Abstract
We study the clinical, management and outcome differences between respiratory syncytial virus (RSV) positive and negative bronchiolitis. A retrospective review of the medical records of children ≤ 2 years of age with acute bronchiolitis between January 1995 and December 2006 was done. There were 2,384 patients hospitalized for acute bronchiolitis, and 1,495 (62.7%) were RSV infections. Overall, hospitalization rate was 55/1,000 admissions. Mortality occurred in 0.08% of cases. Bronchiolitis due to RSV was more frequent from November to March (97%). RSV bronchiolitis had longer hospital stays (6 vs. 5 days, P<0.0001), higher risk of intensive care unit (ICU) admission (OR 2.7; 95%CI 1.87–3.9) and more oxygen use (OR 2.2; 95%CI 1.8–2.6). Infants < 2 months had longer median hospital stay (6 vs. 5 days, P <0.0001) and higher risk of ICU admission (OR 3.4; 95%CI 2.5–4.6). Prematures of < 32 gestational weeks, congenital heart disease, and atelectasis/condensation were the main risk factors for ICU admission in both RSV and non-RSV bronchiolitis. The introduction of palivizumab in prematures diminished hospitalization for RSV bronchiolitis, oxygen need, length of hospital stay and mechanical ventilation. In conclusion, this study supports that RSV bronchiolitis seems to be a more severe disease than that caused by other viruses.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute bronchiolitis is the main cause of hospitalization in young infants. Although this infection can occur year round it is more frequent in epidemic peaks during the winter months [1, 2]. At the moment, there is no pharmacological intervention that has been proven to have an impact on the course of the disease. During the last decade a better knowledge of the etiology of this entity has been achieved, but it has not resulted in significant therapeutic advances. Respiratory syncytial virus (RSV) usually causes 50–80% of cases of acute bronchiolitis, but other viruses causing bronchiolitis have been reported [3]. These findings have raised the question of the clinical relevance of the etiologic agent, especially if the course of the disease caused by RSV is similar to that of other viruses, and also the significance of the simultaneous presence of more than one virus [4].
In this study, we have determined the epidemiology and outcomes of the infants hospitalized for bronchiolitis in an insular area of Spain. The epidemiological, clinical, and diagnostic approaches as well as management differences between RSV positive and RSV negative bronchiolitis were especially evaluated.
Patients and methods
Study population
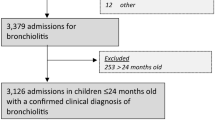
From January 1, 1995 to December 31, 2006, the medical records of infants and young children admitted to the Department of Pediatrics of Son Dureta University Hospital with a diagnosis of acute bronchiolitis were retrospectively reviewed. Situated in the southeastern part of the island of Mallorca (Spain), this hospital is the only tertiary care center in the Balearic Islands.
Subjects were selected after revision of the hospital discharge codes with a primary or secondary diagnosis of bronchiolitis. Episodes of acute bronchiolitis were identified via the International Classification of Diseases, 9th revision, with the following discharge codes: acute bronchiolitis (466.1), RSV bronchiolitis (466.11), RSV pneumonia (480.1) and RSV not otherwise specified (079.6). After reviewing the medical records only those with a first episode of obstructive lower respiratory tract infection during the first two years of life were selected. All children with a previous episode of lower respiratory tract infection were excluded. Information on the total number of premature infants born during the study period was obtained from the neonatal unit registry.
Data collection
In this study, we collected the following data: (a) demographic and epidemiologic (age, gender, date of admission, season, palivizumab administration); (b) underlying conditions (history of prematurity < 32 weeks of gestation or extreme prematurity, and 32–36 weeks of gestation or non-extreme prematurity, congenital heart disease); (c) comorbidities (acute otitis media, condensation and/or atelectasis, urinary tract infection); (d) diagnostic tests (RSV detection or not, thorax X-rays, thoracic CT scans, echocardiography, complete blood count and chemistry, blood culture, immunoglobulines, sweat test, esophagogastric scintiscan, fibrobronchoscopy); (e) treatments (salbutamol, epinephrine, ipratropium bromide, budesonide, ribavirin use, systemic steroids, antibiotic use, enteral feeding, nitric oxide, invasive and non-invasive mechanical ventilation); (f) outcomes of care or disease-severity parameters (intensive care unit [ICU] admission, oxygen supply, length of stay and mortality).
All bronchiolitis in which RSV was not detected were classified as non-RSV bronchiolitis. The rate of hospitalization for bronchiolitis was calculated as the number of admissions per 1,000 hospital admissions. Mortality rate for bronchiolitis was defined as the number of deaths per 1,000 admissions for bronchiolitis. Data on the use of oral and/or intravenous antibiotic was collected as a unique variable. Only blood tests including white blood cell (WBC) count, percentage of neutrophils and C-reactive protein (CRP) performed during the first 72 hours of admission were considered.
Virological detection
In our hospital protocols all children admitted for acute bronchiolitis are tested for RSV. RSV detection was done on nasopharyngeal aspirate or wash specimen by an enzyme-linked immunoassay (Becton Dickinson, Lincoln Park, NJ) and/or virus culture using HEp-2 cell lines.
Statistics
Results are presented as mean ± standard deviation and range or percentage as required. Continuous variables were analyzed using the Student’s t-test and categorical variables by the χ2 test or Fischer’s exact test. A non-parametric test (Mann-Whitney U test) was used for variables that were not normally distributed. The independent association between risk factors for severe disease and outcome (measured by length of hospital stay, oxygen need and ICU admission) were analyzed using a backward multivariate linear and logistic regression. To evaluate the impact of analytical tests on ICU admission and oxygen need, one way ANOVA test was performed. To analyze trends, the introduction of palivizumab in the year 2001 was used as cut point. A P value < 0.05 was considered statistically significant. All the analyses were performed with SPSS version 15.0 software.
Results
General characteristics
From January 1st 1995 to December 31st 2006, a total of 2,889 patients were admitted with a diagnosis of bronchiolitis. Excluded from analyses were: 19 patients with no information about RSV microbiology, eight patients erroneously codified, 77 patients with more than 2 years of age, and 401 patients with a previous episode of obstructive lower airway infection. A total of 2,384 patients were selected for study. Most of the admissions occurred in the months of January (652, 27.3%), February (443, 18.6%) and December (496, 20.8%). The hospitalization rate was 55 cases per 1,000 hospital admissions, accounting for 5.5% of the children hospitalized during the study period. A total of 1,391/2,384 (58%) were male sex. The mean age was 3.9 months (range, 0–23 months), with 5 median days of hospital stay (range 1–55). Among the infants hospitalized for bronchiolitis, 1,836/2,384 (77%) were under 6 months of age. A total of 246 (10.3%) patients had a previous history of prematurity; 174 (7.3%) were born between 32 and 36 weeks of gestational age (GA) and 72 (3%) were born at or before 32 weeks GA. Mortality rate was 0.8 cases per 1,000 admissions for bronchiolitis (2/2,384; 0.08%), and all of them were RSV positive.
Comorbidities
During the hospital stay 351 children (14.7%) were diagnosed with acute otitis media. The mean age for children with acute otitis media was higher than the mean age of the population studied (5.3 vs. 3.9 months; P <0.0001). A concomitant urinary tract infection was detected in 14 patients (0.6%). Among the 2,097 children who had a chest X-ray, 353 (16.8%) showed atelectases and/or condensations. During hospitalization other non-related morbidities were diagnosed: 1 cystic fibrosis, 2 congenital diaphragmatic hernia, 1 leukemia, 1 aortic coarctation, 1 hypogammaglobulinemia, and 1 ventricular septal defect.
Diagnostic tests and treatment
Table 1 shows the main diagnostic tests and treatments performed on patients hospitalized for bronchiolitis. RSV rapid antigen test and/or virus culture was done in all cases, and a blood test (complete blood count and chemistry) was performed in 653 patients. The results of CRP, WBC count and neutrophil percentage are shown in Table 2. Regardless of the etiology of bronchiolitis, CRP values were associated with increased length of stay (Z = 16.01 and 10.4, with P <0.001, for RSV and non-RSV, respectively). In addition, total WBC count was associated with ICU admission (F = 31.2 and 6.01, with P <0.0001 and P <0.05, for RSV and non-RSV, respectively) and length of hospital stay (Z = 24.34 and 19.2, with P <0.0001, for RSV and non-RSV, respectively). The percentage of neutrophils was not associated with ICU admission, oxygen need or length of hospital stay.
Differences between RSV and non-RSV bronchiolitis
Among children hospitalized for acute bronchiolitis, RSV was detected in 1,495 (62.7%) cases. Admissions for RSV bronchiolitis usually occurred from November to March (97%). Non-RSV bronchiolitis admissions occurred year round with peaks between the months of January and March. Figure 1 shows the monthly distribution of cases. Hospitalization rates for RSV bronchiolitis and non-RSV bronchiolitis were 34.5 and 20.5 admissions per 1,000 hospitalizations, respectively. Table 1 shows the main differences between RSV bronchiolitis and non-RSV bronchiolitis. RSV bronchiolitis had a longer median hospital stay (6 vs. 5 days, P <0.0001), higher risk of admission to ICU (OR 2.7; 95% CI 1.87–3.9), and more oxygen use (OR 2.2; 95% CI 1.8–2.6). Children with RSV bronchiolitis were also at a higher risk of presenting acute otitis media (OR 1.28; 95% CI 1–1.6) and atelectases/condensations (OR 1.38; 95% CI 1.08–1.77) compared to non-RSV bronchiolitis. As shown in Table 2, WBC count was higher in non-RSV compared to RSV bronchiolitis, and no significant differences were observed for the percentage of neutrophils or CRP.
Effect of risk factors on outcomes
The results of the risk factors in the multivariate analysis are summarized in Tables 3 and 4. Increase in the median hospital stay was more important in patients less than 1 month (8 vs. 3 days; P < 0.0001) and less than 2 months (6 vs. 5 days; P < 0.0001) of age. In the same way children aged less than 1 month (OR 4.4; 95% CI 2.7–7.2) and less than 2 months (OR 3.4; 95% CI 2.5–4.6) were at higher risk of ICU admission. Though outcome variables suggested a worse prognosis of RSV bronchiolitis in infants with a history of ≤ 32 gestational weeks compared to non-RSV bronchiolitis (see Table 5), statistical significance was not achieved.
Children with a history of prematurity had a longer median hospital stay compared to non-premature infants. It was significantly longer both in non-extreme prematures (6 vs. 5 days; P <0.001) and extreme prematures (6 vs. 5 days; P <0.001). Infants with a history of heart disease also had a longer hospital stay (6 vs. 5 days; P <0.0001).
Impact of Palivizumab in RSV and non-RSV bronchiolitis
A total of 774 children were born with ≤ 32 gestational weeks during the study period; 72/774 (9.3%) children were hospitalized for bronchiolitis. Children born with ≤ 32 weeks GA and hospitalized for acute bronchiolitis accounted for 3% (72/2384) of all the children admitted for acute bronchiolitis during the study period. Differences between pre-palivizumab and post-palivizumab introduction in RSV and non-RSV bronchiolitis are shown in Table 5. The median number of doses administered in hospitalized patients for bronchiolitis was 2 (IQR 1–3). In patients hospitalized for RSV bronchiolitis, four had not received RSV prophylaxis with palivizumab, two were to receive it in the following days, and two had received a single dose in the previous 48 hours.
Trends
During the periods 1995–2000 and 2001–2006 there were 1,292 and 1,092 cases of bronchiolitis, respectively. Hospitalization rates for bronchiolitis decreased from 58.8 to 51 admissions per 1,000 hospitalizations (P <0.001). There was a decrease in the median age of children hospitalized for bronchiolitis (4.3 months vs. 3.4 months, P < 0.0001) and in the median hospital stay (5 days vs. 4 days, P < 0.05). We also observed a significant (P < 0.001) increase in the proportion of RSV bronchiolitis in the period 2001–2006 (59% vs. 66.6%; P < 0.001). Regarding the use of diagnostic tools, no differences were found except for an increase in sweat tests during the last study period (51 vs. 93 tests, P < 0.0001).
Discussion
In general there is scarce information about the epidemiology of children hospitalized for bronchiolitis. In the United States an increase in the rates of hospitalization for this disease were reported during the 1990s [1, 2]. Nevertheless, our hospital admission rates for bronchiolitis slightly decreased from 2001 to 2006. During this time the mean age of the children admitted for this cause also decreased. In Europe there is a current trend towards an age decrease in the patients with bronchiolitis [5, 6].
As in other reports [7, 8], RSV was the main etiologic agent in our children hospitalized for bronchiolitis, accounting for 62.7% of cases. It would have been of interest to know the distribution of various viruses (including rhinovirus, influenza, bocavirus, parainfluenza, or human metapneumovirus) [3] in the non-RSV group, but the detection of other viruses was not uniform in our laboratory during the 12 years of retrospective study. Some of the RSV negative cases may also represent RSV infection that was not detected because the viral load was low, or due to a deficient sampling.
There is a regional seasonality of RSV bronchiolitis, and in temperate regions RSV epidemics occur in the winter months with annual and geographical variations in seasonal onset and duration [5, 9]. In our hospital, 97% of children admitted for RSV bronchiolitis clustered from November to March, seasonality similar to that previously reported from Spain and other Mediterranean countries [10, 11]. On the contrary, RSV negative bronchiolitis occurred year round with peaks between the months of January and March.
The use of different diagnostic tools in the management of bronchiolitis is still controversial. In our study, overall use of diagnostic tests did not significantly change during the study period. Despite recommendations to avoid a generalized use of chest X-rays in these patients there are reports indicating a high rate of chest X-rays in children with bronchiolitis [6]. In our case, 88% of the patients had a chest X-ray performed. In this study, atelectasis/condensation had a predictive value on outcome and was associated with an increase in ICU admission, oxygen need and length of hospital stay in RSV and non-RSV bronchiolitis. In addition, two patients were diagnosed with diaphragmatic hernia that would have been overlooked if the chest X-rays had not been performed. We think that chest X-rays should be recommended in all hospitalized bronchiolitis for the detection of congenital malformations, lung complications and its future consequences [12] as well as for prognosis.
The mortality and morbidity attributable to infection with RSV appears greatest in infants younger than 3 months of age and in those with known risk factors, especially prematurity, chronic lung disease and congenital heart disease [5, 13]. In our study, bronchiolitis-associated deaths occurred only in two patients with RSV bronchiolitis (2/1,495; 0.13%), a very low rate similar to that already published in Spain [10].
Our analysis selected the final outcome measured by oxygen need, mean hospital stay and ICU admission as the indicators of disease severity. In the multiple regression analyses, atelectasis/condensation, congenital heart disease and prematurity (<32 gestational weeks) were the main factors for a worst outcome in RSV and non-RSV bronchiolitis. In contrast, age was a protective factor. When we analyzed the effect of age groups, we observed that age less than two months was a factor strongly related to an increased risk of oxygen need and ICU admission. This is consistent with other studies in which infants aged less than 6–12 weeks were at higher risk of hospital admission for bronchiolitis [14, 15]. Criteria based on clinical observations have not proved to be efficient enough to predict a severe course or the need of hospital admission. For this reason, children with less than two months of age, even with mild bronchiolitis, could be considered for hospital admission. Unfortunately, admission criteria have not been well established in the different guidelines [16].
In our study, we have specifically focused on congenital heart disease and prematurity as risk factors of severe bronchiolitis. Previous reports have found that premature infants were at higher risk of admission for bronchiolitis [17]. Despite these findings we observed that children with a history of non-extreme prematurity (>32 gestational weeks) were not at higher risk of ICU admission. However, extreme prematurity and congenital heart disease were predictors of a worse outcome and should be considered as admission criteria.
The introduction of palivizumab reduced the rate of hospitalization for RSV bronchiolitis (from 11.9% to 2.1%) in a similar way to that described in the IRIS trial (from 13.25% to 3.95%) or the IMpact-RSV study (from 10.6% to 4.8%) [18, 19]. We also observed a reduction in ICU admission (from 3.1% to 0.3%) after palivizumab introduction, a similar finding to that observed in the IMpact trial (from 3% to 1.3%). Oxygen need and mechanical ventilation also decreased after the introduction of palivizumab.
Interestingly, we have observed a reduction in the hospitalization rate of non-RSV hospitalizations in preterm ≤32 weeks gestational age infants after palivizumab introduction. This finding was not observed in the IMpact trial. In the IRIS study a trend towards a reduction in non-RSV lower respiratory tract infections was observed but did not achieve statistical significance (p = 0.063). If confirmed, this finding could be caused by co-infection of RSV with other respiratory viruses. An initial RSV infection might trigger a respiratory inflammatory state and increase morbidity of a subsequent viral infection.
In this study we have compared the clinical course of bronchiolitis caused by RSV with RSV negative bronchiolitis. RSV positive patients had a longer length of hospital stay, were more frequently admitted to ICU, and had more oxygen requirements. In RSV bronchiolitis other co-morbidities such as atelectasis/condensation and AOM were also more common. These findings suggest that RSV bronchiolitis is a more severe illness compared to that caused by other viruses. In a recent study from the United States, Garcia et al. have reached a similar conclusion [20]. One of the major strengths of our study is that we have analyzed the risk factors for severe outcome of RSV versus non-RSV bronchiolitis separately, rather than describing the characteristics of the whole study group.
Several committees of the American Academy of Pediatrics have discussed the real utility of testing the etiologic diagnosis of bronchiolitis [21, 22], but most centers proceed to RSV detection advocating preventive reasons. Our study, apart from suggesting that RSV bronchiolitis is a more severe disease, shows that children with RSV bronchiolitis had a reduction in several diagnostic tests compared with RSV negative bronchiolitis. These findings suggest that etiologic diagnosis is not only useful for preventive purposes but also to determine prognosis and ultimately reduce other unnecessary diagnostic tests.
References
Shay DK, Holman RC, Newman RD, Liu LL, Stout JW, Anderson LJ (1999) Bronchiolitis-associated hospitalizations among US children, 1980-1996. JAMA 282:1440–1446
Mansbach JM, Emond JA, Camargo CA (2005) Bronchiolitis in US emergency departments 1992 to 2000. Epidemiology and practice variation. Pediatr Emerg Care 21:242–247
Manoha C, Espinosa S, Aho SL, Huet F, Pothier P (2007) Epidemiological and clinical features of hMPV, RSV and RVs infections in young children. J Clin Virol 38:221–226
Richard N, Komurian-Pradel F, Javouhey E, Perret M, Rajoharison A, Bagnaud A, Billaud G, Vernet G, Lina B, Floret D, Paranhos-Baccalà G (2008) The impact of dual viral infection in infants admitted to a pediatric intensive care unit associated with severe bronchiolitis. Pediatr Infect Dis J 27:213–217
Simoes E, Carbonell-Extrany X (2003) Impact of severe disease caused by respiratory syncytial virus in children living in developed countries. Pediatr Infect Dis J 22:S13–S22
Tsolia MN, Kafetzis D, Danelatou K, Astral H, Kallergi K, Spyridis P, Karpathios TE (2002) Epidemiology of respiratory syncytial virus bronchiolitis in hospitalized infants in Greece. Eur J Epidemiol 18:55–61
Purcell K, Driscoll FJ (2004) Children's hospital respiratory syncytial virus database: risk factors, treatment and hospital course in 3308 infants and young children, 1991 to 2002. Pediatr Infect Dis J 23:418–423
Calvo C, García-García ML, Blanco C, Vázquez MC, Frías ME, Pérez-Breña P, Casas I (2008) Multiple simultaneous viral infections in infants with acute respiratory tract infections in Spain. J Clin Virol 42:268–272
Stensballe LG, Devasundaram JK, Simoes EAF (2003) Respiratory syncytial virus epidemics: the ups and downs of a seasonal virus. Pediatr Infect Dis J 22:S21–S32
Alonso A, Andres JM, Garmendia JR, Diez I, Gil JM, Ardura J (2007) Bronchiolitis due to respiratory syncytial virus in hospitalized children: a study of seasonal rhythm. Acta Paediatr 96:731–735
Dagan R, Landau D, Haikin H, Tal A (1993) Hospitalization of Jewish and Bedouin infants in southern Israel for bronchiolitis caused by respiratory syncytial virus. Pediatr Infect Dis J 12:381–386
Piastra M, Polidori G, De Carolis MP, Tempera A, Caresta E, Pulitanò S, Chiaretti A, Valentini P, De Rosa G (2005) Fatal coronary artery anomaly presenting as bronchiolitis. Eur J Pediatr 164:515–519
Langley GF, Anderson LJ (2011) Epidemiology and prevention of respiratory syncytial virus infections among infants and young children. Pediatr Infect Dis J 30:510–517
Chan PW, Lok FY, Khatijah SB (2002) Risk factors for hypoxemia and respiratory failure in respiratory syncytial virus bronchiolitis. Southeast Asian J Trop Med Public Health 33:806–810
Boyce TG, Mellen BG, Mitchel EF, Wright PF, Griffin MR (2000) Rates of hospitalization for respiratory syncytial virus infection among children in medicaid. J Pediatr 137:865–870
Lind I, Gill JH, Calabretta N (2006) What are hospital admission criteria for infants with bronchiolitis? J Fam Practice 55:67–69
Heikkinen T, Valkonen H, Lehtonen L, Vainionpää R, Ruuskanen O (2005) Hospital admission of high risk infants for respiratory syncytial virus infection: implications for palivizumab prophylaxis. Arch Dis Child Fetal Neonatal Ed 90:F64–F68
Pedraz C, Carbonell-Estrany X, Figueras-Aloy J, Quero J, and the IRIS Study Group (2003) Effect of palivizumab prophylaxis in decreasing respiratory syncytial virus hospitalizations in premature infants. Pediatr Infect Dis J 22:823–827
The IMpact-RSV Study Group (1998) Palivizumab, a humanized respiratory syncytial virus monoclonal antibody, reduces hospitalization from respiratory syncytial virus infection in high-risk infants. Pediatrics 102:531–537
Garcia CG, Bhore R, Soriano-Fallas A, Trost M, Chason R, Ramilo O, Mejías A (2010) Risk factors in children hospitalized with RSV bronchiolitis versus non-RSV bronchiolitis. Pediatrics 126(6):e1453–1460
American Academy of Pediatrics Subcommittee on Diagnosis and Management of Bronchiolitis (2006) Diagnosis and management of bronchiolitis. Pediatrics 118:1774–1793
Harris JA, Huskins WC, Langley JM, Siegel JD, Pediatric Special Interest Group of the Society for Healthcare Epidemiology of America (2007) Health care epidemiology perspective on the October 2006 recommendations of the Subcommittee on Diagnosis and Management of Bronchiolitis. Pediatrics 120:890–892
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hervás, D., Reina, J., Yañez, A. et al. Epidemiology of hospitalization for acute bronchiolitis in children: differences between RSV and non-RSV bronchiolitis. Eur J Clin Microbiol Infect Dis 31, 1975–1981 (2012). https://doi.org/10.1007/s10096-011-1529-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-011-1529-y