Abstract
Rapid bacterial typing is a valuable and necessary tool in the prevention and detection of outbreaks. The purpose of this study was to adapt a multilocus variable number of tandem repeats analysis (MLVA) for analysis on a benchtop capillary electrophoresis instrument and compare the modified assay with multilocus sequence typing (MLST) for typing cefpodoxime-resistant Escherichia coli (E. coli). Further, we identified the causative resistance mechanisms and epidemiological type of infection for isolates producing extended-spectrum β-lactamases (ESBLs). A collection of E. coli resistant to cefpodoxime was typed by MLST and a modified MLVA assay using a benchtop capillary electrophoresis instrument. Resistance mechanisms were identified by polymerase chain reaction (PCR) and sequencing. Patient history was examined to establish the epidemiological type of infection for ESBL-producing E. coli. MLVA yielded typing results homologous with MLST and it correctly identified E. coli sequence type (ST) 131 that was accounting for 45 % of all ESBL-producing isolates in the sample collection. The majority (76.7 %) of ESBL-producing isolates was healthcare-related and only 23.3 % of the ESBL-producing isolates were community-onset infections (COI), regardless of the ST. Patients with COI were significantly more often of female gender and younger age compared to healthcare-associated infections (HCAI) and hospital-onset infections (HOI). In conclusion, the modified MLVA is a useful tool for the rapid typing of E. coli and it identified ST131 as the predominating ESBL-producing lineage in Copenhagen. Healthcare-related infections were the predominant infection setting of ESBL-producing E. coli and the demographic characteristics differed between patients with COI and healthcare-related infections.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bacterial typing is a valuable tool in both outbreak investigation and epidemiological surveillance. Multilocus sequence typing (MLST) is an excellent tool for longitudinal epidemiological surveillance [1]. The method is, however, laborious. Multilocus variable number of tandem repeats analysis (MLVA) provides many of the benefits of MLST at lesser economic and labor cost, and still fulfils essential criteria for typing methods, such as high discriminatory power, high typability, and reproducibility [2]. Several MLVA protocols have been developed for the typing of enterohemorrhagic Escherichia coli (E. coli) O157 [3, 4], as well as MLVA protocols designed to detect all serogroups of E. coli [5, 6]. However, all the typing methods described rely on fragment analysis using sequencing apparatuses. Benchtop capillary electrophoresis instruments are increasingly used as an alternative to agarose gel electrophoresis. This method allows automation and offers increased accuracy of size determination and high throughput compared to gel electrophoresis, and may provide an alternative to more expensive sequence apparatuses in MLVA protocols.
Enterobacteriaceae producing extended-spectrum β-lactamases (ESBLs) constitute a major global health concern [7]. E. coli sequence type (ST) 131 expressing blaCTX-M-15 is of particular concern, as this lineage has been established worldwide and has been reported as a pathogen capable of efficient transmission both within the community and in care-providing settings [8–11]. Further, ESBL-producing E. coli has been described to be an important cause of community-onset infections (COI) [12].
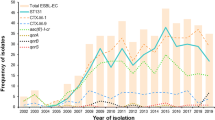
In Denmark, we have observed that the frequency of ESBL-producing E. coli and Klebsiella pneumoniae (K. pneumoniae) has risen during the last decade [13]. Earlier, we described an outbreak of ESBL-producing K. pneumoniae, where two clones that both carried blaCTX-M-15 were responsible for 77 % of all infections caused by ESBL-producing K. pneumoniae [14]. In contrast, little information is available on whether the increase observed in E. coli is caused by specific lineages or several unrelated clones, or on the epidemiological setting in which these infections are acquired.
In the present study, we evaluated an MLVA assay for the rapid typing of cefpodoxime-resistant E. coli using a benchtop capillary electrophoresis instrument for size determination. We compared the typing results obtained using MLVA with the distribution obtained using MLST. Furthermore, mechanisms accounting for cefpodoxime resistance were identified in all isolates using polymerase chain reaction (PCR) and sequencing. Finally, patient histories were reviewed to establish the epidemiological setting of infections with ESBL-producing E. coli.
Materials and methods
Strain collection
All cefpodoxime-resistant E. coli were collected at the Department of Clinical Microbiology, Hvidovre Hospital, providing diagnostic services for five hospitals and general practice in the Copenhagen area, in October 2009 (N = 67). Only a single isolate from each patient was included in the strain collection. All isolates originated from urine samples (n = 66), except for one that originated from a blood culture. E. coli resistant to cefpodoxime was identified using the disk diffusion method and all cefpodoxime-resistant isolates were further confirmed to be ESBL- or AmpC-producers using Mast D68C disks (Mast Group), following the directions of the manufacturer.
Epidemiology of ESBL-producing isolates
Patient history was reviewed using laboratory databases, the hospital information system, and demographic data. On this basis, infections were classified as community onset (COI), hospital onset (HOI), or healthcare-associated (HCAI) [15]. HOI was defined by the culture of an ESBL-producing E. coli from a sample obtained from a patient hospitalized for 48 h or longer. HCAI was defined by the culture of an ESBL-producing E. coli from a sample obtained from a patient in general practice or within 48 h after hospital admission and one or more of the following criteria have been fulfilled by the patient: (1) admitted to hospital for more than 2 days within the preceding 3 months; (2) attended an outpatient clinic within the preceding 30 days; (3) received specialized nursing care at home; (4) residence in a nursing home or long-term care facility. COI was defined by the culture of an ESBL-producing E. coli obtained from a patient in general practice or within 48 h after hospital admission where none of the criteria for HCAI were met [15].
For 15 patients, cultures prior to the one included in this study had yielded ESBL-producing E. coli. In these cases, epidemiological classification was done from the first culture yielding an ESBL-producing E. coli. The median interval between the first culture yielding an ESBL-producing E. coli and the isolate included in this study was 96.5 days (range 15–965 days).
β-Lactamase characterization
Phenotypic ESBL-producing isolates were screened by PCR for the presence of blaCTX-M, blaSHV, and blaTEM. PCR and sequencing were performed to identify specific genes, as previously described [16]. Phenotypic AmpC-producing isolates were screened for the presence of plasmid-mediated ampC (pAmpC) genes by multiplex PCR [17], followed by sequencing to identify the exact genotype. The promoter of the chromosomal ampC (cAmpC) gene was sequenced in all isolates with an AmpC phenotype and for which a pAmpC gene could not be detected by PCR in order to identify mutations associated with hyperproduction, as previously described [16].
MLVA
All isolates were typed using a modified MLVA assay originally described by Manges et al. [5]. This MLVA is based on multiplex PCR detection and size determination of eight variable number of tandem repeats (VNTR) loci using labeled primers, followed by size determination on a sequencing instrument. In this study, PCR for all targets were performed as described [5], with the exception that all reactions were done as singleplex PCR amplifications using unlabeled primers and the size of the amplified fragments was determined using an automated benchtop capillary electrophoresis system (QIAxcel, Qiagen), using a high-resolution cartridge and the accompanying BioCalculator software.
The exact sizes of the flanking regions of each locus were determined by the sequencing of MLVA PCR products from each VNTR region from selected isolates. Tandem repeats were identified by manual inspection of sequences or by the use of the tandem repeats finder [18]. The number of tandem repeats was calculated using the following equation: number of repeats = (amplicon size − flanking region)/repeat size. The isolates were sorted manually into groups according to their number of repeats. The same number of repeats in each individual locus was assigned the same value, and this was done for all loci, hereby, generating a numeric MLVA code for each isolate.
MLST
All isolates were also typed by MLST, as previously described [19]. Allele profiles and STs were assigned at the E. coli MLST homepage (http://mlst.ucc.ie/mlst/dbs/Ecoli).
Results
Validation of MLVA
PCR amplifications of all eight MLVA alleles were carried out and the size of the resulting PCR products was determined using the QIAxcel capillary electrophoresis system. For each locus, the distribution of size determinations was analyzed using frequency plots and the results were sorted into seemingly normally distributed data. The coefficient of variation (CV) for the largest clusters of data showed CV ranging between 0.7 % for VNTR-5 (mean size for the cluster: 368 bp) and 1.2 % for VNTR-1 (mean size for the cluster: 210 bp). From this analysis, it was apparent that the accuracy of the size determination using the QIAxcel system was inadequate for determining repeat numbers for locus O157-11 (repeat size: 6 bp) and O157-56 N (repeat size: 5 bp). These loci were, therefore, excluded from further analysis. The remaining six loci had repeat sizes between 12 and 95 bp.
MLVA
Using this abbreviated MLVA (a-MLVA) scheme to type the strain collection, 67/67 (100 %) isolates were typable. In all, 27 different a-MLVA types were identified and the largest cluster contained 25 isolates (37.3 %) (Table 1). Within this cluster, 22 isolates contained blaCTX-M-15, and the remaining three isolates contained blaCTX-M-14, blaCTX-M-27, and hyperproduced cAmpC, respectively (Online resource 1).
MLST
MLST was performed on the collected isolates. Using this method, 67/67 (100 %) isolates were typed and the results are summarized in Table 1. The isolates belonged to 25 different STs. The largest sequence type, ST131, contained 28 isolates (41.8 %). A number of smaller clusters were also identified. Of these, the three largest were ST405, ST448, and ST10, containing six, four, and three isolates, respectively.
When comparing a-MLVA and MLST, homologous results were found (Table 1). The major ST131 cluster identified by MLST included all the isolates identified in the major a-MLVA cluster (153562), together with three isolates, all with another a-MLVA code (153526). These two a-MLVA codes were found exclusively within the ST131 cluster. Eighteen of 25 STs had unique a-MLVA codes, i.e., the a-MLVA code was not shared with isolates with another ST. Three isolates of ST10 displayed two different a-MLVA codes; two isolates shared their a-MLVA code with the single isolate of ST167. ST167 is a single-locus variant of ST10. Two isolates of ST88 shared a-MLVA codes with the single ST410 isolate and the single ST2673 isolate. ST410 is a single-locus variant of ST88 and ST2673 is a double-locus variant of ST88. Finally, four ST448 isolates displayed two different a-MLVA codes. Two of the isolates shared their a-MLVA code with the single ST101 isolate. ST101 and ST448 are unrelated by MLST, sharing only a single allele.
Resistance mechanisms
Eleven different mechanisms of cefpodoxime resistance were identified (Table 2). Of these, blaCTX-M-15 and blaCTX-M-14 were the most commonly detected in 42/67 (62.7 %) and 7/67 (10.4 %) of the isolates, respectively. AmpC enzymes accounted for resistance in 7/67 (10.5 %) of the isolates, with cAmpC being more common [5/67 (7.5 %)] than blaCMY-2 [(2/67 (3.0 %)] (Table 2).
Epidemiology of ESBL-producing isolates
Infections caused by ESBL-producing E. coli were classified as HOI, HCAI, and COI. In all, 42/60 (76.7 %) infections were classified as healthcare-related (HCAI or HOI) and only 18/60 (23.3 %) were classified as COI (Table 3). Patients with COI were significantly younger (median age 38 years; p < 0.001, Mann–Whitney U-test) and more often female (13/14; p < 0.01, Fisher’s exact probability test) than patients with HCAI (median age 77 years and 12/28 females) or HOI (median age 78 years and 11/18 females) (Online resource 1). If stratified into infections caused by E. coli ST131 and E. coli non-ST131, the two groups did not differ in the epidemiological type of infection (Table 3).
Discussion
Typing methods that provide rapid and reliable typing results are valuable and necessary tools in the prevention and detection of outbreaks. However, many of today’s typing methods, such as pulsed-field gel electrophoresis (PFGE) and MLST, are laborious [14]. The a-MLVA described here can be used as a high-throughput assay and can provide rapid typing results compared to MLST and PFGE.
The exclusion of two loci affected the discriminatory power of the MLVA assay, making it less discriminatory than the original assay. When comparing a-MLVA typing results with MLST results, similar typing patterns were obtained, although, occasionally, more than one ST was found within an a-MLVA code. Including additional VNTR loci of sufficient repeat size can increase the discriminatory power of the MLVA assay and could possibly resolve these discrepancies. In a recently published MLVA protocol, the addition of three VNTR loci to a total of ten loci increased the number of different genotypes from 296 to 507 in a collection of 794 E. coli [20].
The a-MLVA divided the predominant ST131 lineage into two subtypes that were unique for ST131. The subdivision of ST lineages was not unexpected, as studies comparing more discriminative methods, such as PFGE with MLST, have identified several different PFGE clones within the same ST [21, 22]. As ST131 is highly prevalent, typing methods that are capable of subdividing this ST are desirable from an epidemiological point of view.
The major cause of cefpodoxime resistance in the study collection was blaCTX-M-15. This gene has also been shown to be the major cause of ESBL production in K. pneumoniae in the same region [14], and has been described worldwide to be a dominating ESBL gene [12, 23–26]. Interestingly, several cases were found where different resistance mechanisms were identified within the same STs, which could support that several different subclones within the same ST are circulating.
The epidemiological data of this study indicated the presence of two different transmission routes. Healthcare-related infections (HOI and HCAI) accounted for over three out of four ESBL-producing E. coli infections. This distribution is in contrast to a recent Canadian study, where it was reported that 130 of 209 isolates (62 %) were submitted from community collection sites, 63 (30 %) were from hospitals, and 16 (8 %) were from nursing homes [12]. However, this study did not investigate the patient history data to determine if the patients had prior hospital association, which could, together with the different geographical settings, explain the discrepancy in observed infection settings.
The different demographic characteristics of COI and healthcare-related infections may indicate that different risk factors are present in the two settings. Risk factors for infection due to ESBL-producing E. coli, such as hospitalization within the previous 3 months, age ≥65 years, male gender, comorbidity, and prior receipt of antibiotics, have been described [27–29]. However, these risk factors are mainly healthcare-related and other risk factors may be relevant for COI. Foreign travel has been identified as a risk factor for subsequent colonization and infection with ESBL-producing E. coli [30, 31]. A significant difference in the frequency of fecal carriage of ESBL-producing E. coli among different ethnic populations has also been reported [32]. This may be caused by high travel rates to and from regions with high rates of ESBL-producing E. coli [33] or differences in lifestyle or dietary habits. Studies investigating COI may, therefore, likely identify other risk factors and exposure routes than studies conducted in a hospital setting.
References
Maiden MCJ (2006) Multilocus sequence typing of bacteria. Annu Rev Microbiol 60:561–588
van Belkum A, Tassios PT, Dijkshoorn L, Haeggman S, Cookson B, Fry NK, Fussing V, Green J, Feil E, Gerner-Smidt P, Brisse S, Struelens M; European Society of Clinical Microbiology and Infectious Diseases (ESCMID) Study Group on Epidemiological Markers (ESGEM) (2007) Guidelines for the validation and application of typing methods for use in bacterial epidemiology. Clin Microbiol Infect 13(Suppl 3):1–46
Keys C, Kemper S, Keim P (2005) Highly diverse variable number tandem repeat loci in the E. coli O157:H7 and O55:H7 genomes for high-resolution molecular typing. J Appl Microbiol 98:928–940
Noller AC, McEllistrem MC, Pacheco AG, Boxrud DJ, Harrison LH (2003) Multilocus variable-number tandem repeat analysis distinguishes outbreak and sporadic Escherichia coli O157:H7 isolates. J Clin Microbiol 41:5389–5397
Manges AR, Tellis PA, Vincent C, Lifeso K, Geneau G, Reid-Smith RJ, Boerlin P (2009) Multi-locus variable number tandem repeat analysis for Escherichia coli causing extraintestinal infections. J Microbiol Methods 79:211–213
Lindstedt BA, Brandal LT, Aas L, Vardund T, Kapperud G (2007) Study of polymorphic variable-number of tandem repeats loci in the ECOR collection and in a set of pathogenic Escherichia coli and Shigella isolates for use in a genotyping assay. J Microbiol Methods 69:197–205
Pitout JD, Laupland KB (2008) Extended-spectrum beta-lactamase-producing Enterobacteriaceae: an emerging public-health concern. Lancet Infect Dis 8:159–166
Pitout JD, Gregson DB, Campbell L, Laupland KB (2009) Molecular characteristics of extended-spectrum-beta-lactamase-producing Escherichia coli isolates causing bacteremia in the Calgary Health Region from 2000 to 2007: emergence of clone ST131 as a cause of community-acquired infections. Antimicrob Agents Chemother 53:2846–2851
Rooney PJ, O’Leary MC, Loughrey AC, McCalmont M, Smyth B, Donaghy P, Badri M, Woodford N, Karisik E, Livermore DM (2009) Nursing homes as a reservoir of extended-spectrum beta-lactamase (ESBL)-producing ciprofloxacin-resistant Escherichia coli. J Antimicrob Chemother 64:635–641
Rogers BA, Sidjabat HE, Paterson DL (2011) Escherichia coli O25b-ST131: a pandemic, multiresistant, community-associated strain. J Antimicrob Chemother 66:1–14
Van der Bij AK, Peirano G, Pitondo-Silva A, Pitout JD (2012) The presence of genes encoding for different virulence factors in clonally related Escherichia coli that produce CTX-Ms. Diagn Microbiol Infect Dis 72:297–302
Peirano G, Richardson D, Nigrin J, McGeer A, Loo V, Toye B, Alfa M, Pienaar C, Kibsey P, Pitout JD (2010) High prevalence of ST131 isolates producing CTX-M-15 and CTX-M-14 among extended-spectrum-beta-lactamase-producing Escherichia coli isolates from Canada. Antimicrob Agents Chemother 54:1327–1330
Hansen DS, Frimodt-Møller N; DANRES Study Group (2009) Extended spectrum beta-lactamase producing bacteria in Danish pigs, Danish and imported retail meat and human patients. DANMAP 2009, pp. 19–21. Available online at: http://www.danmap.org/Downloads/Reports.aspx
Nielsen JB, Skov MN, Jørgensen RL, Heltberg O, Hansen DS, Schønning K (2011) Identification of CTX-M15-, SHV-28-producing Klebsiella pneumoniae ST15 as an epidemic clone in the Copenhagen area using a semi-automated Rep-PCR typing assay. Eur J Clin Microbiol Infect Dis 30:773–778
Friedman ND, Kaye KS, Stout JE, McGarry SA, Trivette SL, Briggs JP, Lamm W, Clark C, MacFarquhar J, Walton AL, Reller LB, Sexton DJ (2002) Health care-associated bloodstream infections in adults: a reason to change the accepted definition of community-acquired infections. Ann Intern Med 137:791–797
Jørgensen RL, Nielsen JB, Friis-Møller A, Fjeldsøe-Nielsen H, Schønning K (2010) Prevalence and molecular characterization of clinical isolates of Escherichia coli expressing an AmpC phenotype. J Antimicrob Chemother 65:460–464
Pérez-Pérez FJ, Hanson ND (2002) Detection of plasmid-mediated AmpC beta-lactamase genes in clinical isolates by using multiplex PCR. J Clin Microbiol 40:2153–2162
Benson G (1999) Tandem repeats finder: a program to analyze DNA sequences. Nucleic Acids Res 27:573–580
Wirth T, Falush D, Lan R, Colles F, Mensa P, Wieler LH, Karch H, Reeves PR, Maiden MC, Ochman H, Achtman M (2006) Sex and virulence in Escherichia coli: an evolutionary perspective. Mol Microbiol 60:1136–1151
Løbersli I, Haugum K, Lindstedt BA (2012) Rapid and high resolution genotyping of all Escherichia coli serotypes using 10 genomic repeat-containing loci. J Microbiol Methods 88:134–139
Novais A, Pires J, Ferreira H, Costa L, Montenegro C, Vuotto C, Donelli G, Coque TM, Peixe L (2012) Characterization of globally spread Escherichia coli ST131 isolates (1991 to 2010). Antimicrob Agents Chemother 56:3973–3976
Lau SH, Kaufmann ME, Livermore DM, Woodford N, Willshaw GA, Cheasty T, Stamper K, Reddy S, Cheesbrough J, Bolton FJ, Fox AJ, Upton M (2008) UK epidemic Escherichia coli strains A–E, with CTX-M-15 beta-lactamase, all belong to the international O25:H4-ST131 clone. J Antimicrob Chemother 62:1241–1244
Severin JA, Mertaniasih NM, Kuntaman K, Lestari ES, Purwanta M, Lemmens-Den Toom N, Duerink DO, Hadi U, van Belkum A, Verbrugh HA, Goessens WH; Study Group ‘Antimicrobial Resistance in Indonesia: Prevalence and Prevention’ (AMRIN) (2010) Molecular characterization of extended-spectrum beta-lactamases in clinical Escherichia coli and Klebsiella pneumoniae isolates from Surabaya, Indonesia. J Antimicrob Chemother 65:465–469
Kiratisin P, Apisarnthanarak A, Laesripa C, Saifon P (2008) Molecular characterization and epidemiology of extended-spectrum-beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae isolates causing health care-associated infection in Thailand, where the CTX-M family is endemic. Antimicrob Agents Chemother 52:2818–2824
Önnberg A, Mölling P, Zimmermann J, Söderquist B (2011) Molecular and phenotypic characterization of Escherichia coli and Klebsiella pneumoniae producing extended-spectrum β-lactamases with focus on CTX-M in a low-endemic area in Sweden. APMIS 119:287–295
Lascols C, Hackel M, Hujer AM, Marshall SH, Bouchillon SK, Hoban DJ, Hawser SP, Badal RE, Bonomo RA (2012) Using nucleic acid microarrays to perform molecular epidemiology and detect novel β-lactamases: a snapshot of extended-spectrum β-lactamases throughout the world. J Clin Microbiol 50:1632–1639
Ben-Ami R, Rodríguez-Baño J, Arslan H, Pitout JD, Quentin C, Calbo ES, Azap OK, Arpin C, Pascual A, Livermore DM, Garau J, Carmeli Y (2009) A multinational survey of risk factors for infection with extended-spectrum beta-lactamase-producing enterobacteriaceae in nonhospitalized patients. Clin Infect Dis 49:682–690
Rodríguez-Baño J, Picón E, Gijón P, Hernández JR, Cisneros JM, Peña C, Almela M, Almirante B, Grill F, Colomina J, Molinos S, Oliver A, Fernández-Mazarrasa C, Navarro G, Coloma A, López-Cerero L, Pascual A (2010) Risk factors and prognosis of nosocomial bloodstream infections caused by extended-spectrum-beta-lactamase-producing Escherichia coli. J Clin Microbiol 48:1726–1731
Cornejo-Juárez P, Pérez-Jiménez C, Silva-Sánchez J, Velázquez-Acosta C, González-Lara F, Reyna-Flores F, Sánchez-Pérez A, Volkow-Fernández P (2012) Molecular analysis and risk factors for Escherichia coli producing extended-spectrum β-lactamase bloodstream infection in hematological malignancies. PLoS One 7:e35780
Freeman JT, McBride SJ, Heffernan H, Bathgate T, Pope C, Ellis-Pegler RB (2008) Community-onset genitourinary tract infection due to CTX-M-15-producing Escherichia coli among travelers to the Indian subcontinent in New Zealand. Clin Infect Dis 47:689–692
Tängdén T, Cars O, Melhus A, Löwdin E (2010) Foreign travel is a major risk factor for colonization with Escherichia coli producing CTX-M-type extended-spectrum beta-lactamases: a prospective study with Swedish volunteers. Antimicrob Agents Chemother 54:3564–3568
Wickramasinghe NH, Xu L, Eustace A, Shabir S, Saluja T, Hawkey PM (2012) High community faecal carriage rates of CTX-M ESBL-producing Escherichia coli in a specific population group in Birmingham, UK. J Antimicrob Chemother 67:1108–1113
Hawser SP, Bouchillon SK, Hoban DJ, Badal RE, Hsueh PR, Paterson DL (2009) Emergence of high levels of extended-spectrum-beta-lactamase-producing gram-negative bacilli in the Asia-Pacific region: data from the Study for Monitoring Antimicrobial Resistance Trends (SMART) program, 2007. Antimicrob Agents Chemother 53:3280–3284
Acknowledgment
This work was supported by Fondation Idella (3.3.5/2008/II to K.S.), Fonden til Lægevidenskabens Fremme (10–316 to K.S.), and Hvidovre Hospitals Forskningsfond (grant to J.B.N.).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Online resource 1
(PDF 39 kb)
Rights and permissions
About this article
Cite this article
Nielsen, J.B., Albayati, A., Jørgensen, R.L. et al. An abbreviated MLVA identifies Escherichia coli ST131 as the major extended-spectrum β-lactamase-producing lineage in the Copenhagen area. Eur J Clin Microbiol Infect Dis 32, 431–436 (2013). https://doi.org/10.1007/s10096-012-1764-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-012-1764-x