Abstract
We aimed to determine the effects of enteral supplementation of a prebiotic mixture of neutral and acidic oligosaccharides (scGOS/lcFOS/pAOS) on the faecal microbiota and microenvironment in preterm infants. Furthermore, we determined the influence of perinatal factors on the development of the faecal microbiota. In a randomised controlled trial, preterm infants with gestational age <32 weeks and/or birth weight <1,500 g received enteral supplementation of scGOS/lcFOS/pAOS or placebo (maltodextrin) between days 3 and 30 of life. Faecal microbiota, as measured with fluorescent in situ hybridisation (FISH), and microenvironment [short-chain fatty acids (SCFAs), pH, sIgA] were measured at four time points: before the start of the study and at days 7, 14 and 30 of life. In total, 113 preterm infants were included. Enteral supplementation of the prebiotic mixture increased the total bacteria count at day 14 (Exp 3.92; 95 % confidence interval [CI] 1.18–13.04, p = 0.03), but not at day 30 (Exp 1.73; 95 % CI 0.60–5.03, p = 0.31). There was a trend toward increased bifidobacteria counts. There was a delayed intestinal colonisation of all bacteria. Enteral supplementation of the prebiotic mixture decreased the faecal pH (Exp 0.71; 95 % CI 0.54–0.93, p = 0.01) and there was a trend toward increased acetic acid compared to the placebo group (Exp 1.09; 95 % CI 0.99–1.20, p = 0.10). There was no effect on sIgA (Exp 1.94; 95 % CI 0.28–13.27, p = 0.50). Antibiotics decreased the total bacteria count (Exp 0.13; 95 % CI 0.08–0.22, p < 0.001). Enteral supplementation of a prebiotic mixture of neutral and acidic oligosaccharides increases the postnatal intestinal colonisation. However, the extensive use of broad-spectrum antibiotics in preterm infants decreased the growth of all intestinal microbiota, thereby, delaying the normal microbiota development.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The intestinal microbiota plays a pivotal role in the susceptibility of preterm infants for serious infections [1]. In preterm infants, intestinal colonisation is delayed compared with term infants [2]. The use of broad-spectrum antibiotics on the neonatal intensive care unit (NICU) further delay the intestinal colonisation [2]. The intestinal microbiota communicates extensively with the intestinal immune system, leading to metabolic and immunologic reactions by the epithelial cells and the underlying lymphoid cells; this is called the bacterial–epithelial ‘cross-talk’ [3]. To improve the outcome of preterm infants, modulating the intestinal microbiota with oligosaccharides early in life may be an important target. Over 200 human milk oligosaccharides have been identified, with significant variability in the composition of human milk oligosaccharides between individuals over time [4]. Human milk oligosaccharides pass unabsorbed and undigested through the small intestine into the colon, where they are fermented by resident bacteria to yield the main end products: short-chain fatty acids (SCFAs) and lactic acid [5]. By fermentation of human milk oligosaccharides, the intestinal microbiota creates a specific microenvironment with a lower pH, which supports the colonisation of fermentative bacteria (e.g. lactobacilli and bifidobacteria) and is less favourable for Enterobacteriaceae and other potential pathogenic species [6, 7]. Specific dietary milk oligosaccharides such as short-chain galacto-oligosaccharides (scGOS) and long-chain fructo-oligosaccharides (lcFOS) are used to substitute the functions of human milk oligosaccharides to stimulate a specific microbiota composition and activity [5]. In previous studies in preterm infants, the supplementation of neutral oligosaccharides increased the growth of bifidobacteria and lactobacilli and decreased the growth of pathogens in the intestine [6].
Of human milk oligosaccharides, approximately 80 % are neutral and 20 % are acidic [5]. Specific acidic oligosaccharides can be derived from pectin (pAOS). pAOS are able to act as receptor analogs and inhibit the adhesion of pathogens on the epithelial surface [5]. Recently, we found that enteral supplementation of a prebiotic mixture of specific neutral oligosaccharides (scGOS/lcFOS, 9:1) and acidic oligosaccharides (pAOS), if given in sufficient amounts, decreased the incidence of serious infections, especially endogenous infections [8]. We hypothesise that the previously found lower endogenous infection rate in preterm infants receiving a prebiotic mixture with neutral and acidic oligosaccharides may originate from an improved microenvironment of the gastro-intestinal tract with increased numbers of bifidobacteria and lower numbers of potentially pathogenic bacteria. Therefore, the aims of our study were to measure the effect of enteral supplementation of this type of prebiotic mixture on the faecal microbiota and microenvironment, reflected by SCFAs, lactate acid, pH and secretory IgA (sIgA) [9–12]. In addition, we determined the influence of perinatal factors on the development of the faecal microbiota in preterm infants.
Methods
Subjects
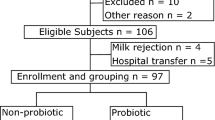
Infants with gestational age (GA) <32 weeks and/or birth weight (BW) <1,500 g, admitted to the level III NICU of the VU University Medical Center, Amsterdam, the Netherlands, were eligible for participation in the study. Exclusion criteria were: infants with GA >34 weeks, major congenital or chromosomal anomalies, death <48 h after birth and transfer to another hospital <48 h after birth. The medical ethical review board of our hospital approved the study protocol. Written informed consent was obtained from all parents.
Randomisation, blinding and treatment
The infants were randomly allocated <48 h after birth to receive either enteral 80 % scGOS/lcFOS (9:1) and 20 % pAOS or placebo powder (maltodextrin), as previously described [8]. The randomisation code was broken after data analysis was performed. Prebiotic mixture and placebo powder (maltodextrin) were prepared and packed under nitrogen environment in sachets (Danone Research, Friedrichsdorf, Germany). During the study period, prebiotics and placebo powder were monitored for stability and microbiological contamination. Supplementation of the prebiotic mixture or placebo was administered in increasing doses between days 3 and 30 of life to 1.5 g/kg/day to breast milk or preterm formula (without oligosaccharides). When infants were transferred to another hospital before the end of the study, the protocol was continued under the supervision of the principal investigator (E.A.M.W.).
Enumeration of faecal microbiota by fluorescent in situ hybridisation
Faecal sample preparation and fluorescent in situ hybridisation (FISH) analysis were performed as previously described [13], with minor modifications. All seven of the probes used, normally representing the major groups of micro-organisms in term infants, were commercially synthesised and 5′-labelled with Cy3 (Biolegio BV, Nijmegen, the Netherlands) (Table 1). For total cell counts, slides were counterstained with 4′,6-diamidino-2-phenylindole (DAPI). Slides were counted by an automated Olympus AX70 epifluorescence microscope. The percentage of labelled bacteria per sample was determined by counting all cells and all labelled bacteria in the same field with a DAPI filter set (SP100) and CY3 filter set (41007), respectively (Chroma Technology Corp., Brattleboro, VT, USA).
pH measurements
Faecal samples were collected in sterile tubes and stored at −20 °C until analysis. Prior to analysis, faecal samples were thawed in ice water and the pH was measured directly, as previously described [14].
SCFA and lactate analysis
Lactate and the SCFA acetic, propionic, n-butyric, isobutyric and n-valeric acids were measured as previously described [14].
Measurement of sIgA response by ELISA
sIgA was measured by specific enzyme-linked immunosorbent assay (ELISA) assays, as previously described [9].
Nutritional support
Parenteral and enteral nutrition was introduced at our NICU according to clinical evidence-based guidelines [8].
Statistical analysis
The sample size was based on sample size calculations for the primary outcome of the trial. Normally distributed and non-parametric data are presented as means [± standard deviation (SD)] and medians (ranges), respectively. Patient and nutritional characteristics were compared with Student’s t-test, Mann–Whitney U-test, Chi-square test or Fisher’s exact test, as appropriate. Generalised estimating equations (GEE) were used to compare changes in the faecal microbiota and microenvironment over time between the groups. In additional GEE analyses, adjustments were made for chorioamnionitis, GA, BW, mode of delivery, Apgar score at 5 min <6, exclusively breast milk feeding, stay at an NICU or general hospital ward, serious endogenous infection, postnatal antibiotic treatment (<48 h preceding the sample) and necrotising enterocolitis (NEC).
The effect of perinatal factors on the development of the intestinal microbiota was analysed by GEE. A natural logarithm transformation was performed in not normally distributed variables. All statistical analyses were performed on an intention-to-treat basis. A two-tailed p-value <0.05 was considered to be significant. SPSS 17.0 (SPSS Inc., Chicago, IL, USA) was used for the data analysis.
Results
Between May 2007 and November 2008, 113 preterm infants were entered into the study. The baseline patient and nutritional characteristics were not different in the prebiotic mixture (n = 55) and placebo group (n = 58) [8]. Faecal samples were collected at 43.8 ± 26.5 h (t = 0) after birth, at postnatal days 7.4 ± 0.9 (t = 1), 14.1 ± 0.8 (t = 2) and 30.0 ± 0.7 (t = 3). The percentage of missing faecal samples was not different in both groups: on average, at t = 0, 18 %; at t = 1, 16 %; at t = 2, 13 %; and at t = 3, 12 %. The main reasons for missing samples were death or exclusion before the end of the study period, no faecal sample available or too small a sample size of faecal sample.
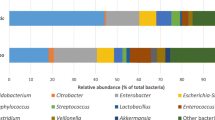
Faecal microbiota
The faecal colonisation increased at t = 3 in both groups (Exp 35.41; 95 % confidence interval [CI] 15.82–79.24, p < 0.001) (Fig. 1). Enteral supplementation of the prebiotic mixture enhanced the increase of postnatal faecal colonisation from t = 0 to t = 2 (Exp 3.92; 95 % CI 1.18–13.04, p = 0.03), but not to t = 3 (Exp 1.73; 95 % CI 0.60–5.03, p = 0.31) compared with the placebo group (Fig. 1). Adjustment for potentially confounding factors (see Methods) did not change the result of the primary analysis. Therefore, we only report the results of the primary analysis.
Enteral supplementation of the prebiotic mixture did not affect the intestinal colonisation of specific bacterial groups (Table 2). There was a trend toward increased bifidobacteria counts after enteral supplementation with the prebiotic mixture. As the results of specific bacterial groups in both groups were not different, the data of both groups were combined in order to analyse the role of perinatal factors on the development of the faecal microbiota (Table 3). Antibiotics delayed faecal colonisation, especially at day 30 (Table 4).
Faecal microenvironment
Faecal pH
The faecal pH decreased from t = 0 to t = 3 in both groups (Exp 0.62; 95 % CI 0.51–0.76, p = 0.001). Enteral supplementation of the prebiotic mixture enhanced the decrease of the faecal pH from t = 0 to t = 3 compared with the placebo group (Exp 0.71; 95 % CI 0.54–0.93, p = 0.01) (Table 2).
Faecal sIgA
The faecal sIgA increased from t = 0 to t = 3 in both groups (Exp 31.36; 95 % CI 9.15–107.53, p < 0.001). There was no effect of enteral supplementation of the prebiotic mixture on the faecal sIgA (Exp 1.94; 95 % CI 0.28–13.27, p = 0.50) (Table 2)
Faecal SCFAs and lactate
Both D-lactate and L-lactate increased from t = 0 to t = 3 (Exp 2.30; 95 % CI 1.35–3.92, p = 0.002 and Exp 2.27; 95 % CI 1.32–3.90, p = 0.003, respectively). Enteral supplementation of the prebiotic mixture had no effect on D-lactate (Exp 1.50; 95 % CI 0.70–3.22, p = 0.30) and L-lactate (Exp 1.55; 95 % CI 0.70–3.46, p = 0.28).
The total SCFAs increased from t = 0 to t = 3 (Exp 2.62; 95 % CI 1.95–3.53 p < 0.001). Acetic acid was the major SCFA in both groups at all time points. There was a trend towards increased acetic acid after enteral supplementation of the prebiotic mixture from t = 0 to t = 3 compared with the placebo group (Exp 1.09; 95 % CI 0.99–1.20, p = 0.10) (Table 2).
Discussion
In our study, a prebiotic mixture consisting of neutral and acidic oligosaccharides increased the postnatal intestinal colonisation, as measured with FISH, until day 14 and decreased the faecal pH. There was a trend toward increased bifidobacteria counts and increased acetic acid, and no effect on the faecal sIgA.
The development of the intestinal microbiota was characterised by large interindividual differences in terms of both composition and counts. In general, the initial total bacteria count was low and increased over time, in line with previous studies using molecular techniques in preterm infants [15–19]. However, with FISH analysis, we measured only seven groups among the most common bacterial groups in neonates. Novel molecular techniques, such as IS-Pro, will enable to detect almost all types of intestinal bacteria [20].
Host-, treatment- and nutrition-related factors play a role in the development of the intestinal microbiota. In our study, broad-spectrum antibiotics decreased the total bacteria count of all specific bacteria groups, especially at day 30. This is in line with previous studies in preterm and term infants [2, 19, 21]. We speculate that the use of broad-spectrum antibiotics in preterm infants decreases the growth of all intestinal bacteria, counteracting the beneficial effect of prebiotics on the growth of (health-promoting) bacteria. The fact that broad-spectrum antibiotics decreased bacterial growth especially at day 30 may explain why the increased intestinal colonisation in the prebiotic mixture group did not persist till day 30. We hypothesise that the negative effect of antibiotics on the intestinal microbiota is larger when the total bacterial count is higher. Antibiotics may also negatively interact with the bacterial–epithelial ‘cross-talk’, and, subsequently, negatively influence the immune system, leading to increased risk of NEC or death [22] and the development of asthma [23].
Furthermore, delivery by caesarean section, birth weight and stay at a NICU decreased the postnatal total bacterial count in our study. In term infants, delivery by caesarean section is associated with less diverse faecal microbiota, with delayed colonisation with bifidobacteria and Bacteroides, and increased numbers of Clostridium difficile compared with vaginally delivery [24]. In preterm infants, the effect of the mode of delivery is less clear [18, 19]. We speculate that this is related to low total bacteria count directly after preterm birth amongst others due to high maternal antibiotic use. Furthermore, the use of broad-spectrum antibiotics directly postpartum may counteract the beneficial effect of vaginal delivery. The mode of delivery and its effect on early intestinal colonisation may decrease atopic diseases later in life [25]. Follow-up of our cohort of preterm infants is important to determine the development of atopic diseases.
Increased level of total bacteria count of infants staying at a general hospital ward may reflect the clinical condition of the infants, but also that stay at different hospital wards influences the intestinal colonisation [15].
In term infants, combined supplementation of neutral and acidic oligosaccharides, but not of acidic oligosaccharides alone, increased the levels of faecal bifidobacteria and lactobacilli [26]. Due to delayed intestinal colonisation and immaturity of the host immune defence system and increased intestinal permeability, potentially pathogenic bacteria may translocate from the intestinal lumen and cause systemic infections [27]. Therefore, we hypothesise that especially the combination of neutral and acidic oligosaccharides may prevent bacterial translocation of potentially pathogenic bacteria that may cause systemic infections.
In our study, the stool pH decreased after enteral supplementation of the prebiotic mixture. Although the prebiotic mixture did not increase the total SCFA levels and concentration of lactate acid, there was a trend toward increased concentration of acetic acid. Acetic acid produced by bifidobacteria improves intestinal defence mediated by epithelial cells and, thereby, protects the host against lethal infection [10]. Breast-fed infants have an SCFA pattern dominated by acetic acid, mainly produced by acid-producing bacteria, such as bifidobacteria [11]. Butyric acid is mainly produced by anaerobes, e.g. Clostridium and Bacteroides species, and may be harmful, contributing to the pathogenesis of NEC [28]. In term formula-fed infants, the enteral supplementation of neutral oligosaccharides produced a faecal SCFA pattern similar to breast-fed infants [29]. Decreased stool pH and increased acetic acid suggest an improved intestinal microenvironment which may favour the ‘bifidogenic’ effect of prebiotic supplementation. Furthermore, we found a trend toward increased levels of bifidobacteria at day 30 after enteral supplementation of the prebiotic mixture. These findings may, at least partly, contribute to the previously found lower infection rate after enteral supplementation of the prebiotic mixture [8].
sIgA plays a key role in the gastrointestinal defence mechanism against dietary and microbial agents, and is influenced by the intestinal microbiota [12]. High faecal sIgA is associated with decreased IgE-associated allergic diseases and, in preterm and term infants, faecal sIgA is higher in breast-fed than in formula-fed infants [30]. In term formula-fed infants, the supplementation of neutral oligosaccharides may increase the faecal sIgA [9, 12]. However, we found no effect of the prebiotic mixture on the faecal sIgA. We hypothesise that the absence of this effect may be due to immaturity of the mucosal surface of preterm infants, suppression of mucosal sIgA production by sIgA of breast milk and/or a too low total intestinal bacteria count to induce the production of sIgA.
Some remarks may be formulated with regard to the methodology of our study. First, the sample size calculation was based on the primary outcome of the main trial. Therefore, the sample size may have been insufficient to detect significant differences in the intestinal microbiota. Second, breast milk itself contains neutral and acidic oligosaccharides. Therefore, the effect of enteral supplemented prebiotic mixture may be less pronounced in preterm infants with exclusively human milk (60 %) than with exclusively formula (20 %) feeding. However, in additional analysis, adjustment for the type of feeding did not change the results of the primary analysis on the effect of neutral and acidic oligosaccharides on the intestinal microbiota. Third, as 75 % of our infants received direct postnatal broad-spectrum antibiotics, enteral supplementation of prebiotics during a period of 28 days may be too short to have a significant effect. Furthermore, as the optimal supplementation dose of 1.5 g/kg/day was reached at 11 days, and the median age at first endogenous infection was 16 days [8], the supplementation of prebiotics should preferably be started directly after birth.
In conclusion, enteral supplementation with a prebiotic mixture consisting of neutral and acidic oligosaccharides in preterm infants during a period of 28 days increases the intestinal colonisation, with a trend toward increased growth of bifidobacteria. However, the use of broad-spectrum antibiotics in preterm infants decreased the growth of all intestinal microbiota and may negatively influence the normal microbiota development and interfere with the bacterial–epithelial ‘cross-talk’ necessary for normal gut development.
References
Neish AS (2009) Microbes in gastrointestinal health and disease. Gastroenterology 136:65–80
Westerbeek EA, van den Berg A, Lafeber HN et al (2006) The intestinal bacterial colonisation in preterm infants: a review of the literature. Clin Nutr 25:361–368
Lu L, Walker WA (2001) Pathologic and physiologic interactions of bacteria with the gastrointestinal epithelium. Am J Clin Nutr 73:1124S–1130S
Niñonuevo MR, Lebrilla CB (2009) Mass spectrometric methods for analysis of oligosaccharides in human milk. Nutr Rev 67(Suppl 2):S216–S226
Boehm G, Moro G (2008) Structural and functional aspects of prebiotics used in infant nutrition. J Nutr 138:1818S–1828S
Knol J, Boehm G, Lidestri M et al (2005) Increase of faecal bifidobacteria due to dietary oligosaccharides induces a reduction of clinically relevant pathogen germs in the faeces of formula-fed preterm infants. Acta Paediatr Suppl 94:31–33
Sherman PM, Cabana M, Gibson GR et al (2009) Potential roles and clinical utility of prebiotics in newborns, infants, and children: proceedings from a global prebiotic summit meeting, New York City, June 27–28, 2008. J Pediatr 155:S61–S70
Westerbeek EA, van den Berg JP, Lafeber HN et al (2010) Neutral and acidic oligosaccharides in preterm infants: a randomized, double-blind, placebo-controlled trial. Am J Clin Nutr 91:679–686
Scholtens PA, Alliet P, Raes M et al (2008) Fecal secretory immunoglobulin A is increased in healthy infants who receive a formula with short-chain galacto-oligosaccharides and long-chain fructo-oligosaccharides. J Nutr 138:1141–1147
Fukuda S, Toh H, Hase K et al (2011) Bifidobacteria can protect from enteropathogenic infection through production of acetate. Nature 469:543–547
Edwards CA, Parrett AM, Balmer SE et al (1994) Faecal short chain fatty acids in breast-fed and formula-fed babies. Acta Paediatr 83:459–462
Bakker-Zierikzee AM, Tol EA, Kroes H et al (2006) Faecal SIgA secretion in infants fed on pre- or probiotic infant formula. Pediatr Allergy Immunol 17:134–140
Thiel R, Blaut M (2005) An improved method for the automated enumeration of fluorescently labelled bacteria in human faeces. J Microbiol Methods 61:369–379
Bakker-Zierikzee AM, Alles MS, Knol J et al (2005) Effects of infant formula containing a mixture of galacto- and fructo-oligosaccharides or viable Bifidobacterium animalis on the intestinal microflora during the first 4 months of life. Br J Nutr 94:783–790
Schwiertz A, Gruhl B, Löbnitz M et al (2003) Development of the intestinal bacterial composition in hospitalized preterm infants in comparison with breast-fed, full-term infants. Pediatr Res 54:393–399
Butel MJ, Suau A, Campeotto F et al (2007) Conditions of bifidobacterial colonization in preterm infants: a prospective analysis. J Pediatr Gastroenterol Nutr 44:577–582
Magne F, Abély M, Boyer F et al (2006) Low species diversity and high interindividual variability in faeces of preterm infants as revealed by sequences of 16S rRNA genes and PCR-temporal temperature gradient gel electrophoresis profiles. FEMS Microbiol Ecol 57:128–138
Mshvildadze M, Neu J, Shuster J et al (2010) Intestinal microbial ecology in premature infants assessed with non-culture-based techniques. J Pediatr 156:20–25
van den Berg A, van Elburg RM, Westerbeek EA et al (2007) The effect of glutamine-enriched enteral nutrition on intestinal microflora in very low birth weight infants: a randomized controlled trial. Clin Nutr 26:430–439
Budding AE, Grasman ME, Lin F et al (2010) IS-pro: high-throughput molecular fingerprinting of the intestinal microbiota. FASEB J 24:4556–4564
Tanaka S, Kobayashi T, Songjinda P et al (2009) Influence of antibiotic exposure in the early postnatal period on the development of intestinal microbiota. FEMS Immunol Med Microbiol 56:80–87
Cotten CM, Taylor S, Stoll B et al (2009) Prolonged duration of initial empirical antibiotic treatment is associated with increased rates of necrotizing enterocolitis and death for extremely low birth weight infants. Pediatrics 123:58–66
Sobko T, Schiött J, Ehlin A et al (2010) Neonatal sepsis, antibiotic therapy and later risk of asthma and allergy. Paediatr Perinat Epidemiol 24:88–92
Biasucci G, Rubini M, Riboni S et al (2010) Mode of delivery affects the bacterial community in the newborn gut. Early Hum Dev 86(Suppl 1):13–15
Salminen S, Gibson GR, McCartney AL et al (2004) Influence of mode of delivery on gut microbiota composition in seven year old children. Gut 53:1388–1389
Fanaro S, Jelinek J, Stahl B et al (2005) Acidic oligosaccharides from pectin hydrolysate as new component for infant formulae: effect on intestinal flora, stool characteristics, and pH. J Pediatr Gastroenterol Nutr 41:186–190
Duffy LC (2000) Interactions mediating bacterial translocation in the immature intestine. J Nutr 130:432S–436S
Waligora-Dupriet AJ, Dugay A, Auzeil N et al (2009) Short-chain fatty acids and polyamines in the pathogenesis of necrotizing enterocolitis: kinetics aspects in gnotobiotic quails. Anaerobe 15:138–144
Boehm G, Jelinek J, Stahl B et al (2004) Prebiotics in infant formulas. J Clin Gastroenterol 38:S76–S79
Kuitunen M, Savilahti E (1995) Mucosal IgA, mucosal cow’s milk antibodies, serum cow’s milk antibodies and gastrointestinal permeability in infants. Pediatr Allergy Immunol 6:30–35
Acknowledgements
We are indebted to the parents for allowing their infants to participate in the study. Furthermore, we thank the medical and nursing staff of the neonatal intensive care unit of the VU University Medical Center and all the participating hospitals and Danone Research for the financial support and for providing the preterm formula (Nenatal Start®, Nenatal 1®) and study supplementation (acidic and neutral oligosaccharides and placebo [Maltodextrin]).
Financial disclosure
This study was supported by an unrestricted research grant from Danone®, Friedrichsdorf, Germany. Danone® also supported the manufacture of the prebiotic mixtures used in this study, but had no involvement in the analysis of the data or the interpretation of the results of this investigation. All authors approved the final version of the manuscript.
Conflict of interest
None of the authors have a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Westerbeek, E.A.M., Slump, R.A., Lafeber, H.N. et al. The effect of enteral supplementation of specific neutral and acidic oligosaccharides on the faecal microbiota and intestinal microenvironment in preterm infants. Eur J Clin Microbiol Infect Dis 32, 269–276 (2013). https://doi.org/10.1007/s10096-012-1739-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-012-1739-y