Abstract
Airway epithelial cells are the first cells to be challenged upon contact with the conidia of Aspergillus. In response, they express pattern-recognition receptors that play fundamental roles as sentinels and mediators of pulmonary innate immunity. The C-type lectin Dectin-1 is expressed predominantly on the surface of myeloid lineage cells. We examined the induction, regulation, and functions of Dectin-1 in pulmonary epithelial cells by challenging human bronchial epithelial (HBE) cells with A. fumigatus. Inflammatory, antimicrobial peptide genes and reactive oxygen species (ROS) were quantified, with and without knockdown of Dectin-1. We found that A. fumigatus induced the expression of Dectin-1 mRNA and protein in HBE cells in a toll-like receptor (TLR) 2-dependent manner. In addition, A. fumigatus-mediated generation of ROS was dependent on the upregulation of Dectin-1. Moreover, A. fumigatus actively induced the expression of TNFα, GM-CSF, IL8, HBD2, and HBD9. Knockdown of Dectin-1 inhibited TNFα, IL8, HBD2, and HBD9 expression. Hence, Dectin-1 was required for the upregulation of pro-inflammatory cytokines and antimicrobial peptides. Finally, knockdown of TLR2 significantly inhibited Dectin-1 upregulation. Our results demonstrate the novel induction of Dectin-1 in human bronchial epithelial cells and its critical role in the innate immune response against A. fumigatus in non-phagocytic cells.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Aspergillus fumigatus is a saprophytic, airborne mold that is responsible for life-threatening invasive pulmonary aspergillosis (IPA) in immunocompromised hosts [1]. As an opportunistic infection, IPA has an increasing incidence, at the same rate as the number of severely immunocompromised patients, despite the availability of new antifungal drugs [2]. Neutropenia and high-dose steroid treatments are the main risk factors for IPA, and these underline the importance of an appropriate inflammatory response if fungal invasion is to be avoided. Therefore, a better understanding of the mechanisms responsible for resistance to A. fumigatus infection is required.
The respiratory epithelium plays an important role in the innate immune defense against various inhaled pathogens by sensing signals from the external environment. Most studies stress the important roles that alveolar macrophages and neutrophils play in controlling A. fumigatus infection [3, 4]. However, the respiratory epithelium is the first tissue that inhaled conidia encounter, and it probably participates in the efficient coordinated response against IPA. In animal models of IPA, most inhaled conidia are trapped in the upper respiratory tract, and the respiratory epithelium coordinates with alveolar macrophages [5]. Some studies have observed the production of inflammatory mediators and antimicrobial peptides by studying the human lung epithelial cell line A549 after stimulation with molds or mold extracts [6–8]. Lee et al. [9, 10] reported that Mycobacterium can induce Dectin-1 through a toll-like receptor (TLR) 2-dependent manner in type II airway epithelial cells, and that the upregulation of Dectin-1 plays a critical role in the innate immune response against Mycobacterium in non-phagocytic cells.
Dectin-1 is a 28-KDa type II transmembrane protein. It was originally defined as a receptor on dendritic cells (DC), hence its name “Dendritic cell-associated C-type lectin-1,” but, later, it was found to be expressed on macrophages, monocytes, neutrophils, and some T cells [11]. In humans, Dectin-1 is also expressed in eosinophils and B cells. The functional importance of this difference in expression patterns is not presently clear. The expression pattern can differ between tissue and cell type, but, in general, Dectin-1 is expressed at high levels in the lung and intestine, as well as areas of high T cell levels, such as the spleen, thymus, and lymph nodes [12]. Yeast cell walls are, in a large part, made up of β-glucan, a ligand of Dectin-1, and the receptor is now understood to be the primary receptor on macrophages for the phagocytosis of yeast. Mice deficient in Dectin-1 are more susceptible to fungal infections, demonstrating the importance of this innate immune receptor in host defense [13]. Dectin-1 is strongly linked to phagocytosis and also strongly implicated in the induction of reactive oxygen species (ROS). Moreover, Dectin-1 seems likely to signal to modify cytokine and chemokine production, and can collaborate with TLRs in identifying and generating inflammatory responses to fungi [14].
To our knowledge, there are few reports on the response of Dectin-1 expression in bronchial epithelium to A. fumigatus. Therefore, an investigation of the potential function and mechanism of Dectin-1 receptor on bronchial epithelium after A. fumigatus challenge could help explain why it is a frequently encountered etiological agent of invasive infection. The aim of our study was to investigate whether the upregulation of Dectin-1 occurred in airway epithelial cells after exposure to A. fumigatus and whether this was beneficial during the course of infection. We also aimed to explore the potential collaboration between Dectin-1 and TLR2.
Materials and methods
A. fumigatus strain and cell line
A. fumigatus A1 was kindly provided by the Microbiological Laboratory of Jinlin Hospital (Nanjing, China). A. fumigatus strains were propagated on Sabouraud dextrose agar (10 g/L peptone, 40 g/L glucose, and 15 g/L agar) for 5 to 8 days at 37 °C. Human bronchial epithelium (HBE) cells from a papilloma virus immortalized bronchial epithelial cell line were kindly provided by Professor Xing (Laboratory of Immunology and Virology, Nanjing University, China) [15]. HBE cells were cultured in a Ham’s F12/Dulbecco’s modified Eagle’s medium (DMEM) (1:1) supplemented with insulin (5 μg/ml), transferrin (5 μg/ml), epidermal growth factor (10 ng/ml), dexamethasone (0.1 μM), cholera toxin (10 ng/ml), bovine hypothalamus extract (15 μg/ml), and bovine serum albumin (0.5 mg/ml), as described in a previous study [15].
Preparation of conidia
A. fumigatus conidia were harvested and prepared as described in a previous study [16]. Briefly, after 5 to 8 days of culture, A. fumigatus conidia were dislodged from agar plates by gentle tapping and resuspended in sterile phosphate-buffered saline supplemented with 0.025 % Tween-20 (PBST). The conidia were then passed through eight layers of sterile gauze to remove hyphal fragments and enumerated on a hemacytometer. Fungal cells were washed twice and stored at 4 °C for use within 48 h. To be sure that the inducible regulations were specific to A. fumigatus resting conidia (RC) and did not simply reflect a phagocytosis response, killed conidia (KC) were used as a control. As required, heat inactivation was performed at 121 °C for 15 min in an autoclave.
Reagents and antibodies
Laminarin and latex beads were purchased from Sigma-Aldrich (Carlsbad, CA, USA). DMEM and fetal bovine serum (FBS) were purchased from Invitrogen Gibco (Carlsbad, CA, USA). Dectin-1 siRNA (siDectin-1) and TLR2 siRNA (siTLR2) were designed as described previously [17], and synthesized by GenePharma (Shanghai, China). The Lipofectamine™ 2000 reagent was purchased from Invitrogen and polymerase chain reaction (PCR) primers were synthesized by GenScript (Nanjing, China). The sequences of all primers are listed in Table 1, which is available in the supplementary online material. The PrimeScript™ RT reagent Kit and SYBR® Premix Ex Taq™ were purchased from TaKaRa (Dalian, China). The mouse-anti-TLR2 antibody was ordered from Abcam (Cambridge, UK) and goat-anti-Dectin-1 antibody was purchased from Santa Cruz Biotechnology (Santa Cruz, CA, USA). The secondary antibody, fluorescein (FITC)-conjugated donkey anti-goat IgG, was obtained from Santa Cruz Biotechnology. The Alexa Fluor® 488-conjugated mouse anti-human Dectin-1 for fluorescence-activated cell sorting (FACS) was ordered from AbD Serotec (Kidlington, UK).
RNA interference experiments
HBE cells were transfected with siDectin-1 or siTLR2 when 50–70 % confluent in six-well plates. Nonspecific siRNA (siNS) with random nucleotides was used in each experiment as a negative control. For each transfection, 100 pmol siRNA per well was diluted in 250 μl Opti-MEM I medium (Invitrogen, Cat. No. 31985–062) without serum and gently mixed with 5 μl Lipofectamine 2000 diluted in 250 μl Opti-MEM I medium. After incubation for 15 min at room temperature, siRNA and Lipofectamine 2000 complexes were added to each well of the six-well culture plates. These plates were gently mixed by rocking back and forth. Transfected cells were incubated for 24 h before being stimulated with A. fumigatus.
Molecular studies
For PCR assays, total RNA was isolated from cultured cells using solutions in RNAprep pure Cell Kit (TIANGEN, Beijing, China). One microgram subtotal RNA was subjected to reverse transcriptase PCR (RT-PCR) and the equivalent cDNA was used for quantitative real-time PCR (Applied Biosystems, Foster City, CA, USA). The mRNA expression levels of genes were analyzed by a two-step quantitative real-time RT-PCR, as described previously [18]. Relative expression values were normalized using an internal GAPDH control.
Western blot analysis and enzyme-linked immunosorbent assay (ELISA)
HBE cells were lysed with a hypotonic buffer with 1 % NP-40 lysis buffer containing 1 mM PMSF, 1 % aprotinin, and 1 mM sodium vanadate (Sigma), as described previously [19]. Cell lysates were mixed with loading buffer and boiled for 5 min. The cell lysis was then assayed on an SDS–polyacrylamide electrophoresis gel (12 %) and transferred onto PVDF membrane (Millipore). This membrane was subsequently blocked with 5 % non-fat milk solution. Western blot analysis was performed following standard protocols using relevant antibodies, followed by incubation with relevant HRP-conjugated secondary antibodies. BeyoECL Plus reagents (Beyotime) were used for the development of colorimetric signals on the membrane. The membrane was also blotted with a monoclonal anti-actin antibody (Santa Cruz) as a loading control. The band image was acquired using G:BOX Chemi systems (Syngene).
For ELISA, cell-free supernatants were collected at the indicated times and aliquots were stored at −70 °C until use. The concentration of TNFα in medium was determined using an ELISA kit (R&D Systems, Minneapolis, MN, USA), according to the manufacturer’s instructions.
Flow cytometry and immunofluorescence confocal microscopy analysis
HBE cells were analyzed by FACS for the expression of Dectin-1 using a flow cytometer (FACSAria III, Becton Dickinson). The cells were collected at the indicated times and stained with a primary antibody against Dectin-1, conjugated to Alexa Fluor 488, for 30 min at room temperature, using 10 μl antibody at the suggested working dilution to label 1 × 106 cells in 100 μl. In each case, 10,000 cells were acquired. The data were analyzed using WinMDI (version 2.9).
HBE cells were cultured in six-well culture plates and cytospun onto glass slides. After stimulation, cells were fixed and incubated with anti-Dectin-1 antibody at 4 °C overnight. Then, cells were washed with PBS and incubated with FITC-conjugated secondary antibody at room temperature for 1 h. Cells were analyzed by an Olympus FV10i laser scanning confocal microscope for acquiring and processing the confocal images.
Measurement of intracellular ROS
HBE cells were initially plated and cytospun onto glass slides at a density of 5 × 105 cells/well in six-well plates for 24 h. To monitor the intracellular accumulation of ROS, the cells were pretreated with MDCF-DA (10 μm/L), a substrate which detects ROS production, for 20 min at 37 °C and then incubated with RC and KC (MOI = 1) for 1 h. After stimulation, the treated cells were subjected to confocal microscopy using 485-nm excitation and 535-nm emission filters [20]. DCF fluorescence images were imported into NIH ImageJ software, and fluorescence intensities were analyzed under fixed thresholds across all slides [21]. Thresholds were chosen within the range that allowed outlining as many immunopositive areas as possible throughout all images. The intensities of images were detected using the ‘analyze particle’ module of the program. The results were given as percentages relative to the oxidative stress of the control cells set to 1. All of the data shown are means ± standard deviation (SD).
Statistical analysis
The data expressed in the figures were either from a representative experiment or from the mean ± SD of three independent experiments. Except where otherwise indicated, Student’s paired t-test was used to compare the difference between groups, and values of p < 0.05 were considered to be statistically significant.
Results
Upregulation of Dectin-1 expression in HBE cells
Dectin-1 can be induced in epithelial cells and plays a critical role in the innate immune response to microorganisms such as M. ulcerans and M. tuberculosis by the recognition of β-glucan [9, 10]. As the cell walls of A. fumigatus are rich in β-glucan, just like Mycobacterium sp., we sought to determine whether A. fumigatus could induce Dectin-1 expression in human bronchial epithelial cells. To explore the expression of Dectin-1 and identify its potential role in airway epithelium during A. fumigatus infection, we challenged HBE cells with RC. In cells stimulated with KC, latex beads, and laminarin, the expression of Dectin-1 mRNA remained at a low level. When challenged by RC, the cells significantly increased the expression of Dectin-1 mRNA at 6 and 18 h (Fig. 1a). The results also showed that neither laminarin nor latex beads induced Dectin-1 expression in HBE cells. Interestingly, the pretreatment of HBE cells with laminarin resulted in an inhibition of RC-induced Dectin-1 upregulation (Fig. 1a). Furthermore, FACS analysis and confocal immunofluorescence microscopy identified that the distribution of Dectin-1 receptor on the cell membrane increased in a time-dependent manner (Fig. 1b, c, d). According to confocal analysis, the expression of Dectin-1 peaked about 24 h after stimulation.
The expression of Dectin-1 in human bronchial epithelial (HBE) cells can be induced by Aspergillus fumigatus. a HBE cells were stimulated with resting conidia (RC), killed conidia (KC) (MOI = 1), latex beads, or laminarin (250 μg/ml), as indicated. Total mRNA was isolated at the indicated times for real-time polymerase chain reaction (PCR). The mRNA level of Dectin-1 was measured by quantitative real-time PCR. b After being challenged with RC and KC (MOI = 1), and labeled with specific human Dectin-1 antibody and fluorescein (FITC)-conjugated secondary antibody in the indicated times, the HBE cells were observed through a confocal immunofluorescence microscope. c HBE cells were collected 6 h after stimulation with RC and KC (MOI = 1) and subjected to fluorescence-activated cell sorting (FACS) analysis. In total, 10,000 cells were analyzed per sample. d The mean fluorescence intensities are shown as the mean ± standard deviation (SD) of three independent experiments. # p < 0.01. Scale bar = 20 μm
Expression of inflammatory cytokines and innate antimicrobial peptides
The exposure of epithelial cells to A. fumigatus can increase the mRNA levels of some inflammatory mediators and antimicrobial peptides [5, 8, 22–24]. We aimed to investigate the role of epithelial chemokines, cytokines, and antimicrobial peptides in initiating the protective response to A. fumigatus. After exposing HBE cells to RC, HBE cells were subjected to real-time PCR for the quantification of genes expression. HBE cells significantly increased the expression of TNFα, GM-CSF, IL8, HBD2, and HBD9 after being stimulated for 6 and 18 h, and the expression of IL6, HBD1, and LL37 had unchanged levels (Fig. 2a, b).
Standardized HBE cell mRNA expression of the genes encoding inflammatory cytokines and innate antimicrobial peptides after exposure to RC and KC. Total mRNA was isolated at the indicated times for real-time PCR. The levels of mRNA for different genes were measured by quantitative real-time PCR. a Induction of inflammatory cytokines was measured by quantitative real-time PCR in HBE cells after being stimulated for 6 and 18 h, as indicated. b Induction of antimicrobial peptides was measured by quantitative real-time PCR in HBE cells after being stimulated for 6 and 18 h, as indicated. Gene expression was subsequently normalized against the median values of the uninfected controls. # p < 0.01
Dectin-1 and protective responses
Since Dectin-1 was required for pro-inflammatory cytokine release and antimicrobial effects of bronchial epithelia against some Mycobacterium [9, 10], we next investigated the role of the upregulation of Dectin-1 in the protective response of HBE cells to A. fumigatus. We performed knockdown experiments using siRNA for Dectin-1. As shown in Fig. 3, the transfection of siDectin-1 significantly reduced the A. fumigatus-mediated upregulation of Dectin-1 in HBE cells, whereas the transfection of control siRNA did not.
Inhibition of Dectin-1 mRNA and protein expression by siRNA. HBE cells were pretransfected with nonspecific siRNA (siNS) or Dectin-1-specific siRNA (siDectin-1). After 12 h, HBE cells were challenged with RC conidia (MOI = 1). a The level of mRNA for Dectin-1 was measured in total RNA preparations by quantitative real-time PCR for the indicated times. b HBE cells were harvested at 18 h and subjected to Western blot analysis using Dectin-1 antibody. c After transfection, HBE cells were challenged with RC and then subjected to FACS analysis 6 h after incubation. In total, 10,000 cells were analyzed per sample. d The mean fluorescence intensities are shown as the mean ± SD of three independent experiments. # p < 0.01
Then, we examined whether Dectin-1 was required for the unregulated expression of some inflammatory cytokines and antimicrobial peptides in HBE cells. Dectin-1 silencing resulted in a moderate but significant downregulation of TNFα and IL8 mRNA at 6 and 18 h of RC infection (p < 0.05), but not of GM-CSF (Fig. 4a). Innate antimicrobial peptides, HBD2 and HBD9, also showed significant downregulation (Fig. 4b). The expression of GM-CSF was not influenced by Dectin-1 silencing, suggesting that there may be some other signaling pathway involved in GM-CSF expression. We also measured the concentration of TNFα in culture supernatants from HBE cells by ELISA (Fig. 4c). After Dectin-1 silencing, the level of TNFα was significantly attenuated at 6 and 18 h post-infection, according to ELISA detection.
Regulation of inflammatory cytokines and antimicrobial peptides mRNA in HBE cells after Dectin-1 knockdown. Total mRNA was isolated at the indicated times for reverse transcription PCR. The levels of mRNA for different genes were measured by quantitative real-time PCR. a The induction of inflammatory cytokines was measured in HBE cells following transfection with siDectin-1 or siNS after stimulation with RC for 6 and 18 h, as indicated. b Induction of antimicrobial peptides was also measured in HBE cells following transfection with siDectin-1 or siNS. Gene expression was subsequently normalized against the median values of the uninfected controls. c Culture supernatants from HBE cells were harvested at different time points and the level of TNFα was measured by enzyme-linked immunosorbent assay (ELISA). The data are the mean ± SD of three experiments. *p < 0.05, # p < 0.01
ROS generation
Dectin-1 is reported to play a role in ROS production in murine macrophages [25], and human epithelium can generate Dectin-1-dependent ROS when challenged by some Mycobacterium [9, 10]. Therefore, we next determined whether Dectin-1 expression was also required for A. fumigatus-induced ROS generation in airway epithelial cells. HBE cells were transfected with siNS or siDectin-1 and, 24 h after transfection, these cells were treated with RC and KC. The knockdown of Dectin-1 (Fig. 5) markedly inhibited conidia-induced ROS production in HBE cells. ROS generation decreased considerably in cells transfected with siDectin-1, whereas cells transfected with siNS showed higher ROS generation when stimulated with RC. The fluorescence intensity of cells was measured using NIH ImageJ software (Fig. 5b).
Reactive oxygen species (ROS) induction is dependent on the expression of Dectin-1 in HBE cells. a HBE cells pretreated with DCHF-DA (10 μm/L) for 20 min were stimulated with KC and RF (MOI = 1) for 6 h and then subjected to confocal fluorescence microscopy. b The fluorescence intensities, indicating ROS levels, were measured by using the ‘analyze particle’ module of NIH ImageJ software and presented as the amount of ROS production. The data represent the mean ± SD for three independent replicates. Scale bar = 20 μm
Dectin-1 expression in a TLR2-dependent manner
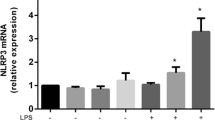
M. tuberculosis actively induces the expression of Dectin-1 mRNA and protein in A549 cells in a TLR2-dependent manner [9]. Therefore, we investigated whether the inducible Dectin-1 expression was mediated by TLR2 receptor. HBE cells were transfected with hTLR2-specific siRNA (siTLR2) and siNS (Fig. 6a) and were then stimulated with RC and KC. We found that the upregulation of Dectin-1 was reduced significantly (p < 0.05) in HBE cells with TLR2 silencing compared to those transfected with siNS (Fig. 6b, c).
The induction of Dectin-1 expression was in a toll-like receptor (TLR) 2-dependent manner. a After the transfection of hTLR2-specific siRNA (siTLR2), HBE cells were incubated with RC and KC for 18 h, harvested, and subjected to Western blot analysis using TLR2 antibody. b, c HBE cells were transfected with siNS, or siTLR2, and then subjected to FACS analysis to identify Dectin-1 expression 6 h after incubation with RC and KC. In total, 10,000 cells were analyzed per sample. For b, the mean fluorescence intensities of FACS are shown as the mean ± SD of three independent experiments. *p < 0.05
Discussion
The inhalation of conidia is the main cause of IPA, and as an important part of the innate immune system, the respiratory epithelium is the first line of defense. Many studies suggest that the airway epithelia are not simply ‘innocent bystanders,’ but may play a crucial role in innate and inflammatory responses [26].
Dectin-1, a C-type lectin-like receptor, appears to play a central role in defense against A. fumigatus [14, 27]. Dectin-1 is a non-TLR receptor that mediates the recognition of glucan [28] and the production of inflammatory mediators in response to live fungal pathogens [29]. It is expressed on the surface of dendritic cells, monocytes/macrophages, neutrophils, and at low levels on a subpopulation of T cells [30, 31]. Human epithelial cells can upregulate Dectin-1 levels when challenged by certain microorganisms [9, 10]. M. tuberculosis actively induces Dectin-1 expression in A549 cells, and this is modulated by blocking TLR2 [9]. We found that treating bronchial epithelial cells with A. fumigatus significantly induced Dectin-1 mRNA and protein expression. In our study, the heat-inactivated resting conidia were used for stimulation, and no induction of Dectin-1 had been observed. However, a similar experiment found that heat-inactivated conidia could induce Dectin-1 expression in airway epithelium [32]. The different data between two studies could be caused by using conidia with different stages. The similar study generated and used inactivated swollen conidia for stimulation. Resting conidia were surrounded by a hydrophobic layer comprised of rodlet proteins. The rodlet layer could protect conidia from recognition and phagocytosis by the host defense system [33]. Conidial swelling released the protective rodlet layer and exposed glucan and some other antigens. Then, innate immune function would be activated, such as upregulation pattern recognition receptors, proinflammatory responses, and phagocytosis [34, 35].
Some studies have highlighted the importance of collaboration between toll-like receptors and Dectin-1 in regulating inflammatory responses [14]. Dectin-1, in collaboration with TLRs and the nucleotide oligomerization domain proteins, plays a central role in the detection of and response to invading pathogens. We found that A. fumigatus-induced Dectin-1 expression is regulated in a TLR2-dependent manner. The modulation of Dectin-1 expression by TLR2 suggests a close interaction between these proteins.
We found that Dectin-1 was required for the upregulation of inflammatory cytokines and innate antimicrobial peptides. An important element of antimicrobial defenses is the production of inflammatory cytokines, the induction of which is critically dependent on the TLRs [36]. However, in addition to the TLRs, this inflammatory response has also been shown to require Dectin-1 [29]. The inducible expression of defensins by human bronchial epithelial cells exposed to A. fumigatus was investigated and several types of defensins can be induced [8]. When challenged with A. fumigatus, HBE cells activated the expression of some inflammatory cytokines and innate antimicrobial peptides, such as TNFα, GM-CSF, IL8, HBD2, and HBD9. The knockdown of Dectin-1 resulted in a significant decrease in A. fumigatus-induced TNFα, IL8, HBD2, and HBD9.
Commonly, Dectin-1 is strongly linked to functions of phagocytosis or the production of ROS [14, 37]. We showed that the upregulation of Dectin-1 played a crucial role in the induction of ROS. When Dectin-1 was silenced, HBE cells significantly decreased their A. fumigatus-induced ROS production. ROS can be released by recruited neutrophils as a response to conidia challenge and mediate extracellular killing [28, 38]. The importance of ROS killing mechanisms is demonstrated by patients with chronic granulomatous disease (CGD), who carry genetic lesions in essential components of an ROS-generating NADPH oxidase complex, and commonly present with life-threatening IPA [28, 39]. We confirmed that HBE cells generated A. fumigatus-induced ROS in a Dectin-1-dependent manner.
Our data also confirmed that A. fumigatus-induced Dectin-1 expression was regulated in a TLR2-dependent manner. A recent study found that M. tuberculosis can actively induce the expression of Dectin-1 mRNA and protein in A549 cells in a TLR2-dependent manner [26]. It also confirmed that phosphorylation of Src family kinases is a crucial regulator of Dectin-1-dependent signaling. Therefore, we investigated whether the induction of Dectin-1 expression was dependent on the TLR2 receptor using TLR2 silencing and found that knockdown of TLR2 significantly reduced the expression of Dectin-1 following A. fumigatus stimulation. As the bronchial epithelium did not express Dectin-1 receptor on the cell membrane, the activation of Dectin-1 upregulation may be initiated by the recognition of A. fumigatus by TLR2.
Our results emphasize a role for Dectin-1 in the A. fumigatus infection of bronchial airway epithelial cells. Innate immune responses to microbial challenge include the production of immunomodulatory cytokines and chemokines, phagocytosis, and killing by the production of anti-microbial peptides and reactive oxygen and nitrogen species. Dectin-1 is strongly linked to phagocytosis or the production of ROS, and likely implicated in regulating cytokine and chemokine production [14]. Previous studies have shown that Dectin-1 collaborates with TLR2 to induce TNFα and IL-6 [31]. In addition, Dectin-1 is involved in conjunction with TLR2 in M. abscessus-induced innate immune responses, including phagocytosis and inflammatory cytokine production by macrophages [40]. Phagocytosis and antimicrobial activation are two crucial elements of the innate immune system response to microorganism infection. The present data clearly demonstrated that Dectin-1 contributes to the A. fumigatus-induced chemokine synthesis in HBE cells. We also found that the upregulation of Dectin-1 was essential for ROS production, thus, indicating that inducible Dectin-1 expression was functional in bronchial airway epithelial cells.
In summary, this study presents a novel insight into Dectin-1 induction via TLR2 in airway epithelial cells, resulting in the induction of proinflammatory responses and ROS generation in response to A. fumigatus. The robust activation of ROS release in response to A. fumigatus required the upregulation of Dectin-1. In addition, our siRNA silencing data indicated that the upregulation of Dectin-1 played a crucial role in the expression of TNFα, GM-CSF, IL8, HBD2, and HBD9. Our results confirmed the biological role that bronchial epithelia play in the innate defense against A. fumigatus infection and the importance of Dectin-1 in this process. Elucidation of the molecular mechanisms which drive the innate immune response in airway epithelial cells will provide new insights into the development of therapies for A. fumigatus.
References
Denning DW, Anderson MJ, Turner G, Latgé JP, Bennett JW (2002) Sequencing the Aspergillus fumigatus genome. Lancet Infect Dis 2:251–253
Kleinberg M (2005) Aspergillosis in the CLEAR outcomes trial: working toward a real-world clinical perspective. Med Mycol 43(Suppl 1):S289–S294
Romani L (2011) Immunity to fungal infections. Nat Rev Immunol 11:275–288
Walsh TJ, Roilides E, Cortez K, Kottilil S, Bailey J, Lyman CA (2005) Control, immunoregulation, and expression of innate pulmonary host defenses against Aspergillus fumigatus. Med Mycol 43(Suppl 1):S165–S172
Bellanger AP, Millon L, Khoufache K, Rivollet D, Bièche I, Laurendeau I et al (2009) Aspergillus fumigatus germ tube growth and not conidia ingestion induces expression of inflammatory mediator genes in the human lung epithelial cell line A549. J Med Microbiol 58:174–179
Zhang Z, Liu R, Noordhoek JA, Kauffman HF (2005) Interaction of airway epithelial cells (A549) with spores and mycelium of Aspergillus fumigatus. J Infect 51:375–382
Tai HY, Tam MF, Chou H, Peng HJ, Su SN, Perng DW et al (2006) Pen ch 13 allergen induces secretion of mediators and degradation of occludin protein of human lung epithelial cells. Allergy 61:382–388
Alekseeva L, Huet D, Féménia F, Mouyna I, Abdelouahab M, Cagna A et al (2009) Inducible expression of beta defensins by human respiratory epithelial cells exposed to Aspergillus fumigatus organisms. BMC Microbiol 9:33
Lee HM, Yuk JM, Shin DM, Jo EK (2009) Dectin-1 is inducible and plays an essential role for mycobacteria-induced innate immune responses in airway epithelial cells. J Clin Immunol 29:795–805
Lee HM, Shin DM, Choi DK, Lee ZW, Kim KH, Yuk JM et al (2009) Innate immune responses to Mycobacterium ulcerans via toll-like receptors and dectin-1 in human keratinocytes. Cell Microbiol 11:678–692
Schorey JS, Lawrence C (2008) The pattern recognition receptor Dectin-1: from fungi to mycobacteria. Curr Drug Targets 9:123–129
Reid DM, Montoya M, Taylor PR, Borrow P, Gordon S, Brown GD et al (2004) Expression of the beta-glucan receptor, Dectin-1, on murine leukocytes in situ correlates with its function in pathogen recognition and reveals potential roles in leukocyte interactions. J Leukoc Biol 76:86–94
Taylor PR, Tsoni SV, Willment JA, Dennehy KM, Rosas M, Findon H et al (2007) Dectin-1 is required for beta-glucan recognition and control of fungal infection. Nat Immunol 8:31–38
Underhill DM (2007) Collaboration between the innate immune receptors dectin-1, TLRs, and Nods. Immunol Rev 219:75–87
Xing Z, Harper R, Anunciacion J, Yang Z, Gao W, Qu B et al (2011) Host immune and apoptotic responses to avian influenza virus H9N2 in human tracheobronchial epithelial cells. Am J Respir Cell Mol Biol 44:24–33
Hohl TM, Van Epps HL, Rivera A, Morgan LA, Chen PL, Feldmesser M et al (2005) Aspergillus fumigatus triggers inflammatory responses by stage-specific beta-glucan display. PLoS Pathog 1:e30
Mezger M, Kneitz S, Wozniok I, Kurzai O, Einsele H, Loeffler J (2008) Proinflammatory response of immature human dendritic cells is mediated by dectin-1 after exposure to Aspergillus fumigatus germ tubes. J Infect Dis 197:924–931
Xing Z, Conway EM, Kang C, Winoto A (2004) Essential role of survivin, an inhibitor of apoptosis protein, in T cell development, maturation, and homeostasis. J Exp Med 199:69–80
Xing Z, Cardona CJ, Adams S, Yang Z, Li J, Perez D et al (2009) Differential regulation of antiviral and proinflammatory cytokines and suppression of Fas-mediated apoptosis by NS1 of H9N2 avian influenza virus in chicken macrophages. J Gen Virol 90:1109–1118
Ye J, Li J, Yu Y, Wei Q, Deng W, Yu L (2010) L-carnitine attenuates oxidant injury in HK-2 cells via ROS-mitochondria pathway. Regul Pept 161:58–66
Blundell J, Blaiss CA, Etherton MR, Espinosa F, Tabuchi K, Walz C et al (2010) Neuroligin-1 deletion results in impaired spatial memory and increased repetitive behavior. J Neurosci 30:2115–2129
Balloy V, Sallenave JM, Wu Y, Touqui L, Latgé JP, Si-Tahar M et al (2008) Aspergillus fumigatus-induced interleukin-8 synthesis by respiratory epithelial cells is controlled by the phosphatidylinositol 3-kinase, p38 MAPK, and ERK1/2 pathways and not by the toll-like receptor-MyD88 pathway. J Biol Chem 283:30513–30521
Huttunen K, Hyvärinen A, Nevalainen A, Komulainen H, Hirvonen MR (2003) Production of proinflammatory mediators by indoor air bacteria and fungal spores in mouse and human cell lines. Environ Health Perspect 111:85–92
Borger P, Koëter GH, Timmerman JA, Vellenga E, Tomee JF, Kauffman HF (1999) Proteases from Aspergillus fumigatus induce interleukin (IL)-6 and IL-8 production in airway epithelial cell lines by transcriptional mechanisms. J Infect Dis 180:1267–1274
Gantner BN, Simmons RM, Underhill DM (2005) Dectin-1 mediates macrophage recognition of Candida albicans yeast but not filaments. EMBO J 24:1277–1286
Gribar SC, Richardson WM, Sodhi CP, Hackam DJ (2008) No longer an innocent bystander: epithelial toll-like receptor signaling in the development of mucosal inflammation. Mol Med 14:645–659
Herre J, Willment JA, Gordon S, Brown GD (2004) The role of Dectin-1 in antifungal immunity. Crit Rev Immunol 24:193–203
Brown GD, Gordon S (2001) Immune recognition. A new receptor for beta-glucans. Nature 413:36–37
Brown GD, Herre J, Williams DL, Willment JA, Marshall AS, Gordon S (2003) Dectin-1 mediates the biological effects of beta-glucans. J Exp Med 197:1119–1124
Ariizumi K, Shen GL, Shikano S, Xu S, Ritter R 3rd, Kumamoto T et al (2000) Identification of a novel, dendritic cell-associated molecule, dectin-1, by subtractive cDNA cloning. J Biol Chem 275:20157–20167
Taylor PR, Brown GD, Reid DM, Willment JA, Martinez-Pomares L, Gordon S et al (2002) The beta-glucan receptor, dectin-1, is predominantly expressed on the surface of cells of the monocyte/macrophage and neutrophil lineages. J Immunol 169:3876–3882
Cunha C, Di Ianni M, Bozza S, Giovannini G, Zagarella S, Zelante T et al (2010) Dectin-1 Y238X polymorphism associates with susceptibility to invasive aspergillosis in hematopoietic transplantation through impairment of both recipient- and donor-dependent mechanisms of antifungal immunity. Blood 116:5394–5402
Dagenais TR, Keller NP (2009) Pathogenesis of Aspergillus fumigatus in invasive Aspergillosis. Clin Microbiol Rev 22:447–465
Dagenais TR, Giles SS, Aimanianda V, Latgé JP, Hull CM, Keller NP (2010) Aspergillus fumigatus LaeA-mediated phagocytosis is associated with a decreased hydrophobin layer. Infect Immun 78:823–829
Paris S, Debeaupuis JP, Crameri R, Carey M, Charlès F, Prévost MC et al (2003) Conidial hydrophobins of Aspergillus fumigatus. Appl Environ Microbiol 69:1581–1588
Akira S, Takeda K (2004) Toll-like receptor signalling. Nat Rev Immunol 4:499–511
Han X, Yu R, Zhen D, Tao S, Schmidt M, Han L (2011) Beta-1,3-Glucan-induced host phospholipase D activation is involved in Aspergillus fumigatus internalization into type II human pneumocyte A549 cells. PLoS One 6:e21468
Nathan C (2006) Neutrophils and immunity: challenges and opportunities. Nat Rev Immunol 6:173–182
Segal BH, Romani LR (2009) Invasive aspergillosis in chronic granulomatous disease. Med Mycol 47(Suppl 1):S282–S290
Shin DM, Yang CS, Yuk JM, Lee JY, Kim KH, Shin SJ et al (2008) Mycobacterium abscessus activates the macrophage innate immune response via a physical and functional interaction between TLR2 and dectin-1. Cell Microbiol 10:1608–1621
Acknowledgments
This study was granted by the Hospital Foundation of Jinling Hospital (2011026). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Table 1
Sequences of primers for the real-time polymerase chain reaction (PCR) (DOCX 12 kb)
Rights and permissions
About this article
Cite this article
Sun, WK., Lu, X., Li, X. et al. Dectin-1 is inducible and plays a crucial role in Aspergillus-induced innate immune responses in human bronchial epithelial cells. Eur J Clin Microbiol Infect Dis 31, 2755–2764 (2012). https://doi.org/10.1007/s10096-012-1624-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-012-1624-8