Abstract
Multiple sclerosis (MS) is the prototypical inflammatory disease of the central nervous system and spinal cord, leading to axonal demyelination of neurons. Recently, we have found a correlation between fungal infection and MS in peripheral blood of patients. The present work provides evidence of fungal infection in the cerebrospinal fluid (CSF) of some MS patients. Thus, fungal antigens can be demonstrated in CSF, as well as antibodies reacting against several Candida species. Comparison was made between CSF and blood serum for the presence of fungal antigens (proteins) and antibodies against different Candida spp. Analyses of both CSF and serum are complementary and serve to better evaluate for the presence of disseminated fungal infection. In addition, PCR analyses indicate the presence of DNA from different fungal species in CSF, depending on the patient analyzed. Overall, these findings support the notion that fungal infection can be demonstrated in CSF from some MS patients. This may constitute a risk factor in this disease and could also help in understanding the pathogenesis of MS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple sclerosis (MS) is an inflammatory and demyelinating disease of the central nervous system (CNS) in which sclerotic plaques form in the brain and spinal cord [1–3]. This complex disease is thought to be triggered by an interaction between genetic and environmental factors [4–9]. MS is prototypical of inflammatory CNS diseases and is associated with a variety of clinical symptoms. Motor impairment and sensory organ dysfunction are two major problems associated with MS. Current therapies are based on immunosuppressive and immunoregulatory compounds that aim to reduce inflammation. However, these therapies are of little benefit in advanced stages of the disease [3].
The exact cause of MS has been the object of intensive research in many laboratories, although the etiology of MS remains enigmatic. Autoimmunity has been put forward as a plausible cause of this disease [10, 11]. Autoimmunity may result from the presence of viral proteins or other pathogen antigens that mimic self-protein molecules in the CNS [12, 13]. However, no association between antimyelin antibodies and progression to MS exists [14]. Moreover, a disorder of the immune system that attacks oligodendrocytes does not account for some clinical observations. For instance, the existence of distinct foci of degeneration cannot be explained by indiscriminate aggression against glial cells [15]. Furthermore, blood vessel inflammation is not easily explained by autoimmunity and destruction of nerve cells [16]. Intensive research to find an infectious agent that directly provokes or triggers MS has been carried out in many laboratories. We have provided evidence that fungal infection is the etiological agent of acute zonal occult outer retinopathy (AZOOR) [17, 18]. This ocular disease was thought to be an autoimmune disorder that affects the optic nerve and the retina [19, 20]. Some AZOOR patients may also present clinical symptoms in the CNS [21, 22]. Moreover, a relationship between AZOOR and other autoimmune diseases including MS has been noted [19, 22]. Recently, we found evidence of disseminated fungal infection in MS patients, since there were elevated levels of yeast antigens in peripheral blood serum [23, 24]. These considerations prompted us to investigate the existence of antibodies against different fungi, as well as the presence of fungal antigens and DNA in cerebrospinal fluid (CSF) from these patients. Our present findings provide evidence of the existence of different fungal species in CSF. These observations are novel and may be of interest in understanding the pathophysiology of this demyelinating disease.
Materials and methods
Description of patients
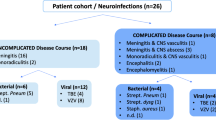
Table 1 lists the patients involved in this study. Eight women and four men were analyzed, thus two-thirds were women, as is the case in MS in the general population. Onset of the disease was recent in all patients and all had a score of 1 on the Expanded Disability Status Scale (EDSS). Therefore, all patients exhibited early symptoms of MS and none of them had been treated with antifungal therapy. None of the patients was receiving immunosuppressive therapies. In general, all patients were young adults with the exception of one 57-year-old man. Peripheral blood and CSF samples were only obtained once the informed consent had been signed. The Ethics Committee of the Universidad Autónoma de Madrid approved the study.
Slot-blot analyses
Two hundred microliters of different serum or cerebrospinal fluid (CSF) dilutions in TBS were added to each well. Samples were blotted onto a 45-mm nitrocellulose membrane (Bio-Rad), previously hydrated in TBS for 10 min using the Bio-Dot SF apparatus (Bio-Rad). After blotting, the membrane was processed and developed as described for western blotting. The primary antibodies, rabbit polyclonal antibodies raised against C. famata, C. albicans, C. glabrata, or C. parapsilosis, as described above, were used at a 1:1,000 dilution. Secondary antibody, a donkey anti-rabbit IgG horseradish peroxidase-conjugated antibody (Amersham Biosciences), was used at a 1:5,000 dilution.
In previous works, we established that values below 10 in this assay should be considered as negative, between 10 and 20 as uncertain, and values above 20 as positive. In the latter case, values between 20 and 50 are considered low, between 50 and 80 as moderate and above 80 as high.
Immunofluorescence assay
For C. famata, 1 ml of culture was placed in 1.5-ml microcentrifuge tubes. Cells were washed with PBS, incubated with 50 mM ammonium chloride for 10 min, and washed three times with PBS-Tween 20. Cells were then treated with the different sera diluted 1:500 and 1:5 respectively, in PBS-Tween 20, at 37 °C for 2 h, washed again with PBS-Tween 20 and incubated with the secondary antibody. Rabbit anti-human immunoglobulins IgG + IgA + IgM (Sigma) fluorescein-conjugated antibody was added at a 1:500 dilution. The cells were then washed, resuspended in PBS, and mounted on slides with a drop of Depex (Serva). Finally, the cells were observed under a fluorescence microscope. For the remaining Candida species, C. albicans, C. glabrata, C. parapsilosis, C. tropicalis, and C. krusei, the commercial kit Euroimmun (MedizinischeLabordiagnostika AG) was used in accordance with the manufacturer’s instructions and using the same serum dilutions as for C. famata.
DNA extraction from CSF
The following method was used to extract DNA from CSF: 20 μl of proteinase K was added to 100 μl of CSF, after 200 μl buffer AL was added and was mixed by pulse-vortexing for 15 s. This mixture was incubated at 56 °C for 10 min. 200 μl ethanol was added to each sample and mixed by pulse-vortexing for 15 s. The mixture was carefully applied to the QIAamp Mini spin column and centrifuged at 8,000 rpm for 1 min. Afterward, 500 μl buffer AW was added and centrifuged at 8,000 rpm for 1 min. 500 μl buffer AW2 was applied and centrifuged at 14,000 rpm for 3 min. Finally, each sample was resuspended in 40 μl distilled water. DNA from extracts was quantified by The NanoDrop® ND-1000 UV–vis Spectrophotometer. Negative controls included three tubes of tri-distilled filtered water.
Design of the primers
Sequences of 18S and 5.8S rRNA genes and internal transcribed spacer 1 (ITS 1) region from several organisms (C. famata, Pichia guilliermondii, C. albicans, C. parapsilosis, C. glabrata, Rhodotorula mucilaginosa, Cryptococcus. neoformans, and Homo sapiens) were accessed via the GenBank database and were aligned by using the Sequence Analysis Package (Clustal W). Multiple potential primer-binding sites for the panfungal primer pair were chosen by comparing regions of Candida homologous with regions of the fungal group from the fungal kingdom with the most divergent DNA sequences and regions of Candida incongruous with the human DNA sequence. The primer selection was optimized for melting temperature equivalence, lack of duplex, hairpin, or primer-dimer formation, and internal stability by using OLIGO software (Amplify).
PCR analyses
The measures used to avoid PCR assay contamination included the use of separate rooms and glassware supplies for PCR set-up and products, aliquoted reagents, positive-displacement pipettes, aerosol-resistant tips, and multiple negative controls. DNA samples obtained from CSF were analyzed by nested PCR. The first PCR was carried out with 4 μl of DNA incubated at 95 °C for 10 min and amplified by 30 cycles of 45 s at 94 °C, 1 min at 57.3 °C, and 45 s at 72 °C. The oligonucleotides used were 5 GTTCTGGGCCGCACGGG3′ and 3′GGCAAAGATTCGATGATT5. The second PCR was carried out with 0.5 μl of the product obtained in the first PCR and amplified by 35 cycles of 45 s at 94 °C, 1 min at 52 °C, and 45 s at 72 °C. The oligonucleotides used were 5′ GCGTCTAGACCTGCGGAAGGATCA3 and 3′ GCGAAGCTTGATCCGTTGTTGAAA5. The amplified product was analyzed by agarose gel electrophoresis.
Results
Analysis of fungal antigens in CSF and in serum
There is no universal test to determine whether disseminated fungal infection is present in a patient. We have developed a very sensitive method based on the slot-blot technique to analyze yeast antigens in human sera [18, 25]. We have analyzed several yeast antigens using rabbit antibodies obtained after injection of the different yeast species indicated [18, 25]. It should be noted that the antigens detected by slot-blot correspond to fungal proteins that immunoreact with the antibody used. This antigen could be of the same species as the one used to raise the antibody or there may be cross-reactivity among different fungal species.
Initially, we assessed the presence of fungal antigens in CSF using anti-C. famata and anti-C. parapsilosis antibodies by slot-blot (Table 1). Since we had to increase the amount of CSF and because samples are tested in triplicate, we only assayed these two antibodies, owing to the shortage of CSF. Analyses of fungal antigens in CSF indicated that the values obtained were negative in most cases. A notable exception was patient 7, a 35-year-old woman. It is most striking to find that very high levels of fungal antigens can be detected in CSF. Another two patients (9 and 12) could be classified as positive upon the analysis of the CSF (Table 1). As an example of the results obtained with the controls, as well as with patient 7, the direct results of the slot-blot are shown in Fig. 1. Clearly, the CSF control was negative, whereas a potent signal was observed with patient 7. We can conclude that fungal antigens can be detected in CSF from some MS patients. It was of interest to compare the presence of fungal antigens in CSF and blood serum from these 12 patients. In this case, since the amount of serum used is about 100-fold lower, we had enough material to test different antibodies, i.e. anti-C. famata, anti-C. albicans, anti-C. parapsilosis, and anti-C. glabrata. The highest values obtained with the 12 patients were found when the anti-C. famata antibody was employed (Table 2). There is only one negative patient (number 4); however, this patient was positive when the anti-C. glabrata antibody was used. An additional 4 patients (numbers 9, 10, 11, and 12) had rather high C. famata antigen levels, but the values obtained with the other three antibodies, when positive, were low. This may reflect the fact that the fungal antigens present in blood serum are more similar to C. famata than to the rest of yeast species analyzed. In such cases, it may be that antigens are not secreted into the bloodstream or that these antigens, if present, belong to fungal species not recognized by the rabbit antibody used.
The comparison between fungal antigens present in CSF and blood serum clearly indicates that there is no correlation between them. Thus, patient 7 exhibits a high value of fungal antigens in CSF, but curiously, in this case the levels of yeast antigens in blood serum were low. The contrary is true for patient 10 who had high values of fungal antigens in blood serum, while the CSF sample was negative when using anti-C. famata antibodies. Collectively, these findings suggest that the levels of fungal antigens in blood and CSF may differ, perhaps because the blood–brain barrier (BBB) is not permeable to macromolecules. Although, it should be possible that, in some instances, fungal infections or toxins [26, 27] could alter the BBB.
Analysis of Candida antibodies
Our next goal was to test whether antibodies against several Candida species can be detected in CSF from MS patients. The presence of antibodies against C. famata, C. albicans, C. parapsilosis, C. glabrata, and C. krusei was assayed by immunofluorescence. Figure 2 illustrates the type of immunoreaction obtained with one MS patient and one healthy volunteer. There is a clear immunoreactivity to some Candida species in one MS patient (number 11), whereas immunoreaction is not observed with another patient (number 1 and the healthy volunteer). This immunoreactivity varies according to the patient analyzed; thus, two of the CSF samples (patients 8 and 11) were very positive (Table 3). This finding reflects the existence of high-titer antibodies against yeast species in CSF from these two patients. On the other hand, patients 1, 5, 6, 7, and 9 were negative, whereas the remaining patients (numbers 2, 3, 4, 10, and 12) exhibited an intermediate reactivity (Table 3). Apart from the inter-patient variability, the important conclusion is that antibodies against Candida spp. can be detected in CSF samples from some MS patients.
Immunofluorescence analysis of antibodies present in CSF against different yeast species. In the case of C. famata, the protocol described in Materials and methods was followed. As a positive control (Control +), rabbit antiserum against C. famata was employed; as a negative control (Control −), PBS was added instead of primary antibody. For the remaining yeast species, the commercial kit Euroimmun was used. NP healthy volunteer used as a negative patient
To compare the presence of anti-Candida antibodies between CSF and blood serum, immunofluorescence analysis using peripheral blood serum from these patients was carried out (Table 4). Six out of 12 patients were very positive against at least one Candida species (patients 3, 4, 8, 10, 11, and 12). This observation reveals that these 6 patients exhibit a high antibody titer in blood serum. On the other hand, 3 patients (numbers 1, 5, and 6) have very low antibody titers against the six Candida species analyzed. The remaining patients (numbers 2, 7, and 9) had intermediate antibody values (Table 4). Not only did the presence or absence of antibodies vary from patient to patient, but the Candida species recognized by the different sera also varied. This variability may be dependent on the colonization of mucosae by different yeasts. Comparison of the presence of anti-Candida antibodies in CSF and blood serum samples indicates that 2 patients (numbers 8 and 11) had a high titer. Curiously, there are some patients with a high titer of antibodies in blood serum, but not in CSF. This is the case in patients 3, 4, and 12, indicating that a high titer of antibodies against Candida spp. in peripheral blood does not necessarily lead to a high titer in CSF, most probably due to the BBB.
Fungal DNA in CSF analyzed by PCR
Circulating fungal genomes in blood from patients with disseminated candidiasis have occasionally been observed [28–30]. Whether such an observation is made probably depends on the activity of fungal foci present in the different organs or tissues. On the other hand, the lack of DNA amplification by PCR in some patients may be because a potential fungal infection is not reflected in blood at the time when the sample was obtained.
Polymerase chain reaction provides a sensitive method for detecting fungal infection. Moreover, PCR bands can be separated on agarose gels, extracted, and sequenced, providing a clue to the fungal species present in CSF. Therefore, it was of great interest to analyze whether fungal DNA could be amplified in CSF from MS patients. Owing to the limited volume of CSF from some patients, we extracted DNA from patients 1, 2, 3, 4, 6, 7, 9, and 12. This DNA was amplified by PCR and the different bands observed were extracted and sequenced. The use of classical PCR is a good approach because it shows whether several DNA bands amplified. Figure 3 shows the result of the PCR from the CSF of the patients mentioned above. In all but one case, several bands were obtained. After DNA sequencing, the following fungal species were detected: Malassezia globosa (300 bp), related to Erythrobasidium clade (230 bp) and Rhodotorula mucilaginosa (180 bp). These findings indicate that each patient may contain different fungal DNAs and therefore the course of the disease may differ.
Polymerase chain reaction (PCR) analysis of different CSF. C negative PCR control without DNA. CE control of DNA extraction without CSF. PCR was carried out as described in Materials and methods
Evidence of fungal infection considering the different assays
The results obtained with the different tests carried out in this work are summarized in Table 5. The presence of fungal macromolecules such as fungal antigens (proteins) and DNA is taken as good evidence of fungal infection. Although the existence of anti-Candida antibodies does not constitute good proof of disseminated candidiasis, the presence of these antibodies may be of interest to provide an indication of the humoral immune response. Therefore, we conclude that there are signs of infection in the majority of patients. Only 2 patients were classified as negative (patients 5 and 6), and 1 as uncertain (patient 8). In principle, collection of additional samples in these patients in the future may also reveal the presence of fungal infection.
Discussion
The determination of the etiology of MS has remained elusive over the years. The most widespread idea is that MS represents an autoimmune disease that reacts against myelin, leading to the destruction of glial cells and is followed by axonal damage of neurons. Many researchers have suggested that a microbial infection may be the cause of MS [31, 32]. In this sense, a number of viruses have been considered as the etiological agent of this neurodegenerative disease. Particular attention has focused on CNS infection by the Epstein–Barr virus [33], although other viruses and bacteria have also been suggested, either as a direct cause of MS or as triggers of the autoimmune reaction [21, 34]. We have found evidence of an association between MS and fungal infections [23]. This was based on the presence of fungal antigens in peripheral blood from MS patients. In addition, follow-up of an MS patient over several years suggested that fungal macromolecules were present in peripheral blood and CSF samples [35]. In the present work we demonstrate that the presence of fungal macromolecules (proteins and DNA) can be demonstrated in CSF from some MS patients. Remarkably, our present findings indicate that fungal proteins can be detected in CSF from several MS patients. Moreover, fungal DNA can be amplified with some of these samples, revealing the presence of several fungal species. The PCR results are of particular interest because they point not only to the idea of a polymicrobial infection, but also to a variety of combinations of fungal species that infect MS patients. In summary, the evidence provided in our work suggests that fungal infection can be found in the CSF of several MS patients. This may represent an important risk factor in a better understanding of the pathology and evolution of the disease in some patients. Also, the potential presence of fungal toxins can play a part in the cytotoxicity and/or inflammation of the CNS in MS patients [26]. It will be of interest to analyze the presence of gliotoxin, or other potential toxins in CSF [27, 36]. Future work can explore the exact determination of fungal antigens present in serum and CSF, as well as ascertain the origin of their production, i.e. which tissues are infected and/or which mucoses are colonized by the fungi.
The presence of fungal infection in MS patients may, on the one hand, be because the infection is the actual cause of the disease or, on the other, infection may be a consequence of immune dysfunction in these patients [37]. Either way, the fungal infection should be treated appropriately with antifungal compounds. The presence of such an infection, even if it does not cause MS, may negatively affect the clinical course of neurodegeneration. Patients with MS are usually treated with corticosteroids and other immunosuppressive agents, which may be favored in the long-term fungal infections [38]. In such cases, diagnosis of this type of infection must be taken into consideration in the management of these patients.
References
Barnett MH, Sutton I (2006) The pathology of multiple sclerosis: a paradigm shift. Curr Opin Neurol 19(3):242–247
Hawker K (2011) Progressive multiple sclerosis: characteristics and management. Neurol Clin 29(2):423–434
Stadelmann C (2011) Multiple sclerosis as a neurodegenerative disease: pathology, mechanisms and therapeutic implications. Curr Opin Neurol 24(3):224–229
Burrell AM, Handel AE, Ramagopalan SV, Ebers GC, Morahan JM (2011) Epigenetic mechanisms in multiple sclerosis and the major histocompatibility complex (MHC). Discov Med 11(58):187–196
Giovannoni G, Ebers G (2007) Multiple sclerosis: the environment and causation. Curr Opin Neurol 20(3):261–268
Holmoy T, Harbo H, Vartdal F, Spurkland A (2009) Genetic and molecular approaches to the immunopathogenesis of multiple sclerosis: an update. Curr Mol Med 9(5):591–611
Kakalacheva K, Munz C, Lunemann JD (2011) Viral triggers of multiple sclerosis. Biochim Biophys Acta 1812(2):132–140
Marrie R (2011) Demographic, genetic, and environmental factors that modify disease course. Neurol Clin 29(2):323–341
Van der Mei IA, Simpson S Jr, Stankovich J, Taylor BV (2011) Individual and joint action of environmental factors and risk of MS. Neurol Clin 29(2):233–255
Goverman JM (2011) Immune tolerance in multiple sclerosis. Immunol Rev 241(1):228–240
Hollifield RD, Harbige LS, Pham-Dinh D, Sharief MK (2003) Evidence for cytokine dysregulation in multiple sclerosis: peripheral blood mononuclear cell production of pro-inflammatory and anti-inflammatory cytokines during relapse and remission. Autoimmunity 36(3):133–141
McCoy L, Tsunoda I, Fujinami RS (2006) Multiple sclerosis and virus induced immune responses: autoimmunity can be primed by molecular mimicry and augmented by bystander activation. Autoimmunity 39(1):9–19
Westall FC (2006) Molecular mimicry revisited: gut bacteria and multiple sclerosis. J Clin Microbiol 44(6):2099–2104
Kuhle J, Pohl C, Mehling M, Edan G, Freedman MS, Hartung HP, Polman CH, Miller DH, Montalban X, Barkhof F, Bauer L, Dahms S, Lindberg R, Kappos L and Sandbrink R (2007) Lack of association between antimyelin antibodies and progression to multiple sclerosis. N Engl J Med 356(4):371–378
Kutzelnigg A, Lucchinetti CF, Stadelmann C, Bruck W, Rauschka H, Bergmann M, Schmidbauer M, Parisi JE, Lassmann H (2005) Cortical demyelination and diffuse white matter injury in multiple sclerosis. Brain 128(Pt 11):2705–2712
D’Haeseleer M, Cambron M, Vanopdenbosch L, De Keyser J (2011) Vascular aspects of multiple sclerosis. Lancet Neurol 10(7):657–666
Carrasco L, Ramos M, Galisteo R, Pisa D, Fresno M, Gonzalez ME (2005) Isolation of Candida famata from a patient with acute zonal occult outer retinopathy. J Clin Microbiol 43(2):635–640
Pisa D, Ramos M, Garcia P, Escoto R, Barraquer R, Molina S, Carrasco L (2008) Fungal infection in patients with serpiginous choroiditis or acute zonal occult outer retinopathy. J Clin Microbiol 46(1):130–135
Gass JD (2003) Are acute zonal occult outer retinopathy and the white spot syndromes (AZOOR complex) specific autoimmune diseases? Am J Ophthalmol 135(3):380–381
Heckenlively JR, Ferreyra HA (2008) Autoimmune retinopathy: a review and summary. Semin Immunopathol 30(2):127–134
Jacobson DM (1996) Acute zonal occult outer retinopathy and central nervous system inflammation. J Neuroophthalmol 16(3):172–177
Monson DM, Smith JR (2011) Acute zonal occult outer retinopathy. Surv Ophthalmol 56(1):23–35
Benito-León J, Pisa D, Alonso R, Calleja P, Díaz-Sánchez M, Carrasco L (2010) Association between multiple sclerosis and Candida species: evidence from a case–control study. Eur J Clin Microbiol Infect Dis:1139–1145
Ramos M (2007) Diagnóstico de candidiasis mediante técnicas de PCR y de detección de antígenos fúngicos. Facultad de Ciencias. Universidad Autónoma de Madrid, Madrid
Pisa D, Ramos M, Molina S, Garcia P, Carrasco L (2007) Evolution of antibody response and fungal antigens in the serum of a patient infected with Candida famata. J Med Microbiol 56(Pt 5):571–578
Purzycki CB, Shain DH (2010) Fungal toxins and multiple sclerosis: a compelling connection. Brain Res Bull 82(1–2):4–6
Malcus-Vocanson C, Giraud P, Broussolle E, Perron H, Mandrand B, Chazot G (1998) A urinary marker for multiple sclerosis. Lancet 351(9112):1330
Avni T, Leibovici L, Paul M (2011) PCR diagnosis of invasive candidiasis: systematic review and meta-analysis. J Clin Microbiol 49(2):665–670
Bretagne S, Costa JM (2005) Towards a molecular diagnosis of invasive aspergillosis and disseminated candidosis. FEMS Immunol Med Microbiol 45(3):361–368
Khan ZU, Mustafa AS (2001) Detection of Candida species by polymerase chain reaction (PCR) in blood samples of experimentally infected mice and patients with suspected candidemia. Microbiol Res 156(1):95–102
Gilden DH (2005) Infectious causes of multiple sclerosis. Lancet Neurol 4(3):195–202
Giovannoni G, Cutter GR, Lunemann J, Martin R, Munz C, Sriram S, Steiner I, Hammerschlag MR, Gaydos CA (2006) Infectious causes of multiple sclerosis. Lancet Neurol 5(10):887–894
Wingerchuk DM (2011) Environmental factors in multiple sclerosis: Epstein-Barr virus, vitamin D, and cigarette smoking. Mt Sinai J Med NY 78(2):221–230
Cermelli C, Jacobson S (2000) Viruses and multiple sclerosis. Viral Immunol 13(3):255–267
Pisa D, Alonso R, Carrasco L (2011) Fungal infection in a patient with multiple sclerosis. Eur J Clin Microbiol Infect Dis 30(10):1173–1180
Rieger F, Amouri R, Benjelloun N, Cifuentes-Diaz C, Lyon-Caen O, Hantaz-Ambroise D, Dobransky T, Perron H, Gemy C (1996) Gliotoxic factor and multiple sclerosis. CR Acad Sci 319(4):343–350
Wu GF, Alvarez E (2011) The immunopathophysiology of multiple sclerosis. Neurol Clin 29(2):257–278
Gutwinski S, Erbe S, Munch C, Janke O, Muller U, Haas J (2010) Severe cutaneous Candida infection during natalizumab therapy in multiple sclerosis. Neurology 74(6):521–523
Acknowledgements
The study was supported by a grant from the Fundación de Investigación Médica Mutua Madrileña. We also acknowledge an institutional grant to Centro de Biología Molecular from the Fundación Ramón Areces.
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pisa, D., Alonso, R., Jiménez-Jiménez, F.J. et al. Fungal infection in cerebrospinal fluid from some patients with multiple sclerosis. Eur J Clin Microbiol Infect Dis 32, 795–801 (2013). https://doi.org/10.1007/s10096-012-1810-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-012-1810-8