Abstract
Colonization of the neonatal gut takes place immediately after birth. Bacteria that get colonized are considered to be “normal” flora derived principally from the mother and the immediate environment. However, for some neonates, the colonization of the gut, particularly with potential pathogens, may lead to subsequent infections or sepsis. The immune system and the gut barrier in neonates is vulnerable, with decreased acid secretion, low levels of protective mucous, and decreased motility, particularly in those who are premature and of low birth weight. This makes the neonatal gut especially prone to colonization with aerobic Gram-negative bacilli (GNB). And these GNB may later, under circumstances favorable to them, cause disease in the neonates. In developing countries, it is the GNB that cause the majority of the infections. In addition, the use of antibiotics in the neonatal intensive care unit also triggers colonization with antibiotic-resistant bacteria. This review discusses various aspects of neonatal gut colonization, neonatal sepsis, and tries to gather support to understand the connection between the gut and subsequent sepsis in neonates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The neonatal gut is like a pristine scaffold where microorganisms can establish themselves. For years, the colonization of the gut and its implications were understood in terms of a mutual tolerance between the host and the microbes, and nothing beyond that. However, it has now been proved that bacteria that colonize the gut play a more vital role beyond tolerance in the early development of the newborn [1, 2]. Bacteria that colonize the gut during the early stages is responsible for the immune functioning and development of the intestinal architecture, in addition to providing nutrients, metabolizing indigestible compounds, and defense against colonization by opportunistic pathogens later in life [2].
For most healthy neonates, this colonization is a routine process which occurs without any conscious effort. And bacteria that get colonized are considered to be “normal” flora derived principally from the mother and the immediate environment [3, 4]. However, for sick neonates who require hospitalization for prolonged periods, the colonization of the gut, particularly with potential pathogens, may lead to subsequent infections or sepsis. The immune system and the gut barrier in neonates is vulnerable, with decreased acid secretion, low levels of protective mucous, and decreased motility [5], particularly in those who are premature and of low birth weight. This makes the neonatal gut especially prone to colonization with aerobic Gram-negative bacilli (GNB). And these GNB may later, under circumstances favorable to them, cause disease in the neonates. Studies have shown that the GNB in the gut may predispose the neonates to septicemia [6, 7]. Evidence from surgical neonates shows that gut overgrowth, particularly with GNB, causes depression of the mucosal and systemic immunity, leading to the development of sepsis [8].
Evidence from earlier research and that from our laboratory show that there is a direct or indirect association between the gut microflora and sepsis. This review tries to gather support to understand the connection between the gut and subsequent sepsis in neonates.
A reality: neonatal sepsis
What is sepsis?
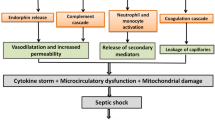
Sepsis is a clinical syndrome characterized by a whole-body inflammatory state (called a systemic inflammatory response syndrome or SIRS) that is triggered by an infection [9, 10]. The body may develop this response to microbes in the blood, urine, lungs, skin, or other tissues. Neonatal sepsis (NS) refers to the above described condition occurring in the first month of life, which is called the neonatal period.
How big is the problem?
Of all infections that occur in neonates, sepsis is a devastating complication and a major cause of morbidity and mortality in the newborn [11]. The World Health Organization (WHO) estimates that one million deaths occur per year due to NS, and 42 % of these deaths occur in the first week of life [12, 13]. Most deaths occur in the developing countries [11], due to the disparity in the neonatal care and hygiene conditions in the developed and developing countries.
Which organisms cause sepsis?
Sepsis can be caused by a diverse repertoire of organisms, and the list seems to be ever-growing. Organisms that cause NS are acquired shortly before, during, and after birth [12]. Furthermore, different trends are observed at different geographic locations. The pathogens most often implicated in NS in developing countries differ from those seen in developed countries. Group B Streptococcus is the most common cause of NS in developed countries and rare in developing countries [14–16]. Again, in low-income countries, Gram-negative organisms mainly represented by Klebsiella sp., Escherichia coli, Pseudomonas, Acinetobacter sp. [17, 18], and Gram-positive cocci, Staphylococcus aureus, and Staphylococcus epidermis are the predominant causative agents [18]. A study carried out by our group reviewing the etiological agents of NS raised concern about the emergence of non-fermenting GNB in sepsis [19, 20].
Conventionally, early-onset sepsis (EOS) is considered to be predominantly maternally acquired and organisms causing EOS have lower chances of being drug-resistant compared to late-onset sepsis (LOS), which is considered to be of environmental origin. However, in resource-poor settings, the unhygienic labor rooms and failure to adhere to aseptic techniques allow transmission of pathogens. Zaidi et al. [21] clearly state that any infection in a hospital-born baby in a low-income country should be considered to be potentially hospital-acquired, even if the onset is within the first few days of life. In congruence with this, other studies carried out in our unit have shown that multidrug-resistant organisms do cause EOS [22].
A gutful of bacteria
Which organisms colonize the neonatal gut?
Classical studies revealed that the gut microbiota very early in life has a higher proportion of facultative bacteria than the adult microbiota [23]. Facultative bacteria dominate the first flora as the abundance of oxygen in the neonatal gut prevents expansion of obligate anaerobes. E. coli and enterococci (E. faecalis and E. faecium) have been identified as the first infant colonizers in some studies [24, 25]. Other Enterobacteriaceae, such as Klebsiella and Enterobacter, are also common in the gut flora of neonates [26, 27]. Other studies have shown that, in addition to GNB, alpha-hemolytic streptococci seem to colonize 20–30 % of neonates [28].
The establishment of facultative anaerobes in the intestinal tract initially decreases the redox potential in the gut lumen, creating a reduced environment that favors the establishment of obligate anaerobes. Bifidobacterium, Bacteroides, and Clostridium sp. were isolated from at least half of the investigated infants in the first week of life at ≤1011 colony-forming units (CFU)/g feces [23–25].
Which factors affect colonization?
The dynamic nature of the gut ecosystem is undisputed. A number of factors influence colonization, particularly during the period of life when this ecosystem is being established. The mode of delivery influences colonization [29]. Vaginally delivered neonates are colonized first with maternal fecal and vaginal flora, whereas neonates delivered by caesarean section get colonized with bacteria originating from the hospital milieu. The feeding pattern of the baby does influence the colonization, but not to the extent as it was claimed to be earlier [23]. In fact, bifidobacteria are found equally often and in similar counts in breast- and formula-fed infants. Differences occur in the case of clostridia [29, 30], which is more common and reach higher counts in formula-fed infants. The environment has a striking affect on the flora. Neonates cared for in the intensive care unit (ICU), where antibiotic use is frequent, tend to acquire antibiotic-resistant and nosocomial pathogens. The sanitary conditions in overcrowded hospitals in resource-poor settings also lead to colonization of the gut with hospital-mediated pathogens.
Studies assessing the risk factors for colonization of the neonatal gut with GNB showed that, immediately after birth, maternal risk factors affected colonization and, later, stay in the neonatal ICU and prolonged feeding by an enteral feeding tube were independent risk factors for the occurrence of GNB [27, 31]. This suggests that, while immediately after birth maternal risk factors are important, the chance of infection from the environment becomes the more important factor as exposure to the hospital environment increases.
Infection en route the gut
Beneficial bacteria and pathogens in the gut
All bacteria that colonize the gut are not beneficial; some are potential pathogens. And the gut can be considered an intelligent organ because of its ability to distinguish between the beneficial and the pathogenic bacteria. This ability to distinguish the good from the bad is a seminal role of the gut mucosal surface.
For the majority of neonates who are well and leave the hospital quickly, there is little opportunity to acquire nosocomial pathogens. However, for the sick neonates, the situation is different. The severity of illness is directly proportional to the length of stay in the hospital and ensuing colonization of the gut with nosocomial pathogens. As discussed earlier, the abundance of oxygen in the neonatal gut allows colonization with facultative anaerobes. But, unlike healthy babies, neonates in the ICU get colonized with pathogens like Klebsiella and Enterobacter, along with E. coli [4, 31]. Studies from our laboratory have also shown that K. pneumoniae was the most common GNB detected in the fecal specimens and gastric aspirates of hospitalized neonates, followed by E. coli (Table 1) [27]. In fact, the presence of K. pneumoniae in the gastric aspirates was significantly higher than E. coli [27].
Establishing the gut connection with neonatal sepsis
The idea that the gastrointestinal tract, teeming with its own bacterial flora, could represent a source of sepsis under certain conditions has interested clinicians for many years. Studies have shown an association between the upper gastrointestinal microflora and subsequent septic complications [32, 33]. Evidence from surgical neonates shows that gut overgrowth, particularly with GNB, causes depression of the mucosal and systemic immunity, leading to the development of sepsis [6, 8], or at least the presence of GNB in the gut has been shown in clinical studies to predispose the neonates to sepsis [6, 7]. The premature infant has lower gastric acid production, lower levels of protective mucus, decreased motility, lower levels of B and T lymphocytes, and lower levels of secretory immunoglobulin A (IgA), all of which are factors that increase bacterial adherence to the intestinal mucosa and susceptibility to infection [5]. The immature gastrointestinal barrier and immune response might, thus, make the neonates more susceptible to sepsis thereof.
A review of the literature showed that studies focused on neonates dealt with those who have undergone surgical procedures. Parenteral nutrition given to surgical patients cause immunosuppression due to atrophy of the small intestinal gut-associated lymphoid tissue [34] and decreased IgA levels. In addition, parenteral nutrition impairs gut motility. A combination of these factors leads to intestinal overgrowth. The endotoxin produced by the bacteria in the gut causes suppression of systemic immunity via liver dysfunction [35], leading to the development of sepsis and septicemia. Previous work has shown that sepsis and septicemia rates were significantly higher in surgical infants (receiving parenteral nutrition) with carriage of aerobic GNB. The carriage precedes sepsis and septicemia, lending proof to the fact that gut overgrowth with abnormal GNB contributes to septic morbidity [6].
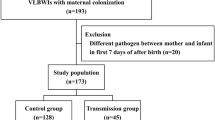
In developing countries like India, NS occurs in a large number of neonates without any surgical intervention. We carried out a study among nonsurgical neonates in a tertiary care hospital in India to find out the association of GNB in the gut and subsequent sepsis in the neonates [27]. K. pneumoniae was found to be not only the predominant organism that colonized the neonatal gut, but also the most common organism isolated from the neonatal blood specimens (Tables 1 and 2). Further, neonates with GNB in the gut had consistently higher incidence of clinical sepsis than those without GNB in the gut. In 50 % of cases, the genotypes of the organisms found in the blood were indistinguishable from their gut counterpart. The representation of organisms like K. pneumoniae, E. coli, and E. cloacae in the gut and blood and not Burkholderia cepacia (not a intestinal colonizer) also suggested a relationship between factors impacting intestinal colonization by GNB and subsequent sepsis.
A few recent studies have also established the link between gut colonization and sepsis using culture-dependent and -independent methods. A study has shown that the neonatal gut harbors sepsis-causing pathogens and gut colonization precedes the onset of sepsis [36]. In another study, the authors noted a difference in the colonizing bacteria between the healthy premature neonates and those that developed sepsis [37].
Studies on sepsis and its relationship with the gut can give us some clues about the mechanism by which the gut flora can cause sepsis. One mechanism could be bacterial translocation (Fig. 1). “Bacterial translocation” is used to describe the passage of viable resident bacteria from the gastrointestinal tract to normally sterile tissues, such as the mesenteric lymph nodes and other internal organs [38, 39]. There is increasing circumstantial evidence to suggest that this translocation of bacteria from the gut may play an important role in the causation of sepsis. One particular study showed that endogenous septicemias due to microbial translocation are clinically relevant in neonates [7]. Some studies in animal models or by in vitro techniques have also shown that bacterial translocation takes place particularly in the immature gut [40].
Mechanisms of bacterial translocation in the small intestine. Multiple pathways, receptors, and cells are involved in bacterial translocation from the intestinal lumen. Toxins such as flagellin, endotoxins, exotoxins, and other bacterial products can disrupt tight junctions and facilitate paracellular translocation of bacteria between intestinal epithelial cells. Transcellular translocation of bacteria can occur via receptors including intelectin [also lactoferrin receptor], type III secretory system, Toll-like receptors, LFA-1 [lectin] receptor, β1 integrin, and IgA displayed on M cells. Bacterial uptake through these cells can result in systemic dissemination of the microbe. Reprinted from Clinical Perinatology (Sherman, 2010) with the permission of the publisher [39]
A number of organisms, particularly the GNB, are known to translocate [38, 41]. Some organisms are obvious pathogens, like Shigella sp. and Salmonella sp., which possess virulence determinants that provide them with the potential to cause disease. Salmonella sp. or Shigella sp. or enteroinvasive E. coli can invade the epithelial barrier in the gut and cause disease [42]. However, the idea that the “enteric bacterial community” plays a role in bacterial translocation is emerging. This is evidenced by a study showing Campylobacter jejuni assisting commensal bacteria to cross gut epithelia using lipid rafts [43].
Apart from the direct translocation of GNB in the gut to the bloodstream, the organisms in the gut can also indirectly affect systems that cause sepsis. One such method of transfer of the gut flora to the blood could be via the trachea. Poor acidity and poor peristaltic movements might lead to the subsequent transmission of GNB from the stomach to the trachea and cause sepsis. A study by Schwartz et al. has shown that, at least in the case of Enterobacteriaceae, the colonization of the gut occurred prior to the colonization of the trachea [44]. There is another method in which the gut flora of one individual can participate in causing sepsis to others. Babies with GNB in their gut can act as carriers and spread infection to others. It is known that carriers increase colonization pressure and the number of patients shedding bacteria increases the risk of infection for another patient [45]. In the environment of the neonatal ICU, there are neonates busily excreting billions of GNB all throughout the day. And in the frantic atmosphere of an ICU, staff do occasionally forget to wash hands and can act as carriers [4]. The modes of transmission of bacteria from the gut to the bloodstream may be different, but the involvement of the gut bacteria in sepsis cannot be ignored.
A more powerful blow to the gut: antibiotic-resistant organisms
ICUs are one of those places where resistance to antimicrobials is more common because of the fact that antimicrobials are used there with the greatest frequency. The intestinal tract provides an important reservoir for antibiotic-resistant GNB [46, 47]. The neonate whose sickness binds him/her within the walls of the ICU easily gets colonized with antibiotic-resistant bacteria [31]. Although many neonates may remain asymptomatic [48], infection can occur because of translocation or a colonized neonate may act as a carrier. To add fuel to the fire, the gut provides an important site for the transfer of genes conferring antibiotic resistance [49, 50]. So, the “normal” flora may also acquire resistance genes and participate in causing disease.
Many of the resistance genes are present on promiscuous plasmids [51, 52] and it does not take long before you have an infection, followed by an outbreak. A number of outbreaks in the neonatal ICU have been reported which have been caused by Enterobacteriaceae [53, 54] or other GNBs like A. baumannii [55, 56]. One particular study showed that drug-resistant Enterobacteriaceae found at high frequency in infants during their stay in the neonatal ICU persisted in a proportion of infants after their discharge from the hospital [57]. The problem of resistance is compounded because GNB are often resistant to multiple classes of antibiotics. The use of many different antibiotics may facilitate colonization and dissemination of these pathogens. For example, the metallo-β-lactamases like IMP-1 or VIM-1 are resistant to carbapenems, aminoglycosides, third-generation cephalosporins, and ciprofloxacins [58].
Repairing the gut, preparing the future: probiotics
In 1907, Nobel laureate Elie Metchnikoff proposed the beneficial role of probiotics [59]. Probiotics not only provide a physical barrier against colonization by pathogenic bacteria, but some of the metabolic products of probiotic bacteria (e.g., lactic acid and a class of antibiotic proteins termed bacteriocins, produced by some bacteria) inhibit growth of pathogenic organisms. Also, the desirable bacteria may compete for nutrients with the pathogens. There is also some evidence that probiotic bacteria may enhance the gut immune response against pathogenic bacteria [60].
Any modulation in the colonizing flora will have possible consequences on neonatal infections, as most infections during this period are routed through the gut. Research shows that the emergence of lactic acid bacteria and bifidobacteria in the bowel prevents bacterial translocation. The supplementation of preterm infants with Bifidobacterium lactis increased the number of bifidobacteria, while the numbers of enterobacteria and clostridia, which include many potential pathogens, were reduced. However, the supplementation did not reduce the fecal reservoir of antibiotic-resistant bacteria [61, 62]. Studies in newborns have also demonstrated that there was a reduction in the incidence of necrotizing enterocolitis on administration of probiotics [63]. Beneficial in vivo effects of probiotics in neonates are reportedly related to more competent gut-related immunity, a less pathogenic intestinal flora, and diminished intraluminal microbial toxins [39, 64]. All evidence, thus, indicates that probiotics in neonates would be valuable and would reduce infections. With the limitation in therapeutic choice to treat sepsis due to increasing antibiotic resistance, prevention could be a very good option. However, more studies would be necessary before probiotics can be routinely used in neonates.
Lessons learnt
Nature does not undertake futile exercises. The flora that resides in the gut has obvious purposes. However, the balance between the benefit and the compromise sometimes becomes skewed in such an arrangement, leading to disease. During the initial stages of life when the partnership between the flora and the gut mucosa is being built, pathogens increase the chances of infection. The problem is compounded with antibiotic-resistant organisms, which are prevalent in the hospital milieu. It is important, at this stage, to provide the right environment and diet to the gut, as it will impact life subsequently. Also vital is the realization that bacteria in the gut need to be regularly monitored, particularly in hospitalized patients. The impact of the microflora necessitates further studies to improve our understanding of how the partnership is formed, is sustained, and how, in disease, it gets imbalanced in neonates. Newer techniques in genomics will probably be able to provide answers regarding the interaction of the microbial community and the gut, and the process in which gut–derived sepsis occurs.
References
Wilks M (2007) Bacteria and early human development. Early Hum Dev 83:165–170
Round JL, Mazmanian SK (2009) The gut microbiota shapes intestinal immune responses during health and disease. Nat Rev Immunol 9:313–323
Rennie JM (2005) Roberton’s textbook of neonatology, 4th edn). Churchill Livingstone, Edinburgh
Goldmann DA (1981) Bacterial colonization and infection in the neonate. Am J Med 70:417–422
Udall JN Jr (1990) Gastrointestinal host defense and necrotizing enterocolitis. J Pediatr 117:S33–S43
van Saene HK, Taylor N, Donnell SC, Glynn J, Magnall VL, Okada Y, Klein NJ, Pierro A, Lloyd DA (2003) Gut overgrowth with abnormal flora: the missing link in parenteral nutrition-related sepsis in surgical neonates. Eur J Clin Nutr 57:548–553
Pierro A, van Saene HKF, Jones MO, Brown D, Nunn AJ, Lloyd DA (1998) Clinical impact of abnormal gut flora in infants receiving parenteral nutrition. Ann Surg 227:547–552
Donnell SC, Taylor N, van Saene HK, Magnall VL, Pierro A, Lloyd DA (2002) Infection rates in surgical neonates and infants receiving parenteral nutrition: a five-year prospective study. J Hosp Infect 52:273–280
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G; SCCM/ESICM/ACCP/ATS/SIS (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med 31:1250–1256
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 101:1644–1655
Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, Jha P, Campbell H, Walker CF, Cibulskis R, Eisele T, Liu L, Mathers C; Child Health Epidemiology Reference Group of WHO and UNICEF (2010) Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet 375:1969–1987
Edmond K, Zaidi A (2010) New approaches to preventing, diagnosing, and treating neonatal sepsis. PLoS Med 7:e1000213
Lawn JE, Cousens S, Zupan J; Lancet Neonatal Survival Steering Team (2005) 4 million neonatal deaths: when? Where? Why? Lancet 365:891–900
Vergnano S, Sharland M, Kazembe P, Mwansambo C, Heath PT (2005) Neonatal sepsis: an international perspective. Arch Dis Child Fetal Neonatal Ed 90:F220–F224
Kuruvilla KA, Thomas N, Jesudasan MV, Jana AK (1999) Neonatal Group B Streptococcal bacteraemia in India: ten years’ experience. Acta Paediatr 88:1031–1032
Tan KW, Tay L, Lin R, Daniel M, Bhavani S, Lim SH (1998) Group B Streptococcal septicaemia/meningitis in neonates in a Singapore teaching hospital. Aust N Z J Obstet Gynaecol 38:418–423
Zaidi AKM, Thaver D, Ali SA, Khan TA (2009) Pathogens associated with sepsis in newborns and young infants in developing countries. Pediatr Infect Dis J 28:S10–S18
Karthikeyan G, Premkumar K (2001) Neonatal sepsis: Staphylococcus aureus as the predominant pathogen. Indian J Pediatr 68:715–717
Viswanathan R, Singh AK, Mukherjee S, Mukherjee R, Das P, Basu S (2011) Aetiology and antimicrobial resistance of neonatal sepsis at a tertiary care centre in eastern India: a 3 year study. Indian J Pediatr 78:409–412
Viswanathan R, Singh AK, Basu S, Chatterjee S, Roy S, Isaacs D (2014) Multi-drug-resistant, non-fermenting, gram-negative bacilli in neonatal sepsis in Kolkata, India: a 4-year study. Paediatr Int Child Health 34:56–59
Zaidi AKM, Huskins WC, Thaver D, Bhutta ZA, Abbas Z, Goldmann DA (2005) Hospital-acquired neonatal infections in developing countries. Lancet 365:1175–1188
Viswanathan R, Singh AK, Basu S, Chatterjee S, Sardar S, Isaacs D (2012) Multi-drug resistant gram negative bacilli causing early neonatal sepsis in India. Arch Dis Child Fetal Neonatal Ed 97:F182–F187
Adlerberth I, Wold AE (2009) Establishment of the gut microbiota in Western infants. Acta Paediatr 98:229–238
Mata LJ, Urrutia JJ (1971) Intestinal colonization of breast-fed children in a rural area of low socio-economic level. Ann N Y Acad Sci 176:93–109
Stark PL, Lee A (1982) The microbial ecology of the large bowel of breast-fed and formula-fed infants during the first year of life. J Med Microbiol 15:189–203
Adlerberth I, Hanson LA, Wold AE (1999) The ontogeny of the intestinal flora. In: Sanderson IR, Walker WA (eds) Development of the gastrointestinal tract. BC Decker, Ontario, pp 279–292
Das P, Singh AK, Pal T, Dasgupta S, Ramamurthy T, Basu S (2011) Colonization of the gut with Gram-negative bacilli, its association with neonatal sepsis and its clinical relevance in a developing country. J Med Microbiol 60:1651–1660
Benno Y, Sawada K, Mitsuoka T (1984) The intestinal microflora of infants: composition of fecal flora in breast-fed and bottle-fed infants. Microbiol Immunol 28:975–986
Penders J, Thijs C, Vink C, Stelma FF, Snijders B, Kummeling I, van den Brandt PA, Stobberingh EE (2006) Factors influencing the composition of the intestinal microbiota in early infancy. Pediatrics 118:511–521
Tullus K, Aronsson B, Marcus S, Möllby R (1989) Intestinal colonization with clostridium difficile in infants up to 18 months of age. Eur J Clin Microbiol Infect Dis 8:390–393
Nordberg V, Quizhpe Peralta A, Galindo T, Turlej-Rogacka A, Iversen A, Giske CG, Navér L (2013) High proportion of intestinal colonization with successful epidemic clones of ESBL-producing Enterobacteriaceae in a neonatal intensive care unit in Ecuador. PLoS One 8(10):e76597
Marshall JC, Christou NV, Horn R, Meakins JL (1988) The microbiology of multiple organ failure. The proximal gastrointestinal tract as an occult reservoir of pathogens. Arch Surg 123:309–315
Marshall JC, Christou NV, Meakins JL (1993) The gastrointestinal tract. The “undrained abscess” of multiple organ failure. Ann Surg 218:111–119
Li J, Kudsk KA, Gocinski B, Dent D, Glezer J, Langkamp-Henken B (1995) Effects of parenteral and enteral nutrition on gut-associated lymphoid tissue. J Trauma 39:44–51
Billiar TR, Maddaus MA, West MA, Curran RD, Wells CA, Simmons RL (1988) Intestinal gram-negative bacterial overgrowth in vivo augments the in vitro response of Kupffer cells to endotoxin. Ann Surg 208:532–540
Carl MA, Ndao IM, Springman AC, Manning SD, Johnson JR, Johnston BD, Burnham CA, Weinstock ES, Weinstock GM, Wylie TN, Mitreva M, Abubucker S, Zhou Y, Stevens HJ, Hall-Moore C, Julian S, Shaikh N, Warner BB, Tarr PI (2014) Sepsis from the gut: the enteric habitat of bacteria that cause late-onset neonatal bloodstream infections. Clin Infect Dis 58(9):1211–1218
Madan JC, Salari RC, Saxena D, Davidson L, O’Toole GA, Moore JH, Sogin ML, Foster JA, Edwards WH, Palumbo P, Hibberd PL (2012) Gut microbial colonisation in premature neonates predicts neonatal sepsis. Arch Dis Child Fetal Neonatal 97(6):F456–F462
Berg RD (1995) Bacterial translocation from the gastrointestinal tract. Trends Microbiol 3:149–154
Sherman MP (2010) New concepts of microbial translocation in the neonatal intestine: mechanisms and prevention. Clin Perinatol 37:565–579
Duffy LC (2000) Interactions mediating bacterial translocation in the immature intestine. J Nutr 130(2S Suppl):432S–436S
MacFie J, O’Boyle C, Mitchell CJ, Buckley PM, Johnstone D, Sudworth P (1999) Gut origin of sepsis: a prospective study investigating associations between bacterial translocation, gastric microflora, and septic morbidity. Gut 45:223–228
Cossart P, Sansonetti PJ (2004) Bacterial invasion: the paradigms of enteroinvasive pathogens. Science 304:242–248
Kalischuk LD, Inglis GD, Buret AG (2009) Campylobacter jejuni induces transcellular translocation of commensal bacteria via lipid rafts. Gut Pathog 1:2
Schwartz SN, Dowling JN, Benkovic C, DeQuittner-Buchanan M, Prostko T, Yee RB (1978) Sources of gram-negative bacilli colonizing the tracheae of intubated patients. J Infect Dis 138:227–231
Bonten MJ, Slaughter S, Ambergen AW, Hayden MK, van Voorhis J, Nathan C, Weinstein RA (1998) The role of “colonization pressure” in the spread of vancomycin-resistant enterococci: an important infection control variable. Arch Intern Med 158:1127–1132
Donskey CJ (2004) The role of the intestinal tract as a reservoir and source for transmission of nosocomial pathogens. Clin Infect Dis 39:219–226
Donskey CJ (2006) Antibiotic regimens and intestinal colonization with antibiotic-resistant gram-negative bacilli. Clin Infect Dis 43:S62–S69
Roy S, Viswanathan R, Singh A, Das P, Basu S (2010) Gut colonization by multidrug-resistant and carbapenem-resistant Acinetobacter baumannii in neonates. Eur J Clin Microbiol Infect Dis 29:1495–1500
Ley RE, Hamady M, Lozupone C, Turnbaugh PJ, Ramey RR, Bircher JS, Schlegel ML, Tucker TA, Schrenzel MD, Knight R, Gordon JI (2008) Evolution of mammals and their gut microbes. Science 320:1647–1651
Salyers AA, Gupta A, Wang Y (2004) Human intestinal bacteria as reservoirs for antibiotic resistance genes. Trends Microbiol 12:412–416
Bockstael K, Van Aerschot A (2009) Antimicrobial resistance in bacteria. Cent Eur J Med 4:141–155
Nikaido H (2009) Multidrug resistance in bacteria. Annu Rev Biochem 78:119–146
Randrianirina F, Vedy S, Rakotovao D, Ramarokoto CE, Ratsitohaina H, Carod JF, Ratsima E, Morillon M, Talarmin A (2009) Role of contaminated aspiration tubes in nosocomial outbreak of Klebsiella pneumoniae producing SHV-2 and CTX-M-15 extended-spectrum β-lactamases. J Hosp Infect 72:23–29
Oteo J, Cercenado E, Fernández-Romero S, Saéz D, Padilla B, Zamora E, Cuevas O, Bautista V, Campos J (2012) Extended-spectrum-β-lactamase-producing Escherichia coli as a cause of pediatric infections: report of a neonatal intensive care unit outbreak due to a CTX-M-14-producing strain. Antimicrob Agents Chemother 56:54–58
Villegas MV, Hartstein AI (2003) Acinetobacter outbreaks, 1977–2000. Infect Control Hosp Epidemiol 24:284–295
Touati A, Achour W, Cherif A, Hmida HB, Afif FB, Jabnoun S, Khrouf N, Hassen AB (2009) Outbreak of Acinetobacter baumannii in a neonatal intensive care unit: antimicrobial susceptibility and genotyping analysis. Ann Epidemiol 19:372–378
Millar M, Philpott A, Wilks M, Whiley A, Warwick S, Hennessy E, Coen P, Kempley S, Stacey F, Costeloe K (2008) Colonization and persistence of antibiotic-resistant Enterobacteriaceae strains in infants nursed in two neonatal intensive care units in East London, United Kingdom. J Clin Microbiol 46:560–567
Queenan AM, Bush K (2007) Carbapenemases: the versatile β-lactamases. Clin Microbiol Rev 20:440–458
Shortt C (1999) The probiotic century: historical and current perspectives. Trends Food Sci Technol 10:411–417
Calder PC, Kew S (2002) The immune system: a target for functional foods? Br J Nutr 88:S165–S177
Mohan R, Koebnick C, Schildt J, Schmidt S, Mueller M, Possner M, Radke M, Blaut M (2006) Effects of Bifidobacterium lactis Bb12 supplementation on intestinal microbiota of preterm infants: a double-blind, placebo-controlled, randomized study. J Clin Microbiol 44:4025–4031
Lee SJ, Cho SJ, Park EA (2007) Effects of probiotics on enteric flora and feeding tolerance in preterm infants. Neonatology 91:174–179
Deshpande G, Rao S, Patole S, Bulsara M (2010) Updated meta-analysis of probiotics for preventing necrotizing enterocolitis in preterm neonates. Pediatrics 125:921–930
Hunter CJ, Upperman JS, Ford HR, Camerini V (2008) Understanding the susceptibility of the premature infant to necrotizing enterocolitis (NEC). Pediatr Res 63:117–123
Conflict of interest
The author declares that she has no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Basu, S. Neonatal sepsis: the gut connection. Eur J Clin Microbiol Infect Dis 34, 215–222 (2015). https://doi.org/10.1007/s10096-014-2232-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-014-2232-6