Abstract
Alterations in the intestinal microbial flora have been linked with autoimmune diseases. Our objective was to analyse the composition of the faecal microbiome of children with new-onset juvenile idiopathic arthritis (JIA) compared to healthy controls, and to identify specific gut bacteria associated with JIA. Stool samples from patients were taken at the time of diagnosis of JIA. The microbiome profiles of samples of 30 children with JIA (mean age 6.2 years, 22 girls) were analysed with 16S region-based sequencing profiling and compared to the stool samples of healthy controls (n = 27, mean age 5.4 years, 18 girls). The proportion of bacteria belonging to the phylum Firmicutes was significantly lower in children with JIA [21 % (95 % confident interval [CI]: 17–25 %)] compared to controls [33 % (95 % CI: 26–41 %), p = 0.009]. Bacteria belonging to Bacteroidetes were significantly more abundant in JIA [78 % (95 % CI: 74–82 %)] than in control samples [65 % (95 % CI: 57–73 %), p = 0.008]. Shared operational taxonomic units (OTUs) between the groups revealed that genera Actinobacteria and Fusobacteria were present only in JIA patients and Lentisphaerae only in controls. In summary, faecal flora in JIA is characterised by a low level of Firmicutes and an abundance of Bacteroidetes, resembling the aberration reported in type 1 diabetes. We suggest that alterations in the intestinal microbial flora may challenge the mucosal immune system of genetically susceptible subjects predisposing to local proinflammatory cascades, thus contributing to the development of JIA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The concept of intestinal dysbiosis encompasses alterations in the microbiome, leading to changes in the gut immune system, such as increased permeability and impaired tolerance to environmental and host antigens. There is emerging data that support the presence of intestinal microbial alterations in the pathogenesis of autoimmune disorders, such as inflammatory bowel disease, type 1 diabetes mellitus and rheumatoid arthritis [1–4]. Faecal microbiota in children with type 1 diabetes shows an abundance of Bacteroidetes, loss of Firmicutes and a lack of butyrate-producing bacteria [2, 5]. The onset of rheumatoid arthritis has been associated with increased abundance of Prevotella copri [6] and reduced abundance of Bifidobacterium spp. in faecal flora [7]. Earlier, in the context of intestinal bypass surgery, colonisation of the proximal part of the gut with bacterial flora from the distal gut was shown to lead to the development of seronegative polyarthritis [8].
While the pathogenic mechanism linking the faecal microbiome to the development of autoimmune diseases is still mostly unknown, some animal studies [9, 10] highlight the importance of microbial flora in the maturation of the immune system to identify self and non-self antigens. For example, mice raised in germ-free conditions have a vulnerable mucosal immune system. Introduction of segmented filamentous bacteria to these animals and colonisation in close proximity to the intestinal epithelium, especially in the terminal ileum, leads to an increased proportion of Th17 cells compared to regulatory T cells and, finally, to the autoimmune manifestation of arthritis [11, 12].
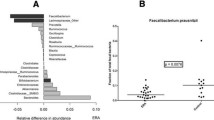
So far, there are only a few studies indicating the presence of intestinal mucosal dysbiosis in juvenile idiopathic arthritis (JIA). Stoll et al. found low representation of Faecalibacterium prausnitzii in faecal flora in children with enthesitis-related arthritis [13]. Malin et al. reported increased urease activity in faecal samples in JIA, and they interpreted this finding as indirect evidence of disturbances in intestinal anaerobic bacterial flora [14]. However, there is clear evidence of functional aberration of the gut mucosa in JIA. Picco et al. found enhanced leakiness of the gut epithelial barrier in children with JIA [15]. In JIA patients suffering from gastrointestinal symptoms [16–18], signs of altered mucosal immunity were observed, such as inflammatory lesions in the gut [18], ileal lymphonodular hyperplasia [16, 17] and HLA-DR expression in abnormal mucosal sites [16]. We also reported an inverse correlation of mucosal anti-inflammatory mediators (IL10, TGFβ, FoxP3) and correlation of massive lymphonodular hyperplasia with JIA disease activity [16]. These studies favour the idea that alterations of both the intestinal immune system and the intestinal microbial flora are involved in the pathogenesis of JIA. Therefore, we characterised the intestinal microbiomes from faecal samples in children with JIA and in healthy control children.
Materials and methods
Study cohort and sample collection
Children with JIA at the Paediatric Rheumatology Outpatient Department of Oulu University Hospital, Finland, were recruited for the study at diagnosis and before initiation of any disease-modifying anti-rheumatic drug (DMARD) or corticosteroid treatment. Stool samples were collected from the JIA patients and the control children between June 2011 and January 2014. The JIA group included 30 children aged from 1 to 15 years, and the control group consisted of 27 children without any autoimmune disease aged from 0 to 14 years. The clinical characteristics of the patients (including the JIA category) and of the controls are presented in Table 1.
The stool samples were collected in vials and stored for a maximum of 2 days at +4 °C. Parents delivered the samples to the outpatient clinic, where they were stored at −80 °C in cryotubes until microbiome analysis. The samples were collected at a time when the study subjects had not recently had any infection or received any antibiotic treatment.
Ethical considerations
Subjects and their parents signed a written informed consent and the protocol was approved by the Ethical Committee for Clinical Science of Oulu University Hospital.
DNA extraction
DNA was extracted from each faecal sample of patients with JIA and healthy children by using the QIAamp DNA Stool Mini Kit, according to the manufacturer’s protocol (Qiagen, USA) and stored at −80 °C until use. The DNA was quantified using a NanoDrop spectrophotometer.
Amplification of bacterial rRNA genes
The hypervariable region V4–V5 of the 16S rRNA gene was amplified using primers F519 and R926. The F519 primer contained an Ion Torrent pyrosequencing adapter sequence A (Life Science Technologies, USA), a 9-bp unique barcode sequence and a nucleotide linker. The R926 primer contained an Ion Torrent adapter trP1 sequence. Polymerase chain reactions (PCRs) were performed in triplicate, each containing 1× Phusion GC buffer, 0.4 μM of forward and reverse primers, 200 μM dNTPs, 0.5 U Phusion enzyme (Thermo Scientific, Finland) and 10 ng genomic community DNA as the template, and molecular-grade water in a total reaction volume of 25 μl. The following cycling conditions were used: 30 cycles of 98 °C, 10 s; 64 °C, 10 s; 72 °C, 20 s, after an initial denaturation of 98 °C, 3 min. After the PCR amplification, pooled triplicate reactions were sequenced using a 316 Chip Kit v2 and Ion Torrent 400 bp chemistry (Life Technologies, USA).
Bioinformatics analysis
The sequences were processed and analysed using state-of-the-art procedures with Quantitative Insights Into Microbial Ecology (QIIME) [19]. Chimeric sequences were removed with UCHIME [20] using the rRNA16S.gold.fasta reference database. The final dataset consisted of 1,574,860 reads after filtering out low-quality and chimeric reads from the 57 samples, with a median of 23,457 reads per sample. The sequences were clustered into operational taxonomic units (OTUs) using a similarity threshold of 97 % in the Ribosomal Database Project (RDP) Naive Bayesian Classifier [20], with a score filtering threshold of 0.5. The OTU table was constructed in a Biological Observation Matrix (BIOM)-formatted table in QIIME, and reads of <5 were removed across the dataset before further analysis. All samples were rarefied to 10,139 sequences prior to the OTU-based analysis, as this was the number of the lowest observed reads in the community. The rarefaction, relative abundance, alpha diversity indices and core microbiome analyses were done with QIIME using a rarefied OTU table. Pie charts were drawn using the Krona software package version 2.4 [21]. Relative abundances of <0.02 % are not shown in the pie charts. The Venn diagram was drawn by the Euler Venn Applet (http://www.cs.kent.ac.uk/people/staff/pjr/EulerVennCircles/EulerVennApplet.html). We have deposited the Ion Torrent raw data in NCBI-SRA with the accession number SRP057688.
Statistical analysis
Statistical analyses were performed with SPSS 20 software (SPSS Inc., Chicago, IL, USA). The Student’s t-test for independent samples or the Mann–Whitney U-test were used, depending on the normality of the distribution, and a p-value < 0.05 was considered to indicate statistical significance. For testing the association of the diversity indexes and clinical characteristics, Pearson’s or Spearman’s correlation tests were used, depending on the type of clinical variable.
Results
Composition of the faecal bacterial community
Among 57 stool samples analysed, there were seven phyla and 55 genera in the full community, and the majority (99 %) of the sequences belonged to the three most abundant phyla: Bacteroidetes (72 %), Firmicutes (27 %) and Proteobacteria (1 %) (Fig. 1). The most noteworthy result was that the abundance of the Bacteroidetes phylum was higher in children with JIA [78 % (95 % confident interval [CI]: 74–82 %)] than in controls [65 % (95 % CI: 57–73 %), p = 0.008]. In contrast, the abundance of Firmicutes was higher in controls [33 % (95 % CI: 26–41 %)] than in JIA children [21 % (95 % CI: 17–25 %), p = 0.009] (Fig. 1). At the family level, Bacteroidaceae (57 % of the Bacteroidetes), Veillonellaceae (7.6 % of the Firmicutes), Ruminococcaceae (7 % of the Firmicutes), Lachnospiraceae (6.3 % of the Firmicutes) and the Rikenellaceae (5.1 % of the Bacteroidetes) were the most common in the whole series of both JIA children and controls.
The relative abundance of gut bacterial flora is shown in control (n = 27) and juvenile idiopathic arthritis (JIA) samples (n = 30). Different taxonomic ranks are represented as circles and distinct taxa as columns, while minor taxa are not shown in the figures. *Less abundant (<1 %) genera are not shown or are combined
At the genus level, Bacteroides (39 %) was the most dominant, followed by B. uniformis (8 %), B. fragilis (5 %), Dialister (4 %), Prevotella copri (4 %), B. ovatus (3 %) and Phascolarctobacterium (2 %). When the JIA patients were compared to the controls, the proportions of the genera Bacteroides (44 vs. 34 %, p = 0.04) were found to differ significantly, but B. uniformis (9 vs. 7 %), B. fragilis (4 vs. 6 %), P. copri (4 vs. 3 %), B. ovatus (2 vs. 4 %) and Dialister (4 vs. 6 %) were found to differ non-significantly between groups (Fig. 1, Table 2).
The OTUs within the two most dominant phyla, Bacteroidetes and Firmicutes, were analysed for low relative abundance of genera among JIA patients and control children (Table 3). Many of the genera in the phylum Bacteroidetes, such as Dysgonomonas and CF231, were present only in control samples. Furthermore, Prevotella and Porphyromonas were present in all samples, irrespective of origin. In the phylum Firmicutes, OTUs of Veillonellaceae, Sarcina, Clostridium butyricum and C. difficile were present only in control samples, whereas members of Megasphaera and Eubacterium biforme were present only in JIA samples. Genera Veillonella, Streptococcus, Coprococcus, Lachnobacterium and Anaerostipes tended to be more abundant in controls than in JIA samples (Table 2).
Comparison of OTUs and the core microbiome between control and JIA samples
To further understand the bacterial distribution within the microbiota, the shared OTUs between the control and JIA samples were analysed (Fig. 2). The control and JIA samples were separated and unique microbiomes were identified for both control and JIA patients, and a Venn diagram was drawn for the shared OTUs. Out of the total 1659 OTUs, 86 and 76 OTUs were unique in control and JIA patients, respectively, and 1497 were shared between them. The bacterial phyla Bacteroidetes, Firmicutes, Proteobacteria and Tenericutes were present in both the controls and the JIA patients, whereas members of Actinobacteria and Fusobacteria were present only in the JIA patients and Lentisphaerae only in the control samples.
The core microbiome analysis for the controls and JIA patients revealed a different view, as there were six and 35 OTUs in the control and JIA samples, respectively, and there were only eight OTUs shared between the groups at the 80 % confidence level (Fig. 3). There was no core microbiome remaining at confidence levels higher than 85 %. The core microbiome of the control samples was dominated by Bacteroides (three OTUs), Lachnospiraceae (two OTUs) and Veillonella (one OTU), and in JIA samples, 30 OTUs of Bacteroides, followed by two OTUs of Oscillospira and one OTU each of Ruminococcus, Veillonella and Blautia, were found. The shared community was dominated by genera Bacteroides (four OTUs), followed by Oscillospira (two OTUs) and one each of Streptococcus and family Rikenellaceae. The rarefaction curves of the faecal microbial diversity of the whole community were constructed and compared between the control and the JIA samples. The diversity of the microbial community tended to be slightly but not significantly higher in the JIA samples compared to the controls (data not shown).
Diversity indexes
We did not find any differences between JIA patients and control children in the diversity index analyses of Chao1 (median in JIA 29.0 vs. controls 28.1, NS), Simpson (median 29.5 vs. 28.4, NS) or Shannon (30.3 vs. 27.5, NS). In the entire study population, there was a correlation between age and the diversity indexes of Chao1 (Pearson’s rho 0.43; p = 0.001) and Shannon (Pearson’s rho 0.34; p = 0.009), but not in the Simpson index (0.18, NS). The correlation was not seen when only the JIA patient group was analysed. In JIA patients, the anti-nuclear antibody titre level correlated inversely with diversity indexes analysed by Spearman’s rho (Simpson −0.43, p = 0.02, Shannon −0.42, p = 0.02 and Chao1 −0.38, p = 0.04).
Discussion
To the best of our knowledge, this is the first report showing that the intestinal microbiome is altered in JIA at the time of diagnosis and before the initiation of DMARDs or corticosteroids. At the phylum level, our JIA patients showed a significantly lower abundance of faecal Firmicutes, but a higher abundance of members of Bacteroidetes, than the control children. The high ratio of Bacteroidetes compared to the Firmicutes phylum in JIA is in accordance with findings in type 1 diabetes mellitus patients [2, 5]. At the genus level, a higher abundance of Bacteroides was found in patients with JIA than in controls, which is also similar to previous findings in type 1 diabetes [2, 3]. Analysis of shared OTUs between the groups revealed that Actinobacteria and Fusobacteria were present only in JIA patients, and Lentisphaerae was present only in control samples. A high abundance of Actinobacteria has also been found in faecal samples of Crohn’s disease patients compared to healthy controls [22]. Finally, in parallel with a recent report from Costello et al. on patients with ankylosing spondylitis [23], OTUs of Veillonellaceae were present only in control samples. Our results indicate that a specific microbial alteration is present in JIA, and that the altered microbiome shares features reported for other autoimmune diseases, including rheumatic diseases.
Our patients with JIA had a low abundance of faecal Firmicutes and a high abundance of members of Bacteroidetes, which was in contrast to the controls. Although the possible mechanism linking this shift with the pathogenesis of JIA remains speculative, the occurrence of a similar microbial shift in type 1 diabetes [2, 5] favours the idea that abnormal immune responses are involved [2]. Several environmental factors may contribute to such a microbial shift [24]. Of the possible dietary factors, consumption of red meat containing haem could modify the Firmicutes/Bacteroidetes ratio in the observed direction [25]. Recently, an association has been found between early exposure to antibiotics, especially clindamycin, and the development of JIA [26, 27]. Of the antimicrobial agents, exposure to clindamycin may lead to loss of Firmicutes and an abundance of the Bacteroidetes phylum in humans [24] and in animal models [28]. In spite of the association of antibiotics with JIA, we did not find an association between low bacterial diversity and JIA. However, the low diversity of Firmicutes has earlier been associated with polyarticular JIA, as presented in a congress abstract [29].
It could be asked whether specific genetic factors of JIA are causally linked to the observed alterations in the intestinal microbial flora. Indeed, HLA-B27-positive rats have shown an increase in abundance of faecal Prevotella spp. and Bacteroides spp. and a decrease in Rikenellaceae compared with wild-type rats [30], which resembles the results in our patients with JIA. However, the observed phylogenic differences between JIA cases and controls could not be explained by HLA-B27, and the effect of HLA-B27 should be tested in a larger series because the rate of HLA-B27 positivity in our JIA patient group (20 %) was almost as low as in the general Finnish population (14 %) [31]. Other HLA classes were not analysed in our JIA series, and, so, the effect of genetic factors on microbial flora [32] cannot be excluded and further studies are needed. There are also reports of geographical differences in faecal microbial composition, such as a higher Firmicutes/Bacteroidetes ratio in children in the USA compared with children in Bangladesh [33]. Therefore, current findings in JIA should be confirmed in other populations.
A healthy mucosal commensal flora induces the mucosal barrier function and prevents excessive antigen-induced activation of the mucosal lymphoid tissues in several ways [34, 35]. Experimentally, these reactions are achieved via optimal stimuli from the luminal commensal bacterial antigens of the toll-like receptors (TLRs), which mediate induction of the synthesis of tight-junction proteins [36] and regulatory T cells [37]. Observations in children with JIA are in line with experimental evidence. In JIA, Picco et al. [15] found intestinal barrier leakiness by using the lactulose-mannitol test. More recently, in JIA patients with gastrointestinal symptoms, we observed evidence of antigen-induced activation of the intestinal mucosa, and in active JIA patients, there was low ileal mRNA levels of anti-inflammatory mediators, such as IL10, TGF-β and FoxP3, simultaneously with low TLR2 [16]. Therefore, we expected to see an alteration in the mucosal flora linked with mucosal barrier function and regulatory T cell function.
In our study, there was a higher abundance of Bacteroides in JIA, but a trend towards low representation of lactic acid-producing bacteria, such as Veillonella, Streptococcus and Aerococcaceae, in JIA patients compared with the controls. This finding is interesting since, in stools from diabetes-prone rats, there was a higher proportion of genera Bacteroides but lower proportions of Lactobacillus than in diabetes-resistant rats [38]. Lactobacillus spp. has been demonstrated to reinforce gut barrier function simultaneously with the induction of intestinal anti-inflammatory cytokine production [39]. The administration of Lactobacillus subspecies was also reported to inhibit the development of experimentally induced arthritis [40, 41] and to alleviate disease activity of rheumatoid arthritis [42].
In conclusion, we found alterations in the faecal microbiome in children with new-onset JIA compared to healthy children. The patterns of the microbiome in JIA show features previously reported in type 1 diabetes, Crohn’s disease and ankylosing spondylitis. We suggest that the observed alterations in the microbiome play a role in the pathogenesis of JIA, as they potentially explain increased mucosal permeability and altered mucosal immunity previously demonstrated in JIA [15–18]. However, more studies are needed in order to confirm these findings in different populations and to dissect the biological mechanisms.
References
Cao Y, Shen J, Ran ZH (2014) Association between Faecalibacterium prausnitzii reduction and inflammatory bowel disease: a meta-analysis and systematic review of the literature. Gastroenterol Res Pract 2014:872725
Giongo A, Gano KA, Crabb DB, Mukherjee N, Novelo LL, Casella G, Drew JC, Ilonen J, Knip M, Hyöty H, Veijola R, Simell T, Simell O, Neu J, Wasserfall CH, Schatz D, Atkinson MA, Triplett EW (2011) Toward defining the autoimmune microbiome for type 1 diabetes. ISME J 5:82–91
Brown CT, Davis-Richardson AG, Giongo A, Gano KA, Crabb DB, Mukherjee N, Casella G, Drew JC, Ilonen J, Knip M, Hyöty H, Veijola R, Simell T, Simell O, Neu J, Wasserfall CH, Schatz D, Atkinson MA, Triplett EW (2011) Gut microbiome metagenomics analysis suggests a functional model for the development of autoimmunity for type 1 diabetes. PLoS One 6:e25792
Scher JU, Sczesnak A, Longman RS, Segata N, Ubeda C, Bielski C, Rostron T, Cerundolo V, Pamer EG, Abramson SB, Huttenhower C, Littman DR (2013) Expansion of intestinal Prevotella copri correlates with enhanced susceptibility to arthritis. Elife 2:e01202
Murri M, Leiva I, Gomez-Zumaquero JM, Tinahones FJ, Cardona F, Soriguer F, Queipo-Ortuño MI (2013) Gut microbiota in children with type 1 diabetes differs from that in healthy children: a case–control study. BMC Med 11:46. doi:10.1186/1741-7015-11-46
Scher JU, Abramson SB (2011) The microbiome and rheumatoid arthritis. Nat Rev Rheumatol 7:569–578
Vaahtovuo J, Munukka E, Korkeamäki M, Luukkainen R, Toivanen P (2008) Fecal microbiota in early rheumatoid arthritis. J Rheumatol 35:1500–1505
Clegg DO, Samuelson CO Jr, Williams HJ, Ward JR (1980) Articular complications of jejunoileal bypass surgery. J Rheumatol 7:65–70
Olszak T, An D, Zeissig S, Vera MP, Richter J, Franke A, Glickman JN, Siebert R, Baron RM, Kasper DL, Blumberg RS (2012) Microbial exposure during early life has persistent effects on natural killer T cell function. Science 336:489–493
Hansen CH, Nielsen DS, Kverka M, Zakostelska Z, Klimesova K, Hudcovic T, Tlaskalova-Hogenova H, Hansen AK (2012) Patterns of early gut colonization shape future immune responses of the host. PLoS One 7:e34043
Ivanov II, Atarashi K, Manel N, Brodie EL, Shima T, Karaoz U, Wei D, Goldfarb KC, Santee CA, Lynch SV, Tanoue T, Imaoka A, Itoh K, Takeda K, Umesaki Y, Honda K, Littman DR (2009) Induction of intestinal Th17 cells by segmented filamentous bacteria. Cell 139:485–498
Wu HJ, Ivanov II, Darce J, Hattori K, Shima T, Umesaki Y, Littman DR, Benoist C, Mathis D (2010) Gut-residing segmented filamentous bacteria drive autoimmune arthritis via T helper 17 cells. Immunity 32:815–827
Stoll ML, Kumar R, Morrow CD, Lefkowitz EJ, Cui X, Genin A, Cron RQ, Elson CO (2014) Altered microbiota associated with abnormal humoral immune responses to commensal organisms in enthesitis-related arthritis. Arthritis Res Ther 16:486. doi:10.1186/s13075-014-0486-0
Malin M, Verronen P, Mykkänen H, Salminen S, Isolauri E (1996) Increased bacterial urease activity in faeces in juvenile chronic arthritis: evidence of altered intestinal microflora? Br J Rheumatol 35:689–694
Picco P, Gattorno M, Marchese N, Vignola S, Sormani MP, Barabino A, Buoncompagni A (2000) Increased gut permeability in juvenile chronic arthritides. A multivariate analysis of the diagnostic parameters. Clin Exp Rheumatol 18:773–778
Arvonen M, Vähäsalo P, Turunen S, Salo HM, Mäki M, Laurila K, Vaarala O, Karttunen TJ (2012) Altered expression of intestinal human leucocyte antigen D-related and immune signalling molecules in juvenile idiopathic arthritis. Clin Exp Immunol 170:266–273
Conti F, Borrelli O, Anania C, Marocchi E, Romeo EF, Paganelli M, Valesini G, Cucchiara S (2005) Chronic intestinal inflammation and seronegative spondyloarthropathy in children. Dig Liver Dis 37:761–767
Mielants H, Veys EM, Cuvelier C, De Vos M, Goemaere S, Maertens M, Joos R (1993) Gut inflammation in children with late onset pauciarticular juvenile chronic arthritis and evolution to adult spondyloarthropathy—a prospective study. J Rheumatol 20:1567–1572
Caporaso JG, Kuczynski J, Stombaugh J, Bittinger K, Bushman FD, Costello EK, Fierer N, Peña AG, Goodrich JK, Gordon JI, Huttley GA, Kelley ST, Knights D, Koenig JE, Ley RE, Lozupone CA, McDonald D, Muegge BD, Pirrung M, Reeder J, Sevinsky JR, Turnbaugh PJ, Walters WA, Widmann J, Yatsunenko T, Zaneveld J, Knight R (2010) QIIME allows analysis of high-throughput community sequencing data. Nat Methods 7:335–336
Edgar RC, Haas BJ, Clemente JC, Quince C, Knight R (2011) UCHIME improves sensitivity and speed of chimera detection. Bioinformatics 27:2194–2200
Ondov BD, Bergman NH, Phillippy AM (2011) Interactive metagenomic visualization in a Web browser. BMC Bioinformatics 12:385. doi:10.1186/1471-2105-12-385
Frank DN, St Amand AL, Feldman RA, Boedeker EC, Harpaz N, Pace NR (2007) Molecular-phylogenetic characterization of microbial community imbalances in human inflammatory bowel diseases. Proc Natl Acad Sci U S A 104:13780–13785
Costello ME, Ciccia F, Willner D, Warrington N, Robinson PC, Gardiner B, Marshall M, Kenna TJ, Triolo G, Brown MA (2014) Intestinal dysbiosis in ankylosing spondylitis. Arthritis Rheumatol 67:686–691
Pérez-Cobas AE, Artacho A, Knecht H, Ferrús ML, Friedrichs A, Ott SJ, Moya A, Latorre A, Gosalbes MJ (2013) Differential effects of antibiotic therapy on the structure and function of human gut microbiota. PLoS One 8:e80201
IJssennagger N, Derrien M, van Doorn GM, Rijnierse A, van den Bogert B, Müller M, Dekker J, Kleerebezem M, van der Meer R (2012) Dietary heme alters microbiota and mucosa of mouse colon without functional changes in host-microbe cross-talk. PLoS One 7:e49868
Horton DB, Scott FI, Haynes K, Putt ME, Rose CD, Lewis JD, Strom BL (2015) Antibiotic exposure and juvenile idiopathic arthritis: a case–control study. Pediatrics 136:e333–e343
Arvonen M, Virta LJ, Pokka T, Kröger L, Vähäsalo P (2015) Repeated exposure to antibiotics in infancy: a predisposing factor for juvenile idiopathic arthritis or a sign of this group’s greater susceptibility to infections? J Rheumatol 42:521–526
Reeves AE, Theriot CM, Bergin IL, Huffnagle GB, Schloss PD, Young VB (2011) The interplay between microbiome dynamics and pathogen dynamics in a murine model of Clostridium difficile infection. Gut Microbes 2:145–158
Hissink Muller PCE, Westedt PM, Budding AE, Allaart CF, Brinkman DMC, Kuijpers TW, van den Berg JM, van Suijlekom-Smit LWA, van Rossum MA, de Meij TG, ten Cate R (2013) Intestinal microbiome in polyarticular juvenile idiopathic arthritis: a pilot study. Pediatr Rheumatol Online J 11(Suppl 2):172
Lin P, Bach M, Asquith M, Lee AY, Akileswaran L, Stauffer P, Davin S, Pan Y, Cambronne ED, Dorris M, Debelius JW, Lauber CL, Ackermann G, Baeza YV, Gill T, Knight R, Colbert RA, Taurog JD, Van Gelder RN, Rosenbaum JT (2014) HLA-B27 and human beta2-microglobulin affect the gut microbiota of transgenic rats. PLoS One 9:e105684
Khan MA (1995) HLA-B27 and its subtypes in world populations. Curr Opin Rheumatol 7:263–269
Gomez A, Luckey D, Yeoman CJ, Marietta EV, Berg Miller ME, Murray JA, White BA, Taneja V (2012) Loss of sex and age driven differences in the gut microbiome characterize arthritis-susceptible 0401 mice but not arthritis-resistant 0402 mice. PLoS One 7:e36095
Lin A, Bik EM, Costello EK, Dethlefsen L, Haque R, Relman DA, Singh U (2013) Distinct distal Gut microbiome diversity and composition in healthy children from Bangladesh and the United States. PLoS One 8:e53838
Kostic AD, Xavier RJ, Gevers D (2014) The microbiome in inflammatory bowel disease: current status and the future ahead. Gastroenterology 146:1489–1499
Brandtzaeg P (2010) Function of mucosa-associated lymphoid tissue in antibody formation. Immunol Investig 39:303–355
Karczewski J, Troost FJ, Konings I, Dekker J, Kleerebezem M, Brummer RJ, Wells JM (2010) Regulation of human epithelial tight junction proteins by Lactobacillus plantarum in vivo and protective effects on the epithelial barrier. Am J Physiol Gastrointest Liver Physiol 298:G851–G859
Round JL, Lee SM, Li J, Tran G, Jabri B, Chatila TA, Mazmanian SK (2011) The Toll-like receptor 2 pathway establishes colonization by a commensal of the human microbiota. Science 332:974–977
Roesch LF, Lorca GL, Casella G, Giongo A, Naranjo A, Pionzio AM, Li N, Mai V, Wasserfall CH, Schatz D, Atkinson MA, Neu J, Triplett EW (2009) Culture-independent identification of gut bacteria correlated with the onset of diabetes in a rat model. ISME J 3:536–548
Martín R, Chain F, Miquel S, Natividad JM, Sokol H, Verdu EF, Langella P, Bermúdez-Humarán LG (2014) Effects in the use of a genetically engineered strain of Lactococcus lactis delivering in situ IL-10 as a therapy to treat low-grade colon inflammation. Hum Vaccin Immunother 10:1611–1621
Kano H, Kaneko T, Kaminogawa S (2002) Oral intake of Lactobacillus delbrueckii subsp. bulgaricus OLL1073R-1 prevents collagen-induced arthritis in mice. J Food Prot 65:153–160
So JS, Kwon HK, Lee CG, Yi HJ, Park JA, Lim SY, Hwang KC, Jeon YH, Im SH (2008) Lactobacillus casei suppresses experimental arthritis by down-regulating T helper 1 effector functions. Mol Immunol 45:2690–2699
Vaghef-Mehrabany E, Alipour B, Homayouni-Rad A, Sharif SK, Asghari-Jafarabadi M, Zavvari S (2014) Probiotic supplementation improves inflammatory status in patients with rheumatoid arthritis. Nutrition 30:430–435
Acknowledgements
The authors thank Dr. Virpi Glumof, PhD and Dr. Tuomo Kokkonen, MD for their useful comments.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Funding Information
Finnish Pediatric Research Foundation Miika Arvonen, Paula Vähäsalo, Mysore V. Tejesvi; Finnish Society of Rheumatology Miika Arvonen; Scandinavian Rheumatology Research Foundation Miika Arvonen; The Finnish Medical Foundation, Paula Vähäsalo; Finnish Cultural Foundation, Paula Vähäsalo; The Alma and K. A. Snellman Foundation, Oulu, Finland, Paula Vähäsalo.
Additional information
M. V. Tejesvi and M. Arvonen contributed equally to this manuscript.
Rights and permissions
About this article
Cite this article
Tejesvi, M.V., Arvonen, M., Kangas, S.M. et al. Faecal microbiome in new-onset juvenile idiopathic arthritis. Eur J Clin Microbiol Infect Dis 35, 363–370 (2016). https://doi.org/10.1007/s10096-015-2548-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-015-2548-x