Abstract
Several protocols for direct matrix-assisted laser desorption/ionisation time-of-flight mass spectrometry (MALDI-TOF MS) from positive blood cultures are currently used to speed up the diagnostic process of bacteraemia. Identification rates are high and results are accurate for the BACTEC™ system and for charcoal-free bottles. Only a few studies have evaluated protocols for charcoal-containing BacT/ALERT bottles reaching substantially lower identification rates. We established a new protocol for sample preparation from aerobic and anaerobic positive charcoal-containing BacT/ALERT blood culture bottles and measured the protein profiles (n = 167). Then, we integrated this protocol in the routine workflow of our laboratory (n = 212). During the establishment of our protocol, 74.3 % of bacteria were correctly identified to the species level, in 23.4 %, no result and in 2.4 %, a false identification were obtained. Reliable criteria for correct species identification were a score value ≥1.400 and a best match on rank 1–3 of the same species. Identification rates during routine workflow were 77.8 % for correct identification, 20.8 % for not identified samples and 1.4 % for discordant identification. In conclusion, our results indicate that MALDI-TOF MS is possible, even from charcoal-containing blood cultures. Reliable criteria for correct species identification are a score value ≥1.400 and a best match on rank 1–3 of a single species.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Matrix-assisted laser desorption/ionisation time-of-flight mass spectrometry (MALDI-TOF MS) is an accurate diagnostic tool used in medical microbiology for the identification of cultured bacteria. The bacteria are identified based on species-specific ribosomal protein profiles. This approach is fast, reliable and cost-effective compared to traditional biochemical identification tools. Limitations of the method are due to the number of database entries per species and the phylogenetic similarity of some bacteria, e.g. Streptococcus pneumoniae and Streptococcus mitis/oralis [1, 2].
Blood cultures (BC) are one important diagnostic tool referred to in the international guidelines for the management of severe sepsis and septic shock [3]. In septic patients, an immediate start of intravenous antibiotics has great priority. However, not only the timely administration but also the appropriate choice of the antimicrobial determine the survival rates of patients with septic shock [4]. To speed up the diagnostic process of bacteraemia, several protocols have been established for the direct identification of bacteria from charcoal-free BC bottles by MALDI-TOF MS. Overall, in at least 75 % of the samples, correct identification to the species level is possible [5–7]. The type of BC system and the use of charcoal-containing BC bottles seem to influence the identification rates [8–10]. The highest identification (ID) rates were reported using the BACTEC™ system (76 % [8, 9]), followed by VersaTREK (69 % [8]), and the lowest for BacT/ALERT (62 % [8] and 28 % [9]), which is used in our university medical centre. Furthermore, in the BacT/ALERT system, direct ID of bacteria was successful in 8 % from charcoal-containing BC and in 28 % from charcoal-free bottles [9]. In the present study, we report the results of our own protocol for the direct identification of bacteria from charcoal-containing BacT/ALERT BC bottles.
Materials and methods
Step 1: Establishment of an improved protocol
A total of 167 positive aerobic BacT/ALERT FA (n = 121) and anaerobic FN (n = 46) bottles (bioMérieux, Marcy l’Etoile, France) and 10 negative aerobic BacT/ALERT FA bottles (inoculated with 10 ml of blood drawn from patients and incubated for 7 days) from our routine diagnostic laboratory were consecutively tested using the following protocol:
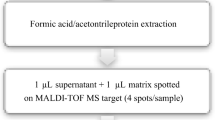
Five millilitres of BC broth were used for the sample preparation. In a first centrifugation step (10 min/400 × g), charcoal and blood cells were removed. One millilitre of the supernatant (SN) was transferred to a 1.5-ml reaction tube (Eppendorf, Hamburg, Germany), 200 μl 5 % saponin were added for cell lysis (Sigma-Aldrich, St. Louis, MO, USA) and the mixture was incubated for 5 min at room temperature. Then, the remainder of charcoal and blood cells were removed in a centrifugation step using a SigmaPrep™ spin column (800 μl, 2 min/2,000 rpm, Sigma-Aldrich, St. Louis, MO, USA). The filtrate was centrifuged for 2 min at 13,000 rpm, the SN was removed carefully and the pellet was washed in 1 ml of ultra-pure water. After another centrifugation step (1 min/13,000 rpm), the SN was discarded and the pellet was resuspended in 300 μl of ultra-pure water. Then, the standard extraction protocol recommended by the manufacturer for bacterial profiling was applied: 900 μl ethanol abs. were added and the mixture was centrifuged for 2 min at 13,000 rpm. The supernatant was discarded and the residual ethanol was removed after a second centrifugation step (2 min/13,000 rpm). The dried pellet was resuspended in 50 μl 70 % formic acid and 50 μl 100 % acetonitrile, mixed and centrifuged for 2 min at 13,000 rpm. Of the clear SN, 0.5 μl and 1 μl were spotted onto a steel target plate (Bruker Daltonik, Bremen, Germany). Each BC was tested with two spots: a 0.5-μl spot and a 1.0-μl spot. The spots were overlaid with 1 μl of matrix solution [a saturated solution of HCCA (α-cyano-4-hydroxycinnamic acid) in organic solvent (50 % acetonitrile and 2.5 % trifluoroacetic acid; Sigma-Aldrich, St. Louis, MO, USA)] and transferred to a Microflex LT instrument (Bruker Daltonik, Bremen, Germany). The protein profiles were recorded as described by Schubert et al. [6]. The results were analysed using the Biotyper 2.0 and the updated 3.0 software (Bruker Daltonik, Bremen, Germany). When direct MALDI-TOF MS from BC failed, measurement was not repeated. The protocol was performed from Monday to Friday once a day in the morning. BC detected to be positive overnight and in the morning until 10.00 a.m. were tested. Only non-duplicate BC bottles were tested per patient and study day. This part of our study was performed by two alternating technicians and supervised by one medical doctor. Mixed cultures and yeast were excluded from the analysis.
Blood culture processing
Gram stain and subculture on Columbia blood agar and Chocolate agar (aerobic FA bottles) or Columbia blood agar and Yeast Extract Cysteine agar with blood (anaerobic FN bottles) were performed from all positive BC. After incubation overnight, subcultures of bacteria were identified in parallel using standard methods, mainly the Vitek 2 automated system (69 %, bioMérieux, Marcy l’Etoile, France), clumping factor test (6 %), oxidase reaction and pigment formation (4 %), optochin susceptibility (1 %) and MALDI-TOF MS (15 %). Partial 16S rRNA gene sequencing was performed in eight cases (5 %), as described previously [11].
Step 2: Integration in the routine workflow
After the establishment of our protocol, we tested 212 positive BacT/ALERT bottles (bioMérieux, Marcy l’Etoile, France) during our routine workflow. Again, the protocol as described above was performed from Monday to Friday once a day in the morning. BC detected to be positive overnight and in the morning until 10.00 a.m. were tested. Only non-duplicate BC bottles were tested per patient and study day. There were two modifications compared to the protocol described under step 1. In contrast to the first part, positive BC bottles were processed by six alternating technicians and in about one-third of the samples, MALDI-TOF MS was used as the reference method for the species identification of the grown bacteria.
Results
Step 1: Establishment of an improved protocol (n = 167)
Direct MALDI-TOF MS from all 10 negative BC broths gave identification results with score values between 0.944 and 1.371 and 10 different bacterial species within the 10 best matched profiles. Therefore, we defined a cut-off score value of 1.400 to differentiate between a reliable result from a positive BC and a background signal caused by human proteins, charcoal or other components of the BC broth, and classified our results as follows: ‘accurate identification’ (concordance of direct ID from BC with a score value ≥1.400 and reference ID), ‘no identification’ (direct ID from BC with a score value <1.400 or ‘no peaks found’) and ‘false identification’ (discordance of direct ID from BC with a score value ≥1.400 and reference ID). Classification of the ID result as accurate ID, no ID or false ID was based on the spot (0.5 μl vs. 1 μl) with the higher score value.
Overall, 74.3 % of the isolates (n = 124) were correctly identified to the species level with our protocol. In 23.4 % (n = 39), no identification was possible and 2.4 % showed false results (n = 4). The highest rates of correct ID were obtained within the group of enterobacteriaceae (96.9 %) and non-fermenting bacteria (80 %), followed by the Staphylococcus spp. (78.5 %), Enterococcus/Streptococcus spp. (41.2 %) and the group of bacteria classified as ‘others’ (33.3 %, Table 1). The mean score values of the correctly identified samples were 2.106 for enterobacteriaceae, 2.168 for non-fermenting bacteria, 1.875 for Staphylococcus spp., 2.005 for Enterococcus/Streptococcus spp. and 1.952 for ‘others’. Four Streptococcus spp. isolates gave a discordant result by MALDI-TOF MS from the BC compared to the reference method (Table 1). One Streptococcus mitis/oralis isolate was misidentified as Streptococcus pneumoniae, which is a known limitation of MALDI-TOF MS [12]. A second Streptococcus mitis/oralis isolate was misidentified as Lactobacillus sakei (score 1.633) and one Streptococcus pneumoniae isolate was misidentified as Pseudomonas syringae (score 1.417). In both cases, the results of direct MALDI-TOF MS from BC and Gram stain were discordant. Consequently, these results were not reported to the clinician. Therefore, Gram staining from positive BC will always be mandatory [13]. The fourth isolate was Streptococcus dysgalactiae that was falsely identified as Streptococcus pyogenes (score 1.408) as the first best match, followed by Streptococcus dysgalactiae, with a similar score of 1.405 as the second best match. On the basis of these results, we introduced an additional criterion for correct ID. Besides the cut-off score value of 1.400, the number of identical species within the 10 best matched patterns was used. In 94.6 % of our correctly identified samples, the first three best matches were of the same species.
In 24 % (n = 40) of all BC, the first best match of the 0.5-μl spot showed a different result compared to the 1.0-μl spot. For classification of the ID result as accurate ID, no ID or false ID, the spot with the higher score value was used. These different ID results were mainly seen in samples where direct ID from BC failed (75 %).
When we compared the identification results of the 25 BC (15 %) where colony MALDI-TOF MS was performed for species identification of the cultured bacteria, we saw that, in 14 samples (56 %), the results of direct MALDI-TOF MS and colony MALDI-TOF MS were concordant. In 11 samples (44 %), direct MALDI-TOF MS failed, whereas MALDI-TOF MS from the cultured bacteria gave reliable identification results at the first measurement.
Step 2: Integration in the routine workflow (n = 212)
A cut-off value of ≥1.400 was used for the classification of results. Of all samples, 77.8 % were correctly identified to the species level (n = 165). In 20.8 % (n = 44), no identification was possible and three samples showed a discordant result (1.4 %). Again, the highest rates of correct ID were obtained within the group of enterobacteriaceae (96 %) and non-fermenting bacteria (80 %), followed by the Staphylococcus spp. (75.5 %), the group of bacteria classified as ‘others’ (75 %) and the Enterococcus/Streptococcus spp. (60.5 %, Table 2). Discordant results were observed within the group of staphylococci (n = 2) and non-fermenting bacteria (n = 1) (Table 2). In detail, one Staphylococcus epidermidis isolate was misidentified as Candida lusitaniae (score 1.411/only the first best matched pattern was of the same species). This ID was discordant from the result of the Gram stain and was, therefore, not reported to the clinician. Another Staphylococcus epidermidis isolate was identified as Staphylococcus aureus (score 1.709). This false result is of significant relevance to the patient, but, again, the second criterion was not fulfilled. On rank two, of the 10 best matched patterns, Staphylococcus epidermidis (score 1.5) followed. The third isolate was Pseudomonas aeruginosa, which was identified as Pseudomonas jinjuensis (score 1.496) as the first best match, followed by Pseudomonas aeruginosa (score 1.417) as the second best match.
In 23 % (n = 48) of all BC, the first best match of the 0.5-μl spot showed a different result compared to the 1.0-μl spot. For classification of the ID result as accurate ID, no ID or false ID, the spot with the higher score value was used. These different ID results were mainly seen in samples where direct ID from BC failed (75 %).
When we compared the identification results of the 74 BC (35 %), where colony MALDI-TOF MS was performed for species identification of the cultured bacteria, we saw that, in 55 samples (74 %), the results of direct MALDI-TOF MS and colony MALDI-TOF MS were concordant. In 17 samples (23 %), direct MALDI-TOF MS failed, whereas MALDI-TOF MS from the cultured bacteria gave reliable identification results at the first measurement. Two samples (3 %) showed a false ID from BC compared to colony MALDI-TOF MS. These were the two Staphylococcus epidermidis isolates described above.
The mean time of sample preparation using this protocol was 50–60 min until the samples were spotted on the target plate. The protocol is actually integrated in our routine workflow as follows: from Monday to Friday, all BC detected positive overnight and in the morning until 10.00 a.m. are tested. The BC are processed by the technician who is responsible for the BC samples or by the technician who cares for all MALDI-TOF MS samples from our routine diagnostic laboratory. There are currently six technicians in rotation. Identification results are available at about 11.00 a.m.
Discussion
We established a protocol for direct species identification from positive charcoal-containing blood culture bottles using MALDI-TOF MS. Our results indicate that direct MALDI-TOF MS is possible even from charcoal-containing BC bottles. A score value ≥1.400 and the first three best matches of a single species were found to be reliable criteria for correct ID to the species level. Correct ID rates of 74.3 and 77.8 % are considerably higher than that reported for other protocols for charcoal-containing BC bottles (studies have reported 8 % [9], 23 % [10] and no reliable results at all [14]). The correct identification rate of the integration of the protocol in our routine workflow was higher compared to the first part of our study. This might be explained by a selection bias of the samples, because when we started with the second part of our study, the results and limitations of our protocol established in the first part were known. Selection bias means that, for example, Propionibacterium might be excluded from analysis when coryneform Gram-positive rods were seen in the Gram staining of anaerobic BC and the time to positivity was ≥72 h.
The classification of score values used for bacteria cultured on solid media should be adapted for BC because score values and spectra are of lower quality [6, 15]. Nonbacterial background peaks due to human proteins, charcoal and other broth components, especially in BacT/ALERT BC, and the bacterial load might be responsible for this [10, 16]. When we applied a score value of ≥2.000 that is proposed by the manufacturer for secure genus identification and probable species identification for cultured bacteria on solid media, our rates for correct species identification from BC were only 35.3 % (n = 59) for the protocol establishment part and 34.9 % (n = 74) for the integration in the routine workflow part. Therefore, we propose for our protocol a cut-off score value of ≥1.400 for correct species ID and a best match on rank 1–3 of the same species, but further studies are needed in order to support the predictive value of this modified cut-off score. In the literature, cut-off score values used for correct species identification from BC ranged from ≥1.400 to ≥1.500 [6, 17]. Both studies recommend that three to four identical species should be listed on rank 1–3/4 of the 10 best matched patterns as additional criterion. The lower ID rates for Gram-positive bacteria in our study correspond to findings by others [7, 8, 18–20] and might be the result of the different cell wall composition of Gram-positive and Gram-negative bacteria.
In 23.4 % (step 1) and 20.8 % (step 2), no ID was possible from BC. When direct MALDI-TOF MS from BC failed, ID was not repeated. No ID failures were observed from the cultured bacteria. Moreover, all bacterial species identified in our study were included in the Bruker database. In our opinion, failures of direct MALDI-TOF MS might be explained by differences in the bacterial load, cell wall composition and background signals.
In 11 cases, we performed partial sequencing of the 16S rRNA gene for species ID because no reliable biochemical reference methods were established in our laboratory for these species (labeled with superscript ‘d’ in Tables 1 and 2). All 11 cases were correctly identified in parallel by colony MALDI-TOF MS.
Overall, seven discordant results were observed in our study, four in part 1 and three in part 2. To avoid the reporting of false ID results, the following criteria should be used: the ID result from the BC and the Gram stain should be concordant. All classification criteria should be fulfilled and the known limitations of MALDI-TOF MS apply for the blood culture protocol as well. In case the results were ambiguous, we reported results to the genus level or the Gram stain only. For example, the case where Streptococcus pyogenes (score 1.408) was the first best match followed by Streptococcus dysgalactiae (score 1.405) as the second best match, we reported beta-haemolytic streptococci to the clinician. Furthermore, direct ID of Streptococcus pneumoniae was only reported when morphology in Gram stain (Gram-positive diplococci) and clinical condition (‘pneumonia’) were compatible.
In this analysis, we included monomicrobial cultures only. Data on polymicrobial cultures and yeasts were excluded. However, in 18 of 25 polymicrobial BC bottles (72 %) that were processed during both study parts, the identification of at least one pathogen was possible and correct. In contrast, no identification was obtained from the four BC positive for yeasts (data not shown).
Our protocol is more labourious and the turnaround time is longer compared to other protocols [5, 6], but the results are accurate and reliable. Identification results are available within one hour and allow a more focussed empiric antibiotic therapy compared to conventional BC processing. We did not measure the mean and standard deviation of delay for proceeding exactly because our priority was the implementation of a protocol for direct MALDI-TOF MS from positive BC in our laboratory, rather than the optimisation of time. We developed our protocol based on the protocol modification for charcoal-containing BC bottles of the commercial Sepsityper Kit (PI_270170_MALDI Sepsityper_V1.doc September 10, Bruker Daltonik, Bremen, Germany). To our knowledge, no evaluation of the Sepsityper protocol for charcoal-containing bottles has been published so far. When we started with direct MALDI-TOF MS from BC, we tested 47 positive monobacterial BacT/ALERT FA and FN bottles from our routine diagnostic laboratory using the Bruker Sepsityper Kit, with their modification for charcoal-containing BC (data not shown). Of the isolates tested, 27.7 % were enterobacteriaceae (n = 13), 36.2 % Staphylococcus spp. (n = 17), 25.5 % Enterococcus/Streptococcus spp. (n = 12) and 10.6 % were classified as ‘others’ (n = 5). Using the same criteria established for our own protocol, accurate ID rates were 63.8 % (n = 30). In 31.9 % (n = 15), no ID was possible and in 4.3 % (n = 2), a discordant ID was observed. Especially, the high rate of samples where direct ID failed (31.9 %) was the reason for the development of an improved protocol. Compared to the Sepsityper protocol, we added one centrifugation step at the beginning. We started with a higher volume (5 vs. 1 ml) and reduced in a first low-speed centrifugation step human blood cells and charcoal particles in order to obtain a lower background signal. Then, we used 1 ml of the supernatant for our protocol. No major problems occurred when we integrated the protocol in the routine workflow. All six technicians succeeded in the application of the protocol. Currently, we offer this test from Monday to Friday once a day in the morning. What we have to discuss in the future is whether we can offer this test on weekends and perform a second run per day. That direct MALDI-TOF MS from positive BC bottles has the potential to speed up the diagnostic process of bacteraemia was shown by Buchan et al. [21]. Despite that, the cultivation of bacteria from BC is still mandatory for standardised susceptibility testing. The next step would be to investigate the influence of identification results on empiric antibiotic therapy and clinical outcome of the patients.
In conclusion, keeping its limitations in mind, MALDI-TOF MS is a fast and accurate tool for direct species identification, even from positive charcoal-containing BC bottles.
References
Seng P, Drancourt M, Gouriet F, La Scola B, Fournier PE, Rolain JM, Raoult D (2009) Ongoing revolution in bacteriology: routine identification of bacteria by matrix-assisted laser desorption ionization time-of-flight mass spectrometry. Clin Infect Dis 49(4):543–551
Bizzini A, Greub G (2010) Matrix-assisted laser desorption ionization time-of-flight mass spectrometry, a revolution in clinical microbial identification. Clin Microbiol Infect 16(11):1614–1619
Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, Reinhart K, Angus DC, Brun-Buisson C, Beale R, Calandra T, Dhainaut JF, Gerlach H, Harvey M, Marini JJ, Marshall J, Ranieri M, Ramsay G, Sevransky J, Thompson BT, Townsend S, Vender JS, Zimmerman JL, Vincent JL (2008) Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med 36(1):296–327
Kumar A, Ellis P, Arabi Y, Roberts D, Light B, Parrillo JE, Dodek P, Wood G, Kumar A, Simon D, Peters C, Ahsan M, Chateau D (2009) Initiation of inappropriate antimicrobial therapy results in a fivefold reduction of survival in human septic shock. Chest 136(5):1237–1248
Drancourt M (2010) Detection of microorganisms in blood specimens using matrix-assisted laser desorption ionization time-of-flight mass spectrometry: a review. Clin Microbiol Infect 16(11):1620–1625
Schubert S, Weinert K, Wagner C, Gunzl B, Wieser A, Maier T, Kostrzewa M (2011) Novel, improved sample preparation for rapid, direct identification from positive blood cultures using matrix-assisted laser desorption/ionization time-of-flight (MALDI-TOF) mass spectrometry. J Mol Diagn 13(6):701–706
Kok J, Thomas LC, Olma T, Chen SC, Iredell JR (2011) Identification of bacteria in blood culture broths using matrix-assisted laser desorption-ionization Sepsityper™ and time of flight mass spectrometry. PLoS One 6(8):e23285
Romero-Gómez MP, Mingorance J (2011) The effect of the blood culture bottle type in the rate of direct identification from positive cultures by matrix-assisted laser desorption/ionisation time-of-flight (MALDI-TOF) mass spectrometry. J Infect 62(3):251–253
Szabados F, Michels M, Kaase M, Gatermann S (2011) The sensitivity of direct identification from positive BacT/ALERT™ (bioMérieux) blood culture bottles by matrix-assisted laser desorption ionization time-of-flight mass spectrometry is low. Clin Microbiol Infect 17(2):192–195
Schmidt V, Jarosch A, März P, Sander C, Vacata V, Kalka-Moll W (2012) Rapid identification of bacteria in positive blood culture by matrix-assisted laser desorption ionization time-of-flight mass spectrometry. Eur J Clin Microbiol Infect Dis 31(3):311–317
Sander A, Ruess M, Bereswill S, Schuppler M, Steinbrueckner B (1998) Comparison of different DNA fingerprinting techniques for molecular typing of Bartonella henselae isolates. J Clin Microbiol 36(10):2973–2981
Stevenson LG, Drake SK, Murray PR (2010) Rapid identification of bacteria in positive blood culture broths by matrix-assisted laser desorption ionization-time of flight mass spectrometry. J Clin Microbiol 48(2):444–447
Fuglsang-Damgaard D, Nielsen CH, Mandrup E, Fuursted K (2011) The use of Gram stain and matrix-assisted laser desorption ionization time-of-flight mass spectrometry on positive blood culture: synergy between new and old technology. APMIS 119(10):681–688
Loonen AJ, Jansz AR, Stalpers J, Wolffs PF, van den Brule AJ (2011) An evaluation of three processing methods and the effect of reduced culture times for faster direct identification of pathogens from BacT/ALERT blood cultures by MALDI-TOF MS. Eur J Clin Microbiol Infect Dis [Epub ahead of print]
Ferroni A, Suarez S, Beretti JL, Dauphin B, Bille E, Meyer J, Bougnoux ME, Alanio A, Berche P, Nassif X (2010) Real-time identification of bacteria and Candida species in positive blood culture broths by matrix-assisted laser desorption ionization-time of flight mass spectrometry. J Clin Microbiol 48(5):1542–1548
Christner M, Rohde H, Wolters M, Sobottka I, Wegscheider K, Aepfelbacher M (2010) Rapid identification of bacteria from positive blood culture bottles by use of matrix-assisted laser desorption-ionization time of flight mass spectrometry fingerprinting. J Clin Microbiol 48(5):1584–1591
Moussaoui W, Jaulhac B, Hoffmann AM, Ludes B, Kostrzewa M, Riegel P, Prévost G (2010) Matrix-assisted laser desorption ionization time-of-flight mass spectrometry identifies 90 % of bacteria directly from blood culture vials. Clin Microbiol Infect 16(11):1631–1638
La Scola B, Raoult D (2009) Direct identification of bacteria in positive blood culture bottles by matrix-assisted laser desorption ionisation time-of-flight mass spectrometry. PLoS One 4(11):e8041
Prod’hom G, Bizzini A, Durussel C, Bille J, Greub G (2010) Matrix-assisted laser desorption ionization-time of flight mass spectrometry for direct bacterial identification from positive blood culture pellets. J Clin Microbiol 48(4):1481–1483
Ferreira L, Sánchez-Juanes F, Porras-Guerra I, García-García MI, García-Sánchez JE, González-Buitrago JM, Muñoz-Bellido JL (2011) Microorganisms direct identification from blood culture by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry. Clin Microbiol Infect 17(4):546–551
Buchan BW, Riebe KM, Ledeboer NA (2012) Comparison of the MALDI Biotyper system using Sepsityper specimen processing to routine microbiological methods for identification of bacteria from positive blood culture bottles. J Clin Microbiol 50(2):346–352
Acknowledgements
We thank Georg Häcker and Friederike von Loewenich for critically reviewing the manuscript and Susanne Stampf for the statistical advice.
Transparency declaration
All authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wüppenhorst, N., Consoir, C., Lörch, D. et al. Direct identification of bacteria from charcoal-containing blood culture bottles using matrix-assisted laser desorption/ionisation time-of-flight mass spectrometry. Eur J Clin Microbiol Infect Dis 31, 2843–2850 (2012). https://doi.org/10.1007/s10096-012-1638-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-012-1638-2