Abstract
It is uncertain whether an initial inappropriate empirical antibiotic treatment of coagulase-negative staphylococci (CoNS) bacteremia adversely affects the outcome. A retrospective cohort study of CoNS bacteremia was performed at the Dongguk University Ilsan Hospital during a 3-year period. During the study period, 109 patients with CoNS bacteremia were enrolled. The median age of the patients was 72 years and most (96 %, 105/109) had one or more comorbid diseases. Among the participants, 29 % (32/109) received an appropriate empirical antimicrobial therapy. The 30-day mortality was 24 % (26/109) and CoNS bacteremia-related mortality was 14 % (15/109). There was no difference in the CoNS bacteremia-related mortality between the group with an inappropriate empirical treatment (13 %, 10/77) and that with an appropriate treatment (16 %, 5/32) (p = 0.46). In the multivariate analysis using the Cox regression analysis method, Pitt bacteremia scores [hazard ratio (HR) 1.48; 95 % confidence interval (CI) 1.09–2.01; p = 0.01] and retention of eradicable focus (HR 5.0; 95 % CI 1.39–17.9; p = 0.01) were found to be associated with CoNS bacteremia-related mortality. The results suggest that inappropriate empirical therapy might not necessarily be associated with the 30-day mortality or CoNS bacteremia-related mortality. Conversely, Pitt bacteremia scores and retention of eradicable focus were associated with poor outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Coagulase-negative staphylococci (CoNS) are one of the most frequently isolated pathogens in blood cultures and an important cause of nosocomial bloodstream infections [1]. Traditionally, a low virulence has been attributed to CoNS bacteremia, although very few controlled studies have described the related mortality [2, 3]. The treatment recommendations for CoNS bacteremia are supported by scarce evidence, and some experts have proposed that the simple removal of an infected catheter without antimicrobial treatment may be sufficient to resolve bacteremia in some cases [4]. A few reports noted that the use of appropriate empirical antibiotic treatment has a favorable effect on CoNS bacteremia [3], whereas others reported that inappropriate empirical treatment results in no significant difference in outcomes [5]. Therefore, it is uncertain whether the initial inappropriate empirical antibiotic treatment of CoNS bacteremia adversely affects the outcome. In this study, the risk factors influencing the outcome of CoNS bacteremia were evaluated. Furthermore, the effect of inappropriate empirical antibiotic treatment on the outcome of patients with CoNS bacteremia was also determined.
Methods
Study population
This study was conducted at the Dongguk University Ilsan Hospital, a university-affiliated teaching hospital in South Korea which has 600 beds. All adult patients (≥18 years old) with blood cultures positive for CoNS were identified from a retrospective review of the computerized records of the clinical microbiology laboratory between January 2010 and December 2013. This study was approved by the institutional review board of the same hospital (IRB 2013–111). For each patient, only the first episode of CoNS bacteremia was included in the analysis.
Definition and data collection
CoNS was defined by the investigator as a contaminant if it did not meet the previously validated criteria for a significant isolate [6]. In brief, CoNS blood cultures were considered significant if the same CoNS isolate was cultured from >2 bottles at separate time intervals within a 5-day period. In the absence of an alternative diagnosis, the presence of an abnormal neutrophil count (>12 × 109/L with 10 % bands or <2 × 109/L) combined with fever and/or hypotension supported the definition of a significant isolate from a single bottle.
Pertinent clinical data were collected, including age, sex, the source of infection, and underlying comorbidity. Comorbidity was measured by the Charlson comorbidity index, which was calculated by adding the patient’s comorbidity score to their age [7]. The McCabe and Jackson scale was used to measure the severity of diseases 48 h before the index blood sample was obtained for culture [8]. Severity of illness was assessed for each patient at the time of initial documentation of bacteremia using the Pitt bacteremia score [9] and the severity of sepsis [10]. The empirical antimicrobial therapy was considered appropriate if the intravenous therapy given within 48 h of the onset of bacteremia included at least one antibiotic to which the isolate was susceptible [11, 12]. Antimicrobial use was considered inappropriate if an antimicrobial agent to which the isolate was susceptible was not administered within 48 h of onset. Daptomycin was not available in South Korea. The treatment outcomes were assessed 30 days after the onset of CoNS bacteremia according to the following criteria: non-CoNS bacteremia-related mortality (death caused by underlying diseases or another process, with no evidence of CoNS infection at the time of death), CoNS bacteremia-related mortality (death occurred before the resolution of symptoms or signs, or within 7 days of the onset of CoNS bacteremia, in the absence of any other experience) [13].
Foci of bacteremia
In patients with central venous catheter (CVC) lines, catheter-related bloodstream infections (CRBSIs) were defined as follows: (1) the culture of a specimen of purulent drainage from the insertion site grew CoNS that had the same resistance pattern as the culture strain from the peripheral blood; (2) the semiquantitative culture of the removed CVC tip revealed ≥15 colony-forming units by the roll plate technique [14]; (3) indicative differential time to positivity (i.e., the blood culture obtained through an intravascular catheter became positive at least 2 h earlier than a positive simultaneous blood culture obtained from a peripheral vein [15]). Surgical wound infection was defined according to the definitions of the Centers for Disease Control and Prevention (CDC) [16]. If a primary focus of infection could not be determined, it was considered to be unknown. Patients with infective endocarditis were excluded.
The identified foci were further subdivided into eradicable and non-eradicable foci, from which the eradicable foci were further subdivided into eradicated and non-eradicated [11]. Eradicable foci included surgically removable infections or drainable abscesses and indwelling foreign bodies, such as peripheral venous catheters and CVCs.
Blood culture, specimen identification, and susceptibility testing
Blood specimens were collected using aseptic techniques and then inoculated using BACTEC Plus aerobic/F and anaerobic culture vials (BD, Sparks, MD). Blood cultures were processed by the hospital microbiology laboratory using automated BACTEC 9240 (BD) blood culture systems. The identification of CoNS was made using Phoenix PMIC/ID-106 (BD).
Statistical analysis
Statistical analysis was conducted using SPSS for Windows (version 20.0; SPSS Inc., Chicago, IL). Continuous variables were compared by the Mann–Whitney U-test or Student’s t-test, as appropriate. Categorical variables were compared using the Pearson χ2 test or Fisher’s exact test. Independent predictors of 30-day mortality in the cohort study were identified by Cox regression analysis. The time from diagnosis to death was compared using the Kaplan–Meier method and log rank testing.
Results
Patient characteristics
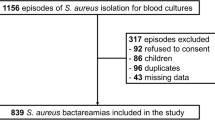
During the study period, a total of 788 CoNS blood cultures were isolated from 618 positive blood culture samples of 488 patients. Of these, 376 patients (77 %) with CoNS bacteremia were classified as contaminated. Among the remaining 112 patients with true CoNS bacteremia, three died before the blood culture results became available. Therefore, 109 patients with true CoNS bacteremia were included in the final analysis (Fig. 1). Only 32 of the 109 (29 %) patients with CoNS bacteremia received initial treatment with the appropriate empirical antibiotics. The median age of the study patients was 72 years [interquartile range (IQR) 54.5–78.0]. Most of the patients (96 %, 105/109) had one or more comorbid diseases. The median Charlson comorbidity index was 7 (IQR 5–9). The clinical characteristics of patients with CoNS bacteremia receiving appropriate empirical antibiotic treatment and those receiving inappropriate treatment are shown in Table 1. Patients who received appropriate empirical antibiotics showed more severe infection in terms of the Pitt bacteremia score than those receiving inappropriate empirical antibiotics. A total of 61 % (67/109) had CVCs at the time when bacteremia was developed (13 % Port-a-Cath, 1.5 % Hickman, 10.4 % hemodialysis tunneled catheters, 11.9 % peripheral inserted central lines, 63.2 % other non-tunneled catheters).
Treatment and outcomes
Of the 77 CoNS bacteremia patients who received inappropriate empirical antibiotic treatment, 67 patients (87 %) received β-lactam ± quinolone (to which the isolated strains were resistant) as an empirical antibiotic treatment within 2 days of the onset of CoNS bacteremia. A further 10 (13 %) patients were given no parenteral antibiotics. Of the 32 CoNS bacteremia patients who received appropriate empirical antibiotic therapy, 27 (84 %) received glycopeptide and 5 (16 %) received β-lactam. Of the 77 patients who received definite treatment after the inappropriate antibiotics, 63 patients were given vancomycin, eight patients β-lactam, and seven teicoplanin. Definite antibiotic treatments (i.e., antibiotics after the susceptibility results) were not different between the inappropriate and appropriate empirical treatment groups. Of the 109 patients with CoNS bacteremia, follow-up blood culture was performed in 76 (70 %) patients, with persistent bacteremia (≥3 days) observed in 32 % (24/76).
The overall 30-day mortality rate was 24 % (26/109). Among the 26 patients who died within 30 days of CoNS bacteremia onset, 11 died due to underlying diseases or infections other than CoNS. In the multivariate analysis using Cox regression, the Pitt bacteremia score [hazard ratio (HR) 1.40; 95 % confidence interval (CI) 1.04–1.88; p = 0.03] and retention of eradicable focus (HR 4.35; 95 % CI 1.64–11.1; p = 0.003) were associated with an increase in the 30-day mortality (Table 2). The survival curves of patients with retention of eradicable focus and removal of eradicated focus are presented in Fig. 2. Table 3 shows the results of the univariate and multivariate analysis of the association of possible risk factors with CoNS bacteremia-related mortality. Inappropriate empirical therapy and persistent bacteremia were not statistically significant.
Subgroup analysis among patients with catheter-related bloodstream infection
Among the 109 patients with CoNS bacteremia, the most common foci of bacteremia was CRBSI 64 (59 %). The CVCs were removed in 67 % (43/64) of cases following diagnosis. A total of 19 (30 %) of the 64 patients died within 30 days after the onset of bacteremia. The CoNS bacteremia-related death rate was 19 % (12/64). Variables associated with CoNS bacteremia-related death are shown in Table 4. In a Cox regression analysis, retention of CVCs and high Pitt bacteremia score were independently associated with mortality.
Discussion
This study evaluated the risk factors for mortality and the impact of inappropriate empirical antimicrobial therapy on the outcomes in patients with CoNS bacteremia. Mortality was not found to be higher in the group with inappropriate empirical treatment compared to the group with appropriate treatment. Retention of eradicable focus and Pitt bacteremia scores were indicated to be strong prognostic factors of 30-day mortality.
Use of appropriate antimicrobial therapy has been shown to reduce mortality in patients with Gram-negative bacteremia and has favorable effects on the outcomes of critically ill patients with bacteremia if initiated early [17]. However, inappropriate empirical therapy in patients with bacteremia caused by Staphylococcus aureus may produce only a negligible increase in mortality [12]. CoNS has been considered more avirulent than S. aureus. Therefore, the result that no relationship was indicated between inappropriate empirical antimicrobial therapy and adverse outcomes is not surprising.
In a recent study, it was found that the absence of inappropriate empirical treatment (p = 0.04) and persistent fever (p = 0.005) were independently associated with mortality in non-critical patients with CoNS bacteremia [3]. That study included only non-critical patients (non-ICU patients), and only 3 % (3/105) presented with severe sepsis or septic shock. However, the present study included 30 % (33/109) ICU patients, and 22 % (24/109) of the patients with CoNS bacteremia presented with severe sepsis or septic shock. That is, the current study showed more severe CoNS bacteremia, which indicates that the severity of illness may dilute the effects of appropriate empirical antibiotic treatments and outcomes.
Our data suggested that an initial delay of 2 days in the use of appropriate antibiotics, especially glycopeptide, prior to a preliminary microbiological report does not adversely affect outcome in patients with CoNS bacteremia. Therefore, our study supports the view that restriction of glycopeptide application could be warranted when empirical antibiotics are used if a patient is stable, not deteriorating rapidly, and has no known risk factors for CoNS infection. A large prospective study is required to confirm these findings.
Acute severity of illness, such as Pitt bacteremia score, was a predictor of poor outcomes in the current study. The Pitt bacteremia score was independently validated by Hill et al. in a study of 424 cases of S. aureus bacteremia [18]. In the present study, 26 % (28/109) of cases presented with a Pitt bacteremia score greater than 2. CoNS bacteremia has traditionally been associated with low virulence, and the need for treatment has even been questioned by clinical guidelines [4]. However, frank sepsis syndrome and fatal outcome may occur, especially in immunocompromised patients and/or if one of the more virulent species, such as S. lugdunensis, is involved [19–21]. Although no cases of S. lugdunensis bacteremia was included in the current study, the study population included severely ill patients, as reflected by the fact that the median Charlson comorbidity index was 7 (IQR 5–9). CoNS bacteremia is rarely life-threatening, especially if treated promptly and adequately. However, it may act as a destabilizing factor in otherwise severely ill patients, as shown in the current study.
Herein, retention of eradicable focus was independently associated with poor outcomes. Several authors emphasized the importance of identifying and treating the focus in the treatment of S. aureus bacteremia [11, 22]. In cases of CoNS bacteremia, Raad et al. reported that CVC retention does not have an impact on the resolution of bacteremia, but is a significant risk factor of recurrence [23]. It is well established that CoNS organisms adhere to the catheter surface through the production of a microbial biofilm [20]. Embedded in this microbial matrix, the CoNS are difficult to eradicate through the use of active agents that are often used in treatment, such as glycopeptide.
This study had some limitations. First, this study was retrospective, observational, and non-randomized. Therefore, it is possible that there were unmeasured confounding factors. The decision of catheter retention or removal is affected by various factors, including the availability of other vascular access, hemodynamic stability for catheter reinsertion, and physician judgment. Second, in this study, the overall mortality rate for patients with CoNS was relatively high (24 %), whereas other studies have reported mortality rates of 14–31 % [2, 3]. This is because many of our patients had other serious underlying conditions, including old age, neurologic diseases, and cancer. This may limit the generalizability of the findings. However, we believe that this phenomenon can be reasonably discarded by multivariate analysis using CoNS bacteremia-related mortality as the secondary outcome. Finally, this study had a limited number of patients and a relatively short duration. Thus, the recurrence or relapse rate of CoNS bacteremia were not obtained. Future research should employ larger data sets and long-term follow-up data.
In conclusion, the results suggest that initial inappropriate empirical therapy may not necessarily be associated with the poor outcomes of CoNS bacteremia. Therefore, our study supported the restriction of glycopeptide use in patients with CoNS bacteremia. However, retention of eradicable focus and Pitt bacteremia scores adversely affected outcome in patients with CoNS bacteremia.
References
Wisplinghoff H, Bischoff T, Tallent SM, Seifert H, Wenzel RP, Edmond MB (2004) Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study. Clin Infect Dis 39(3):309–317
Martin MA, Pfaller MA, Wenzel RP (1989) Coagulase-negative staphylococcal bacteremia. Mortality and hospital stay. Ann Intern Med 110(1):9–16
Molina J, Peñuela I, Lepe JA, Gutiérrez-Pizarraya A, Gómez MJ, García-Cabrera E, Cordero E, Aznar J, Pachón J (2013) Mortality and hospital stay related to coagulase-negative Staphylococci bacteremia in non-critical patients. J Infect 66(2):155–162
Mermel LA, Allon M, Bouza E, Craven DE, Flynn P, O’Grady NP, Raad II, Rijnders BJ, Sherertz RJ, Warren DK (2009) Clinical practice guidelines for the diagnosis and management of intravascular catheter-related infection: 2009 Update by the Infectious Diseases Society of America. Clin Infect Dis 49(1):1–45
Fernández-Rufete A, García-Vázquez E, Hernández-Torres A, Canteras M, Ruiz J, Gómez J (2012) Coagulase-negative Staphylococcus bacteraemia: prognosis factors and influence of antibiotic treatment. Rev Esp Quimioter 25(3):199–205
Beekmann SE, Diekema DJ, Doern GV (2005) Determining the clinical significance of coagulase-negative staphylococci isolated from blood cultures. Infect Control Hosp Epidemiol 26(6):559–566
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383
Jackson GG, Arana-Sialer JA, Andersen Br Grieble HG, McCabe WR (1962) Profiles of pyelonephritis. Arch Intern Med 110:63–75
Paterson DL, Ko WC, von Gottberg A, Mohapatra S, Casellas JM, Goossens H, Mulazimoglu L, Trenholme G, Klugman KP, Bonomo RA, Rice LB, Wagener MM, McCormack JG, Yu VL (2004) International prospective study of Klebsiella pneumoniae bacteremia: implications of extended-spectrum beta-lactamase production in nosocomial Infections. Ann Intern Med 140(1):26–32
Bone RC (1991) Sepsis, the sepsis syndrome, multi-organ failure: a plea for comparable definitions. Ann Intern Med 114(4):332–333
Kim SH, Park WB, Lee KD, Kang CI, Kim HB, Oh MD, Kim EC, Choe KW (2003) Outcome of Staphylococcus aureus bacteremia in patients with eradicable foci versus noneradicable foci. Clin Infect Dis 37(6):794–799
Kim SH, Park WB, Lee KD, Kang CI, Bang JW, Kim HB, Kim EC, Oh MD, Choe KW (2004) Outcome of inappropriate initial antimicrobial treatment in patients with methicillin-resistant Staphylococcus aureus bacteraemia. J Antimicrob Chemother 54(2):489–497
Kim SH, Park WB, Lee CS, Kang CI, Bang JW, Kim HB, Kim NJ, Kim EC, Oh MD, Choe KW (2006) Outcome of inappropriate empirical antibiotic therapy in patients with Staphylococcus aureus bacteraemia: analytical strategy using propensity scores. Clin Microbiol Infect 12(1):13–21
Chatzinikolaou I, Hanna H, Darouiche R, Samonis G, Tarrand J, Raad I (2006) Prospective study of the value of quantitative culture of organisms from blood collected through central venous catheters in differentiating between contamination and bloodstream infection. J Clin Microbiol 44(5):1834–1835
Raad I, Hanna HA, Alakech B, Chatzinikolaou I, Johnson MM, Tarrand J (2004) Differential time to positivity: a useful method for diagnosing catheter-related bloodstream infections. Ann Intern Med 140(1):18–25
Culver DH, Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG, Banerjee SN, Edwards JR, Tolson JS, Henderson TS, Hughes JM (1991) Surgical wound infection rates by wound class, operative procedure, and patient risk index. National Nosocomial Infections Surveillance System. Am J Med 91(3B):152S–157S
Kang CI, Kim SH, Park WB, Lee KD, Kim HB, Kim EC, Oh MD, Choe KW (2005) Bloodstream infections caused by antibiotic-resistant gram-negative bacilli: risk factors for mortality and impact of inappropriate initial antimicrobial therapy on outcome. Antimicrob Agents Chemother 49(2):760–766
Hill PC, Birch M, Chambers S, Drinkovic D, Ellis-Pegler RB, Everts R, Murdoch D, Pottumarthy S, Roberts SA, Swager C, Taylor SL, Thomas MG, Wong CG, Morris AJ (2001) Prospective study of 424 cases of Staphylococcus aureus bacteraemia: determination of factors affecting incidence and mortality. Intern Med J 31(2):97–103
Miele PS, Kogulan PK, Levy CS, Goldstein S, Marcus KA, Smith MA, Rosenthal J, Croxton M, Gill VJ, Lucey DR (2001) Seven cases of surgical native valve endocarditis caused by coagulase-negative staphylococci: an underappreciated disease. Am Heart J 142(4):571–576
von Eiff C, Peters G, Heilmann C (2002) Pathogenesis of infections due to coagulase-negative staphylococci. Lancet Infect Dis 2(11):677–685
Pagano L, Tacconelli E, Tumbarello M, Laurenti L, Ortu-La Barbera E, Antinori A, Caponera S, Cauda R, Leone G (1997) Bacteremia in patients with hematological malignancies. Analysis of risk factors, etiological agents and prognostic indicators. Haematologica 82(4):415–419
Jensen AG, Wachmann CH, Espersen F, Scheibel J, Skinhøj P, Frimodt-Møller N (2002) Treatment and outcome of Staphylococcus aureus bacteremia: a prospective study of 278 cases. Arch Intern Med 162(1):25–32
Raad I, Kassar R, Ghannam D, Chaftari AM, Hachem R, Jiang Y (2009) Management of the catheter in documented catheter-related coagulase-negative staphylococcal bacteremia: remove or retain? Clin Infect Dis 49(8):1187–1194
Acknowledgments
None.
Ethical statements
This manuscript is new, is not being considered elsewhere, and reports new findings. All authors have seen and approved the content and have contributed significantly to the work. This study was approved by the institutional review board of the same hospital (IRB 2013–111).
Conflict of interest
All authors declare no conflicts of interest.
Financial support
This work was supported by the Dongguk University Research Fund 2012.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Park, S.Y., Kwon, K.H., Chung, JW. et al. Coagulase-negative staphylococcal bacteremia: risk factors for mortality and impact of initial appropriate antimicrobial therapy on outcome. Eur J Clin Microbiol Infect Dis 34, 1395–1401 (2015). https://doi.org/10.1007/s10096-015-2364-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-015-2364-3