Abstract
The objectives of this investigation were to study the temporal trends in hospitalizations of patients with sepsis in the Region of Madrid (Spain) from 2003 to 2011 and analyze the factors associated with inpatient mortality. All sepsis hospitalizations from the minimum basic data set (MBDS) during 2003 to 2011 in the Region of Madrid were analyzed. Gender-specific crude and age-adjusted rates were calculated each year. Factors associated with death in these patients were studied with bivariate and multivariate analyses. Simultaneously, sepsis inpatients also underwent descriptive analysis. The study included 98,898 sepsis episodes. The incidence of sepsis hospitalizations per 100,000 habitants increased in males from 114.4 in 2003 to 262.2 in 2011, and in females from 91.2 to 209.1 between 2003 and 2011. The observed inpatient mortality was 23.2 %. There were 45,936 (46.4 %) episodes of severe sepsis (≥1 organ failure), revealing a clear upward trend, especially in multi-organ failure. Severe sepsis mortality showed a decreasing trend in both males (40.0 to 31.8 % from 2003 through 2011) and females (41.6 to 35.2 % from 2003 through 2011). Death was most frequent among the elderly and in patients with more organ failures and comorbidities. In a populous region of Southern Europe, an upward trend in sepsis incidence was observed between 2003 and 2011, as well as a decreasing trend in mortality for sepsis inpatients. Mortality increased with age, comorbidities, and organ failures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sepsis is defined as systemic inflammatory response syndrome (SIRS) of infectious origin. Sepsis diagnosis requires the presence of both infection and a systemic inflammatory response [1]. One or more organ systems failure or the occurrence of hypoperfusion in conjunction with sepsis is considered to be severe sepsis. Septic shock is defined as severe sepsis accompanied with hypotension [2].
It has been estimated that up to 18 million cases of sepsis occur every year, with an approximate mortality of 30 %; therefore, it is considered a major cause of mortality worldwide [3]. In the United States, the overall incidence of sepsis is approximately 300 cases/100,000 inhabitants/year and 226 cases per 100,000 hospital discharges [4]. Nationally reported epidemiological incidence rates for severe sepsis consistently lie between 50 and 100 cases per 100,000 persons in industrialized countries [5].
Sepsis incidence and mortality have increased over the course of several decades [6, 7]. Martin et al. [7] observed that the incidence of sepsis increased over a 22-year period from 82.7 cases per 100,000 population to 240.4 cases per 100,000 population in the USA. Additionally, an increasing trend in severe sepsis over time has been described, escalating from 168,239 cases in 1993 to 391,544 cases in 2003 [6].
Sepsis-associated mortality is high. Sepsis is the tenth leading cause of death in the USA [8]. Blanco et al. [9] published mortality rates for sepsis from 28 to 56 %, despite the launch of the “Surviving Sepsis Campaign” in 2004 with the purpose of reducing sepsis mortality through the development and publication of clinical practice guidelines. Several studies have shown that sepsis mortality increases as sepsis severity progresses to severe sepsis or septic shock [10–15]. Severe sepsis is the most common cause of death in non-coronary critical care units [1]. The number of organ failures (severe sepsis) is the predominant variable responsible for predicting inpatient mortality [6, 11, 15, 16].
Despite continuity of care, sepsis substantially reduces the survivors’ quality of life [17]. It has been suspected that numerous discharged sepsis patients have poor prognoses due to cognitive and functional impairments [18, 19].
Furthermore, sepsis has a significant impact on healthcare resources utilization. These patients often have complex long-term hospitalizations. Sepsis is responsible for an estimated 2 % of the discharges in tertiary hospitals [20], and it is among the leading causes of admission to intensive care units (ICUs) [21, 22].
The increased length of hospital stay and financial charges associated with individuals who experienced septic syndrome lead to significant economic burden [23]. Previous Spanish studies and those in other countries have shown that patients hospitalized with severe sepsis caused a substantial increase in hospital costs [9, 12, 24, 25].
For these reasons, both sepsis and severe sepsis are considered a significant public health problem, because of the increased costs of hospital care, their high morbidity and mortality rates, as well as personal financial burden derived from acute inpatient hospital care and long-term skilled nursing facility care and familial hardships endured [4, 25, 26].
Recently, administrative sepsis data have been analyzed to expand the epidemiological knowledge of sepsis. Discharge records provided a wealth of knowledge concerning incidence, outcome. and economic burden of septic syndrome, by illuminating trends and disparities [4, 6, 7, 27–31].
Temporal data on the occurrence and outcome of sepsis may be useful for the establishment of healthcare policies. Specifically, the data may better inform policy makers concerning the allocation of scarce resources and evaluation of quality sepsis care.
The objectives of this study were to examine the temporal trends in hospitalizations of patients with sepsis in the Region of Madrid (Spain) from 2003 to 2011 and to analyze the factors associated with inpatient mortality in this period.
Materials and methods
Study design
Descriptive population-based cross-sectional study of all hospital admissions with sepsis from 2003 to 2011 in the Region of Madrid (Spain).
Study population and data source
All sepsis hospitalizations (public and private hospitals) from 2003 to 2011 among residents in the Region of Madrid. The source of information was the hospital discharge minimum basic data set (MBDS) from the Region of Madrid.
The annual population of the Region of Madrid by age and gender for each year of the study period was obtained from the municipal census (estimation of the population at mid-period), ranging from 5,761,892 in 2003 to 6,489,680 in 2011.
Study variables
To identify episodes of sepsis, we applied the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) definition. Episodes selection was based on codes used previously by Kumar et al. [29] and Andreu Ballester et al. [11] (Supplementary Table 1). All sepsis hospitalizations were analyzed regardless of the specific cause, whether from sepsis directly, or intercurrent sepsis during the hospitalization, or from other processes. Therefore, the principal diagnosis and the secondary diagnosis (up to 13 diagnoses) were considered.
The following data were collected: age, gender, presence of selected comorbidities, and number of organ failures in sepsis (both were identified using ICD-9-CM codes, Supplementary Table 2). Comorbidities considered included: hypertension, diabetes mellitus, cirrhosis, solid organ transplant, human immunodeficiency virus (HIV), congestive heart failure, chronic obstructive pulmonary disease, cancer, and end-stage renal disease. Additionally, organ system failures assessed included: respiratory, cardiovascular, renal, hepatic, hematologic, metabolic, and neurologic. Severe sepsis was defined when one or more organs were involved, according to the 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference [1].
Furthermore, the type of microorganism involved in the sepsis (Gram-negative bacteria, Gram-positive bacteria, or fungi) was also collected, when available. Other variables obtained were: date of admission and discharge, length of hospital stay, and type of discharge. Discharge was classified as in home, continuity care (home hospital, other health centers or social facilities), deceased, and other. Also, ICD-9-CM procedure codes were used to identify episodes that underwent mechanical ventilation or received blood products or vasopressor agents. The codes used were: 96.7, 96.70, 96.71, and 96.72 (mechanical ventilation), 99.03, 99.04 (blood transfusion), and 00.17 (vasopressor agents).
Given the operational characteristics of the study, including the current legislative limitations and source of data made prior, consent from the patients and ethics committee approval were unnecessary.
Statistical analysis
Crude and age-adjusted rates by gender for each annual period were calculated. Rates were age adjusted using direct methods (European standard population).
A descriptive analysis was performed on inpatients with sepsis. To simplify data presentation, the study period was grouped into three sub-periods (sub-period 1: 2003–2005, sub-period 2: 2006–2008, and sub-period 3: 2009–2011). Factors associated with patient death were also studied. Bivariate and multivariate analyses were performed accounting mortality as the dependent variable, and age, gender, comorbidities, sepsis present at admission, specific, and number of organ failures as the independent variables. Bivariate analysis was carried out through the Chi-square statistic and multivariate analysis with logistic regression. Crude and adjusted odds ratios (aOR) were calculated, along with the 95 % confidence interval (CI), as the measure of association.
Estimates were made using the PASW Statistics 18 program and statistical significance was set using two-tailed α < 0.05.
Results
Trend in hospitalization rates
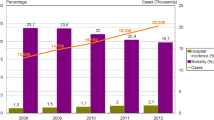
A total of 98,898 hospitalizations with sepsis were identified between 2003 and 2011. The incidence of sepsis hospitalizations increased from 114.4 per 100,000 population in 2003 to 262.2 in 2011 in males, and from 91.2 in 2003 to 209.1 in 2011 in females (Fig. 1). After age adjustment, the rates remained higher in males but with increasing tendency in both genders.
Characteristics of patients with sepsis
Table 1 shows the demographic characteristics and coexistent conditions in patients with sepsis in each sub-period considered.
The mean age of all patients was 60.0 [standard deviation (SD) 28.6], increasing over the study sub-periods from 55.4 years in the first sub-period (2003–2005) to 63.0 years in the third sub-period (2009–2011). 59.6 % of all episodes of sepsis were among people aged 65 years or more. Males accounted for a constant 54.4 % of all hospitalizations throughout the entire study.
At least one comorbidity was present in 66.3 % of sepsis episodes. The presence of more than one comorbidity increased over the sub-periods, from 26.1 % in the sub-period 2003–2005 to 31.4 % in the sub-period 2009–2011. The most common comorbidity related to sepsis was hypertension, the second was cancer, followed by diabetes, whereas the percentage of patients with HIV infection and solid organ transplant was lower during the studied period.
There were 45,936 (46.4 %) episodes of severe sepsis (>1 organ failure) showing a clear upward trend, especially in multi-organ failure.
The most common organ system failure was renal (24.3 %), followed by respiratory (17.2 %) and cardiovascular (16.8 %).
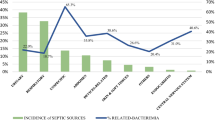
Microbiologic diagnosis of the infection was registered in 13,668 (13.8 %) episodes of sepsis. From 2003 to 2011, Gram-positive bacteria was the predominant sepsis-causing organism.
Among the procedures, vasopressor agents prescription increased from 885 (2.6 %) in the second sub-period to 2,039 (4.6 %) in the third sub-period. During the first sub-period, these agents were not used.
Regarding the length of hospital stay, this remained stable throughout the first two sub-periods (22.6 and 23.2 days. respectively), slightly decreasing in the third sub-period (20.4 days). The proportion of patients discharged home was 71 %, with a small increase in the proportion discharged to skilled nursing home care/social health centers (3.9 % in the first sub-period, 5.0 % in the second, and 5.6 % in the third).
Mortality trends
Hospital sepsis mortality was 23.2 %. Upon analysis, only severe sepsis mortality appeared to follow a declining trend throughout the entire period, in both males (40.0 % in 2003 to 31.8 % in 2011) and females (41.6 % in 2003 to 35.2 % in 2011), illustrating a downward trend since 2007 with no clear difference by gender, as shown in Fig. 2.
Factors associated with inpatient mortality
Throughout the study, death was most frequent among the elderly, inpatients with a higher number of comorbidities, and those with a greater number of organ system failures (Table 2). There was no observed difference in mortality between males and females. A decrease in the proportion of the mortality in the third sub-period (2009–2011) compared to the previous sub-periods was observed in all comorbidities analyzed, except for HIV, which accounted for 17.2 %, 19.6 %, and 22.6 % in the sub-periods of 2003–2005, 2006–2008, and 2009–2011, respectively. Out of all observed organ failures, the proportion of deaths decreased in the last period, with the exception of hematologic organ failure. After adjusting for other variables, the probability of fatal outcome due to sepsis over the three sub-periods was greater with age, with a marked gradient increasing with age except for children between 1 and 14 years old (Table 3). Also, a higher risk of death was attributed to a higher number of comorbidities (with the exception of sub-period 2006–2008). The presence of cancer or congestive heart failure led to a greater likelihood of mortality. An increasing gradient depending on the number of organs involved was observed, although mortality risk was significantly lower in the last sub-period with respect to the first (in the sub-period 2003–2005, aOR 6.1, 95 % CI 4.3–8.9, for those with four or more organs failure with respect to no organ failure, and in 2009–2011, this aOR was 2.7, 95 % CI 2.3–3.3). Cardiovascular and hepatic failure had higher risks of death over the whole study period.
Discussion
This study updates data trends for patients hospitalized with sepsis in a populous region of Southern Europe. The study revealed a progressive increase in sepsis and severe sepsis incidence from 2003 to 2011, but a decrease in inpatient mortality in Madrid, Spain. The leading factors associated with inpatient mortality included age, number of comorbidities, and number of organ failures.
The study by Martin et al. [7] found that US patients with sepsis increased 13.7 % per year from 1979 to 2000. In addition, patients with three or more failing organs had a 70 % chance of dying. Furthermore, the study by Dombrovskiy et al. [6] found that severe sepsis among sepsis patients in the USA had increased during the study period (1993–2003), with advanced age linked to greater mortality. Kumar et al. [29] published that the frequency of severe sepsis increased from 143 per 100,000 in US adults in 2000 to 343 per 100,000 in 2007, observing an increase in mortality with three or more failing organs (15.2 % to 24.9 %). In a recent USA study, the age-adjusted rate of sepsis-associated mortality decreased by 0.18 % per year between 1999 and 2005 [31].
A Spanish study between 1995 and 2004 [11] found that the hospitalization rates due to sepsis increased during the whole study period after adjusting for age, increasing from 64.11 to 114.02 cases per 100,000 population in males and from 45.08 to 83.62 cases among females. An increase in mortality was also observed (mortality in severe sepsis increased from 48 % in 1995 to 55 % in 2004). Another Spanish multicenter study by Blanco et al. [9] discovered a high incidence (25 cases per 100,000) of severe sepsis in ICU patients and a high mortality rate; 54.3 % in the hospital and 48.2 % in ICU patients.
Sepsis is becoming a significant public health problem, especially in hospitals, as a result of medical and technological advances associated with treatments. The increasing number of elderly and patients with underlying diseases such as cancer who require therapy combined with the widespread use of antibiotics has been linked to the growth of drug-resistant microorganisms [3, 32]. Despite this, a better codification of sepsis could help increase the detection and tracking of the cases and discharges.
Early recognition of serious illness or pathological process by a medical doctor and, therefore, early treatment of patients with sepsis through new treatment protocols may contribute in reducing mortality. A factor that could explain the recent decrease in inpatient mortality in our study is the increased use of vasopressor agents since 2004, as well as the availability of protocols such as the “Surviving Sepsis Campaign”, whose main aim is to achieve: venous oxygen saturation greater than 70 %, mean blood pressure of 65 mm/Hg, venous central pressure between 8–12 mm/Hg, and urine output of at least 0.5 ml/Kg/h in less than 6 h, and early treatment with broad-spectrum antibiotics [10].
Our study agrees with previous investigations with regard to higher rates of sepsis among males [12, 13, 16, 33]. In the study by Martin et al. [7], after adjustment for gender, US males were more likely to have sepsis than females in every year of the 22-year study, with a mean annual relative risk of 1.28. Our study did not find a difference in inpatient mortality with respect to gender. However, studies on mortality in severe sepsis have revealed contradictory results, with increased risk of death in males [6, 15] and females [29]. Nevertheless, a multivariate analysis conducted by Angus et al. [4] did not find any differences by gender with respect to the probability of death from severe sepsis when adjusting for age, comorbidities, and site infection.
In the present study, more than 50 % of patients with sepsis were aged 65 years or more, with an increasing trend of inpatient mortality with age, being especially high in those older than 84 years. This finding is consistent with the work of Vincent et al. [16], who found that age was associated with increased mortality in sepsis. Martin et al. [7] found a tendency in the average age of sepsis patients, beginning with an average of 57.4 years in the first period and ending with an average of 60.8 years in the last period. In an Australian study carried out by Ghelani et al. [32] between July 1993 and June 1999, the average age of patients with sepsis admitted to the ICU was 62.6 years and the average age of patients with nosocomial sepsis was 66.3 years.
The incidence of organ failure increased over time. Andreu Ballester et al. [11] observed that failure increased from 48 % among patients in 1995 to 55 % in 2004. Similar to the present study, Banta et al. [15], observed that the principal comorbidities and organ failures that predicted mortality were cancer, congestive heart failure, and hepatic and respiratory failure.
In another study carried out in Spain in 2001, Iñigo et al. [12] found that the comorbidities more associated to death were neoplasia (47.2 %) and cirrhosis (42.2 %), whereas the organs that failed most were the liver (63.8 %) and the cardiovascular system (56.7 %). These percentages were higher than those found in our study. In the multivariate analysis, cancer was the comorbidity that predominately predicted inpatient mortality in all three sub-periods, followed by congestive heart failure. On the other hand, liver failure was the principal predictor of inpatient mortality, followed by failure of the cardiovascular system. These findings are consistent with previous studies [13, 29, 33].
Regarding microorganisms isolated, we found that, during the first sub-period (2003–2005), Gram-negative bacteria were more frequent, coinciding with the data of a similar study for the same period [11]. However, in the two following sub-periods, Gram-positive bacteria was the most common causative organism. That may be due to the increase of severe sepsis and of the microbiological isolates in them. In the last several decades, Gram-positive microorganisms have become one of the most common microorganisms isolated in severe sepsis and septic shock [7]. In any case, these results should be construed with caution due to the uncommonly low proportion of positive cultures.
Our study has some limitations. In relation to the information source, the use of an administrative source restricts our definition of severe sepsis to those with more than one organ failure; these terms do not allow for the precise characterization and staging of patients with this condition [1, 34]. Also the use of ICD-9-CM codes pose difficulties in identifying the clinical signs of systemic inflammatory response for infection. Furthermore, the definition adopted in this study has been subject to some criticism, since it could both overestimate and underestimate the precise incidence of severe sepsis [7]. This information system may not detect important severity differences, through the scores used in the ICU for estimating the severity and risk in these patients (APACHE, SAPS, MPM, or SOFA). Lastly, complete information about mortality after discharge is also not available.
In a large region of Southern Europe for a 9-year period (2003–2011), an increasing trend in the incidence of sepsis was observed, but also a decreasing trend for in-hospital mortality in patients with severe sepsis. The mortality increased with age, comorbidities, and multi-organ failures.
Despite advances in the treatment of these patients [10], we advise the adoption of a consensus-based multidisciplinary measure among different hospital departments and the implementation of standard protocols to shorten intervention time, thus optimizing patient outcome. These measures will assist future sepsis research investigations to better optimize patient treatment and epidemiological outcomes.
References
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D et al (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med 31:1250–1256
Robertson CM, Coopersmith CM (2006) The systemic inflammatory response syndrome. Microbes Infect 8:1382–1389. doi:10.1016/j.micinf.2005.12.016
Slade E, Tamber PS, Vincent J-L (2003) The Surviving Sepsis Campaign: Raising awareness to reduce mortality. Crit Care 7:1–2
Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR (2001) Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med 29:1303–1310. http://www.ncbi.nlm.nih.gov/pubmed/11445675
Moss M (2005) Epidemiology of sepsis: race, sex, and chronic alcohol abuse. Clin Infect Dis 41(Suppl 7):S490–S497. doi:10.1086/432003,
Dombrovskiy VY, Martin AA, Sunderram J, Paz HL (2007) Rapid increase in hospitalization and mortality rates for severe sepsis in the United States: a trend analysis from 1993 to 2003. Crit Care Med 35:1244–1250. doi:10.1097/01.CCM.0000261890.41311.E9, http://www.ncbi.nlm.nih.gov/pubmed/17414736
Martin GS, Mannino DM, Eaton S, Moss M (2003) The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med 348:1546–1554. doi:10.1056/NEJMoa022139, http://www.ncbi.nlm.nih.gov/pubmed/12700374
Kung H-C, Hoyert DL, Xu J, Murphy SL (2008) Deaths: final data for 2005. Natl Vital Stat Rep 56:1–120
Blanco J, Muriel-Bombín A, Sagredo V, Taboada F, Gandía F, Tamayo L et al (2008) Incidence, organ dysfunction and mortality in severe sepsis: a Spanish multicentre study. Crit Care 12:R158. doi:10.1186/cc7157, http://www.ncbi.nlm.nih.gov/pubmed/19091069
Levy MM, Dellinger RP, Townsend SR, Linde-Zwirble WT, Marshall JC, Bion J et al (2010) The surviving sepsis campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Intensive Care Med 36:222–231. doi:10.1007/s00134-009-1738-3
Andreu Ballester JC, Ballester F, González Sánchez A, Almela Quilis A, Colomer Rubio E, Peñarroja Otero C (2008) Epidemiology of sepsis in the Valencian community (Spain), 1995–2004. Infect Control Hosp 29:630–634. doi:10.1086/589583
Iñigo J, Sendra JM, Díaz R, Bouza C, Sarría-Santamera A (2006) Epidemiología y costes de la sepsis grave en Madrid. Estudio de altas hospitalarias. Med Intensiva 30:197–203, http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S0210-56912006000500001&nrm=iso
Azkárate I, Sebastián R, Cabarcos E, Choperena G, Pascal M, Salas E (2012) A prospective, observational severe sepsis/septic shock registry in a tertiary hospital in the province of Guipuzcoa (Spain). Med Intensiva 36:250–256. doi:10.1016/j.medin.2011.10.006
Wenzel RP (2002) Treating sepsis. N Engl J Med 347:966–967. doi:10.1056/NEJMp020096, http://www.ncbi.nlm.nih.gov/pubmed/12324551
Banta JE, Joshi KP, Beeson L, Nguyen HB (2012) Patient and hospital characteristics associated with inpatient severe sepsis mortality in California, 2005–2010. Crit Care Med 40:2960–2966. doi: 10.1097/CCM.0b013e31825bc92f
Vincent J-L, Sakr Y, Sprung CL, Ranieri VM, Reinhart K, Gerlach H et al (2006) Sepsis in European intensive care units: results of the SOAP study. Crit Care Med 34:344–353
Winters BD, Eberlein M, Leung J, Needham DM, Pronovost PJ, Sevransky JE (2010) Long-term mortality and quality of life in sepsis: a systematic review. Crit Care Med 38:1276–1283. doi:10.1097/CCM.0b013e3181d8cc1d
Yende S, Angus DC (2007) Long-term outcomes from sepsis. Curr Infect Dis Rep 9:382–386
Iwashyna TJ, Ely EW, Smith DM, Langa KM (2010) Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA 304:1787–1794. doi:10.1001/jama.2010.1553
Sands KE, Bates DW, Lanken PN, Graman PS, Hibberd PL, Kahn KL et al (1997) Epidemiology of sepsis syndrome in 8 academic medical centers. JAMA 278:234–240
Harrison DA, Welch CA, Eddleston JM (2006) The epidemiology of severe sepsis in England, Wales and Northern Ireland, 1996 to 2004: secondary analysis of a high quality clinical database, the ICNARC Case Mix Programme Database. Crit Care 10:R42. doi:10.1186/cc4854
Vincent J-L, Opal S, Torres A, Bonten M, Cohen J, Wunderink R (2003) The PIRO concept: I is for infection. Crit Care 7:252–255. doi:10.1186/cc2194
Bates DW, Yu DT, Black E, Sands KE, Schwartz JS, Hibberd PL et al (2003) Resource utilization among patients with sepsis syndrome. Infect Control Hosp Epidemiol 24:62–70. doi:10.1086/502117
Davies A, Green C, Hutton J, Chinn C (2001) Severe sepsis: a European estimate of the burden of disease in ICU. Intensive Care Med 27:581A
Burchardi H, Schneider H (2004) Economic aspects of severe sepsis: a review of intensive care unit costs, cost of illness and cost effectiveness of therapy. Pharmacoeconomics 22:793–813, http://www.ncbi.nlm.nih.gov/pubmed/15294012
Angus DC (2010) The lingering consequences of sepsis: a hidden public health disaster? JAMA 304:1833–1834. doi:10.1001/jama.2010.1546
Dombrovskiy VY, Martin AA, Sunderram J, Paz HL (2005) Facing the challenge: decreasing case fatality rates in severe sepsis despite increasing hospitalizations. Crit Care Med 33:2555–2562
Dombrovskiy VY, Martin AA, Sunderram J, Paz HL (2007) Occurrence and outcomes of sepsis: influence of race. Crit Care Med 35:763–768. doi:10.1097/01.CCM.0000256726.80998.BF
Kumar G, Kumar N, Taneja A, Kaleekal T, Tarima S, McGinley E et al (2011) Nationwide trends of severe sepsis in the 21st century (2000–2007). Chest 140:1223–1231. doi:10.1378/chest.11-0352
Wenzel RP, Edmond MB (2000) Managing antibiotic resistance. N Engl J Med 343:1961–1963. doi:10.1056/NEJM200012283432610
Melamed A, Sorvillo FJ (2009) The burden of sepsis-associated mortality in the United States from 1999 to 2005: an analysis of multiple-cause-of-death data. Crit Care 13:R28. doi:10.1186/cc7733
Ghelani D, Moran JL, Sloggett A, Leeson RJ, Peake SL (2009) Long-term survival of intensive care and hospital patient cohorts compared with the general Australian population: a relative survival approach. J Eval Clin Pract 15:425–435. doi:10.1111/j.1365-2753.2008.01030.x
Brun-Buisson C, Meshaka P, Pinton P, Vallet B (2004) EPISEPSIS: a reappraisal of the epidemiology and outcome of severe sepsis in French intensive care units. Intensive Care Med 30:580–588. doi:10.1007/s00134-003-2121-4
Iwashyna TJ, Odden A, Rohde J, Bonham C, Kuhn L, Malani P et al (2012) Identifying patients with severe sepsis using administrative claims: patient-level validation of the Angus implementation of the international consensus conference definition of severe sepsis. Med Care. doi:10.1097/MLR.0b013e318268ac86
Acknowledgments
We thank Alexander J. Louie BSPH, BSN, RN-PHN of the University of California, Irvine, for the assistance with the revision of the manuscript.
Conflict of interest
All the authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 46 kb)
Rights and permissions
About this article
Cite this article
Ayala-Ramírez, O.H., Domínguez-Berjón, M.F. & Esteban-Vasallo, M.D. Trends in hospitalizations of patients with sepsis and factors associated with inpatient mortality in the Region of Madrid, 2003–2011. Eur J Clin Microbiol Infect Dis 33, 411–421 (2014). https://doi.org/10.1007/s10096-013-1971-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-013-1971-0