diagnostics and epidemiologic studies [14]. IS6110-based PCR was performed according to the method described by Thierry et al. [15]. The primers used for this assay were MTB1007 (5′-GTG CGG ATG GTC GCA GAG AT-3′) and MTB1008 (5′-CTC GAT GCC CTC ACG GTT CA-3′).
-
c.
hsp65 PCR-RFLP analysis
The hsp65 gene is present in all species of Mycobacteria, and hsp65 sequence variations are useful for phylogenetic analysis and species identification [16]. A 439-bp fragment of the hsp65 gene was amplified by PCR using two specific primers Tb11 (5′- ACCAACGATGGTGTGTCCAT-3′) and Tb12 (5′-CTTGTCGAACCGCATACCCT-3′). The PCR products were digested with BstEII and the HaeIII [17], and the species were identified by similarity of restriction patterns using the PRASITE database (http://app.chuv.ch/prasite/index.html).
Analysis of discrepant results
Conventional cultures were primarily considered the “gold standard” for performance calculations. When discrepant results between the three NAA tests and culture occurred, the test results from the adjunct BD MGIT TBc identification (Becton Dickinson and Company, Sparks, MD, USA) and GenoType Mycobacterium CM assays (Hain Lifescience GmbH, Nehren, Germany) and a review of the patient’s clinical history were taken into consideration for resolving discrepancies. When a discrepancy concerning TB occurred, the medical data of a patient, including radiographic findings, chest symptoms, and history of antibiotics were also reviewed. Based on these data, patients were classified into five groups according to the recommendations of the American Thoracic Society; patients in groups 3, 4, or 5 were regarded as having TB [18]. For example, a NAA-positive but conventional culture-negative specimen was considered a true positive if the diagnosis of TB was supported by at least one other molecular assay and by the clinical data. In contrast, a NAA-positive but culture-negative specimen was considered a false positive if the positivity could not be confirmed by any other molecular assay, and diagnosis of TB could not be supported by the clinical data.
Performance analysis
Using the results of the conventional culture as the gold standard, the performance of these NAA assays was analyzed. To assess the performance of these assays, the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated after discrepant analysis [19].
Results
Inoculum size and time to positive detection required for identification of M. tuberculosis reference strain by NAA tests
As shown in Table 1, the time to positivity (detected by the MGIT system) with MGIT broth cultures of inoculum sizes ranging from 3 × 108 to 3 × 10−2 CFU/ml was between 5 and 14 days. All three NAA tests were able to detect MTBC at day 1 of MGIT culture at inoculum sizes ranging from 3 × 108 to 3 × 102 CFU/ml. In addition, both IS6110-based PCR and Cobas TaqMan tests were able to detect M. tuberculosis after 1 day in culture with the lowest tested inoculum size (3 × 10−2 CFU/ml). After 5 days in culture in the MGIT instrument, hsp65 PCR-RFLP analysis were also able to detect M. tuberculosis at an inoculum concentration of 3 × 10−2 CFU/ml (Table 1).
Detection of M. tuberculosis in clinical specimens using NAA tests
Clinical specimens, including 150 AFB smear-positive and 50 AFB smear-negative samples, were enrolled for evaluation. Of the 150 AFB smear-positive samples, 12 were AFB (±), 74 were 1+, 28 were 2+, 25 were 3+, and 11 were 4+. As shown in Fig. 1, 118 of 200 MGIT tubes (59.0%) yielded positive culture results detected by the MGIT system, of which 99 specimens (83.9%) were positive after 5 days inoculation. Among these positive cultured isolates in the MGIT system, 83/118 (70.3%) were identified as M. tuberculosis, including 82 from AFB smear-positive specimens and one from an AFB smear-negative specimen.
Detection of 118 culture-positive reactions over the 14-day study period in MGIT system. Within the first 3 days, 19/118 positive reactions (16.1%) were detected. Among the specimens with positive reactions, 62/118 (52.5%) were confirmed as Mycobacteria tuberculosis and 31/118 (26.3%) were identified as nontuberculosis mycobacteria by conventional tests
Analysis of discrepant results
Of the 200 clinical samples analyzed, 84 were positive for TB, and 116 were negative for TB. The detailed analysis of the discrepant results is presented in Table 2. There were three discrepancies between the NAA results and those from conventional culture and identification techniques. The Cobas TaqMan MTB assay yielded 199 concordant results (83 positive and 116 negative) with one false positive after the discrepancies were resolved. IS6110-based PCR yielded 197 concordant results (81 positive and 116 negative), and produced one false positive and two false negatives after the discrepancies were resolved. Finally, hsp65 PCR-RFLP yielded 198 concordant results (81 positive and 117 negative) with two false negatives after the discrepancies were resolved.
Performance analysis after discrepancies were resolved
As shown in Table 3, after a 1-day inoculation in the MGIT system, the sensitivity, specificity, PPV, and NPV for the Cobas TaqMan MTB assay were 70.2%, 100%, 100%, and 82.3% respectively. For IS6110-based PCR, these results were 63.1%, 100%, 100%, and 78.9% respectively, while they were 88.1%, 100%, 100%, and 92.1% respectively for hsp65 PCR-RFLP (Table 3).
After a 3-day incubation in the MGIT system, both the specificity and PPV were 100% for all three NAA tests in AFB smear-positive specimens, and the specificity was 100% for all of three NAA tests in smear-negative specimens. With the exception of one false negative result by the three NAA tests, the other 49 specimens revealed good agreement between the NAA results and conventional culture results. Only the Cobas TaqMan test detected this one sample as TB-positive after a 14-day inoculation in the MGIT system. As shown in Table 4, the overall specificity and PPV were 100% for all three NAA tests, with the Cobas TaqMan MTB assay having the best sensitivity (97.6%).
For the liquid culture after a 14-day incubation, the sensitivity, specificity, PPV, and NPV for the Cobas TaqMan MTB assay were 100%, 99.1%, 98.8%, and 100% respectively; these values were 98.8%, 100%, 100%, and 99.1% respectively for IS6110-based PCR and 97.6%, 100%, 100%, and 98.3% for hsp65 PCR-RFLP (Table 3). In comparison, the sensitivity, specificity, PPV and NPV for the conventional culture method were 98.8%, 100%, 100%, and 99.1% respectively.
Discussion
In the first part of this study, we found that both IS6110-based PCR and the Cobas TaqMan tests were able to detect specimens with a low inoculum concentration (3 × 10−2 CFU/ml) of TB after only 1 day in the MGIT system. After a 5-day incubation in the MGIT system, all three NAA assays had positive detection regardless of the inoculum sizes. This preliminary experiment revealed the possibility of detecting TB after only a 1-day incubation in a broth culture with a bacterial load of ≥3 x 10−2 CFU/ml by both IS6110-based PCR and Cobas TaqMan tests. Using the MGIT culture system alone required 5–14 days to detect culture-positive reactions for the inoculation sizes tested. Thus, use of both procedures (NAA methods for incubated MGIT cultures) decreased the time to detect TB as compared to the MGIT system alone
It has been reported that a specimen with a bacterial load of ≥104 CFU/ml is required to yield a positive smear [20]. It is presumed that the 150 AFB smear-positive specimens used in this study had bacterial loads of at least 104 CFU/ml. Given that all three NAA tests could detect the MGIT-incubated specimens with an initial bacterial load of 3 × 102 CFU/ml after only 1 day in culture, we hypothesize that the turnaround time for recovery of TB could be shortened to 1 day with this procedure for AFB smear-positive specimens. However, the sensitivity, specificity, PPV, and NPV for the NAA tests were less satisfactory for clinical specimens after a 1-day MGIT culture (Table 3). Moreover, although hsp65 PCR-RFLP revealed relatively less sensitivity for 1-day culture specimens of the laboratory strain, it had better sensitivity and NPV for 1-day cultures of clinical specimens. The negative results obtained from the culture-positive specimens using the NAA tests after a 1-day incubation in the MGIT system, and the inconsistent performance results between the laboratory strain and clinical specimens, may be related to a low bacterial load, the presence of PCR inhibitors, an unequal distribution of bacteria in the clinical specimens, or a sample volume effect [7, 21].
The combination of NAA with liquid culture methods has been evaluated in two studies [22, 23]. Aono et al. [22] used a procedure that combined the BACTEC MGIT 960 system with the COBAS Amplicor assay from Roche Diagnostics on day 7, and reported that the sensitivity, specificity, PPV, and NPV were 95.4 %, 100%, 100%, and 90.9% respectively using respiratory specimens. In addition, Noussair et al. [23] used a BacT/Alert instrument from bioMerieux and the GenoType Mycobacteria Direct (GTMD) assay from HainLifescience on day 15, which resulted in a sensitivity, specificity, PPV, and NPV of 88.6 %, 100%, 100%, and 97.9% respectively using nonrespiratory specimens. Both studies reported that the combination of liquid cultures with NAA tests was a highly sensitive and specific method for the detection of TB in different specimens. Our study is based on combining the MGIT 960 system with three NAA tests, including the in-house IS6110-based PCR, hsp65 PCR-RFLP analysis, and Cobas TaqMan MTB assay, which were able to detect M. tuberculosis after a 3-day incubation.
Both the IS6110 insertion element and the hsp65 gene have been widely investigated as target DNA fragments for the diagnosis of TB, with appropriate sensitivities and specificities for clinical specimens [24, 25]. Identification of TB using an IS6110-based PCR assay in positive MGIT cultures led to excellent sensitivity (100%) and specificity (100%) within 7–14 days [25, 26]. The hsp65 PCR-RFLP analysis is often used to identify M. tuberculosis and differentiate other non-tuberculous mycobacteria species in positive cultures, and it could be directly applied on clinical samples with acceptable sensitivity (84.5%) and specificity (100%) [27]. Our study confirmed that the inexpensive in-house NAA methods could be applied to MGIT culture specimens with acceptable sensitivity and excellent specificity (Table 4). The in-house tests cost less, and may be suitable for resource-limited conditions. The Cobas TaqMan MTB test is a quantitative assay that amplifies a segment of the 16S rRNA gene with the use of a TaqMan probe for the detection of M. tuberculosis DNA in clinical specimens [28]. The specificity of the Cobas TaqMan MTB assay is better than its predecessor, the Cobas Amplicor MTB system [29]. Furthermore, our results indicate that combining the Cobas TaqMan MTB assay with the MGIT system could shorten the turnaround time of identifying TB as compared to the combination assay used by Aono et al. [22].
For AFB smear-positive specimens after 3-day MGIT culture, the sensitivity, specificity, PPV, and NPV for the COBAS TaqMan tests were 99.0 %, 100%, 100%, and 99.0% respectively. There was one specimen that required a 14-day inoculation in the MGIT system to be identified by the COBAS TaqMan test. Thus, our results indicate that a negative Cobas TaqMan test result at day 14 can be sufficient to exclude the presence of TB. With AFB smear-positive and negative specimens taken together, the overall sensitivity, specificity, PPV, and NPV of the Cobas TaqMan test were 97.6%, 100%, 100%, and 98.3% respectively at day 3. The reported sensitivity, specificity, PPV, and NPV of the same test used directly for respiratory specimens (without inoculation in the MGIT system) were 91.5%, 98%, 91.5%, and 98.7% respectively [7]. Thus, detecting TB in MGIT culture specimens by NAA can lead to better sensitivity, specificity, and PPV.
In conclusion, the combination of MGIT and NAA tests is a highly sensitive and specific method for the early detection of M. tuberculosis in clinical specimens. The Cobas Taqman MTB test led to an excellent detection outcome at day 3. In addition, the in-house NAA methods, such as IS6110-based PCR and hsp65 PCR-RFLP, also can be useful for incubated broth culture specimens when cost is a concern.
References
World Health Organization (2007) Use of liquid TB culture and drug susceptibility testing (DST) in low and medium income settings. Summary report of the expert group meeting on the use of liquid culture media. WHO, Geneva, Switzerland
Lee JJ, Suo J, Lin CB, Wang JD, Lin TY, Tsai YC (2003) Comparative evaluation of the BACTEC MGIT 960 system with solid medium for isolation of mycobacteria. Int J Tuberc Lung Dis 7:569–574
Somoskövi A, Ködmön C, Lantos A, Bártfai Z, Tamási L, Füzy J, Magyar P (2000) Comparison of recoveries of mycobacterium tuberculosis using the automated BACTEC MGIT 960 system, the BACTEC 460 TB system, and Lowenstein–Jensen medium. J Clin Microbiol 38:2395–2397
Centers for Disease Control, Taipei T (2004) Laboratory manual of mycobacteria. Centers for Disease Control, Taipei, Taiwan
Katila ML, Katila P, Erkinjuntti-Pekkanen R (2000) Accelerated detection and identification of mycobacteria with MGIT 960 and COBAS AMPLICOR systems. J Clin Microbiol 38:960–964
Lee MR, Chung KP, Wang HC, Lin CB, Yu CJ, Lee JJ, Hsueh PR (2013) Evaluation of the Cobas TaqMan MTB real-time PCR assay for direct detection of Mycobacterium tuberculosis in respiratory specimens. J Med Microbiol 62:1160–1164
Yang YC, Lu PL, Huang SC, Jenh YS, Jou R, Chang TC (2011) Evaluation of the Cobas TaqMan MTB test for direct detection of Mycobacterium tuberculosis complex in respiratory specimens. J Clin Microbiol 49:797–801
Piersimoni C, Scarparo C (2003) Relevance of commercial amplification methods for direct detection of Mycobacterium tuberculosis complex in clinical samples. J Clin Microbiol 41:5355–5365
Kent PT, Kubica GP (1985) Public health mycobacteriology: a guide for the level III laboratory. U.S. Department of Health and Human Services, Centers for Disease Control, Atlanta, GA, USA
American Thoracic Society (1981) Diagnostic standards and classification of tuberculosis and other mycobacterial diseases (14th edition). Am Rev Respir Dis 123:343–358
Diagnostic Systems BD (2009) BD MGIT™ TBc ID identification test package insert, BD document L8085917(01). BD Diagnostic Systems, Sparks, MD, USA
Telenti A, Marchesi F, Balz M, Bally F, Bottger EC, Bodmer T (1993) Rapid identification of mycobacteria to the species level by polymerase chain reaction and restriction enzyme analysis. J Clin Microbiol 31:175–178
Kim JH, Kim YJ, Ki CS, Kim JY, Lee NY (2011) Evaluation of Cobas TaqMan MTB PCR for detection of Mycobacterium tuberculosis. J Clin Microbiol 49:173–176
Van Embden JD, Cave MD, Crawford JT, Dale JW, Eisenach KD, Gicquel B, Hermans P, Martin C, McAdam R, Shinnick TM, Small PM (1993) Strain identification of Mycobacterium tuberculosis by DNA fingerprinting: recommendations for a standardized methodology. J Clin Microbiol 31:406–409
Thierry D, Brisson-Noel A, Vincent-Levy-Frebault V, Nguyen S, Guesdon JL, Gicquel B (1990) Characterization of a Mycobacterium tuberculosis insertion sequence, IS6110, and its application in diagnosis. J Clin Microbiol 28:2668–2673
Kim H, Kim SH, Shim TS, Kim MN, Bai GH, Park YG, Lee SH, Chae GT, Cha CY, Kook YH, Kim BJ (2005) Differentiation of Mycobacterium species by analysis of the heat-shock protein 65 gene (hsp65). Int J Syst Evol Microbiol 55:1649–1656
Brunello F, Ligozzi M, Cristelli E, Bonora S, Tortoli E, Fontana R (2001) Identification of 54 mycobacterial species by PCR-restriction fragment length polymorphism analysis of the hsp65 gene. J Clin Microbiol 39:2799–2806
American Thoracic Society (1990) Diagnostic standards and classification of tuberculosis. Am Rev Respir Dis 142:725–735
Greco S, Girardi E, Navarra A, Saltini C (2006) Current evidence on diagnostic accuracy of commercially based nucleic acid amplification tests for the diagnosis of pulmonary tuberculosis. Thorax 61:783–790
Allen BW, Mitchison DA (1992) Counts of viable tubercle bacilli in sputum related to smear and culture gradings. Med Lab Sci 49:94–98
Reischl U, Lehn N, Wolf H, Naumann L (1998) Clinical evaluation of the automated COBAS AMPLICOR MTB assay for testing respiratory and nonrespiratory specimens. J Clin Microbiol 36:2853–2860
Aono A, Azuma Y, Mitarai S, Ogata H (2009) Rapid prediction of BACTEC MGIT 960 culture results by COBAS amplicor mycobacterium polymerase chain reaction detection. Diagn Microbiol Infect Dis 64:27–30
Noussair L, Bert F, Leflon-Guibout V, Gayet N, Nicolas-Chanoine MH (2009) Early diagnosis of extrapulmonary tuberculosis by a new procedure combining broth culture and PCR. J Clin Microbiol 47:1452–1457
Kim HJ, Mun HS, Kim H, Oh EJ, Ha Y, Bai GH, Park YG, Cha CY, Kook YH, Kim BJ (2006) Differentiation of Mycobacterial species by hsp65 duplex PCR followed by duplex-PCR-based restriction analysis and direct sequencing. J Clin Microbiol 44:3855–3862
Sion C, Degraux J, Delmee M (1999) Early identification of Mycobacterium tuberculosis and Mycobacterium avium using the polymerase chain reaction on samples positive by a rapid commercial culture system. Eur J Clin Microbiol Infect Dis 18:346–351
Sun JR, Lee SY, Perng CL, Lu JJ (2009) Detecting Mycobacterium tuberculosis in Bactec MGIT 960 cultures by inhouse IS6110-based PCR assay in routine clinical practice. J Formos Med Assoc 108:119–125
Varma-Basil M, Pathak R, Singh K, Dwivedi SK, Garima K, Kumar S, Sharma D, Dhiman B, Bose M (2010) Direct early identification of Mycobacterium tuberculosis by PCR-restriction fragment length polymorphism analysis from clinical samples. Jpn J Infect Dis 63:55–57
Diagnostics R (2009) CobasTaqMan Mycobacterium tuberculosis test: instruction manual. Roche Diagnostics, Mannheim, Germany
Bloemberg GV, Voit A, Ritter C, Deggim V, Bottger EC (2013) Evaluation of Cobas TaqMan MTB for direct detection of the Mycobacterium tuberculosis complex in comparison with Cobas Amplicor MTB. J Clin Microbiol 51:2112–2117
Acknowledgments
The authors thank colleagues at the Mycobacteriology Section of Clinical Microbiology Laboratory, Kaohsiung Medical University Hospital, for their support
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declared no conflict of interest.
Funding
This work is supported by Kaohsiung Medical University Hospital (KMUH101-1R13).
Ethical approval
This study was approved by the Institutional Review Board (IRB) of Kaohsiung Medical University Chung-Ho Memorial Hospital, Kaohsiung, Taiwan (KMUH-IRB-970369).
Informed consent
The study subjects were mycobacterial culture, and the written consent given by the patients was waived by the approving IRB.
Rights and permissions
About this article
Cite this article
Lin, S.Y., Hwang, S.C., Yang, Y.C. et al. Early detection of Mycobacterium tuberculosis complex in BACTEC MGIT cultures using nucleic acid amplification. Eur J Clin Microbiol Infect Dis 35, 977–984 (2016). https://doi.org/10.1007/s10096-016-2625-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-016-2625-9