Abstract
The purpose of this investigation was to analyse Streptococcus agalactiae (group B Streptococcus, GBS) isolates collected in Italy from vaginal and urine samples in respect to their clonality, distribution of virulence factors and antimicrobial resistance determinants. Three hundred and eighty-eight GBS were recovered from clinical samples. They were analysed for antibiotic resistance profiling. Erythromycin-resistant strains were further characterised by multilocus sequence typing (MLST), serotyping and the detection of alp genes of the alpha-like protein (Alp) family. GBS isolates represented 40 different sequence types (STs), grouped in five clonal complexes (CCs) and belonged to seven serotypes. Most serotype V strains (81%) possessed alp2-3; serotype Ia carried mainly epsilon, while the serotype III mainly rib. All isolates were susceptible to penicillin, whereas resistance to erythromycin was detected in 15% of isolates. Most erythromycin-resistant GBS strains were of serotype V (56.8%) and belonged to the CC-1 group (50%). Macrolide resistance phenotypes were the cMLSB (46.5%) and the M phenotypes (46.5%) due to the presence of ermB and mefA/E genes, respectively. These results provide data which establish a baseline for monitoring erythromycin resistance in this region and also provide an insight into the correlation among clonal types, serotypes, surface protein and resistance genes. The increased prevalence of strains that displayed the M phenotype strengthens the importance of the epidemiological surveillance of macrolide resistance in GBS, which may also represent an important reservoir of resistance genes for other species.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Streptococcus agalactiae (group B Streptococcus, GBS), a commensal of human gastrointestinal and genitourinary flora, is now the major cause of early-onset sepsis in newborns, as well as an important factor of post-partum maternal sepsis and late-onset invasive infections in infants. GBS is also increasingly isolated from bacteraemia, endocarditis, skin and soft tissue infections, pneumonia, and bone and joint infections in non-pregnant adults with underlying medical conditions [1]. β-lactam agents such as penicillin or ampicillin are the antibiotic agents of choice for the prophylaxis and treatment of GBS infections. Macrolides are the recommended second-line drugs and the first alternative in cases of β-lactam allergy. Resistance to the alternative drugs of choice for the treatment of GBS infections, including lincosamides such as clindamycin and macrolides such as erythromycin, has increased during the last decade in several countries, with some geographical variations [2–4]. The resistance is commonly caused by three genes: ermB, ermA (subclass ermTR) and mefA/E. Mechanisms which confer resistance to macrolide, lincosamide and streptogramin B (MLSB) antibiotics include target site modification by methylation of the 23SrRNA binding site. This mechanism is mediated by the ermB and ermTR genes, which confer cross-resistance to all MLSB antibiotics. Resistance can be either inducible (iMLSB ), where the methylase is produced in the presence of an inducer (such as erythromycin), or constitutive (cMLSB), where the methylase is produced constitutively [5]. The mefA and mefE genes, which are 90% identical, encode 14- and 15-member macrolide efflux pumps, respectively, and lead to the macrolide-only (M) resistance phenotype [6].
This increasing resistance to macrolides observed worldwide underlines the need for detailed studies on GBS resistance determinants and population structure. Among typing methods applied to GBS, multilocus sequence typing (MLST) possesses a high discriminatory power [7].
Capsular serotyping is the classical method used in epidemiological studies. Nine capsular types are recognised: Ia, Ib and II to VIII, along with a new provisional serotype IX, which has been recently proposed [8]. Comparison of the capsular locus genes suggested that the structural diversity of the capsular polysaccharide is associated with the genetic diversity of the capsular locus, possibly driven by horizontal gene transfer [9]. The capsular polysaccharide is a major GBS virulence factor and also the main target of antibody-mediated killing [7]. In the last decade, conjugated multivalent vaccines have been developed and proved to be highly immunogenic, raising the possibility of the prevention of perinatal GBS disease through maternal immunisation [10].
Proteins of the α-like protein (Alp) family play an important role in GBS pathogenesis and are also vaccine candidates [11]. The Alp family includes the alpha, Rib, Alp2, Alp3/R28, Alp4 and epsilon proteins, encoded by the allelic bca, rib, alp2, alp3, alp4 and alp1/alp5 genes, respectively, located on the pathogenicity island IV [12, 13].
The purpose of this paper was to characterise a collection of GBS isolated both from urine and vaginal samples by antimicrobial susceptibility testing, the presence of antimicrobial resistance genes, serotyping, MLST and analysis of the alp gene distribution.
Materials and methods
Strain collection
A total of 388 GBS isolates were collected between June 2009 and January 2010 from patients aged between 23 and 70 years (median 40.5 years) who visited Brescia’s main hospital (Spedali Civili); 265 originated from vaginal samples and 123 originated from urine samples. All strains were isolated from consecutive outpatients who for gynaecologic healthcare control, for normal routine screening during pregnancy or for the presence of symptoms of genital infections had attended Brescia’s hospital. GBS strains were isolated by streak plating 1 to 10 μl of transport medium onto chromID Strepto B agar plates (bioMérieux, St. Louis, MO, USA). The plates were incubated at 37°C for 18 to 24 h in aerobic conditions. GBS was selected by the production of a pink pigment when grown aerobically on chromID Strepto B agar. GBS identification was performed by means of the VITEK™ system (bioMérieux).
Alpha-like protein (Alp) genes and serotyping
Surface protein markers were detected by using a multiplex polymerase chain reaction (PCR) for the direct identification of the Alp protein genes [12]. Primer nucleotide sequences used as the reverse primers and the nucleotide sequence, common to all of the surface protein genes, used as the forward primer are reported in the Table 1. Capsular serotyping was carried out by latex agglutination method with anti-type Ia, Ib, II, III, IV, V, VI, VII and VIII sera (Statens Serum Institute, Copenhagen, Denmark; distributed in Italy by Biogenetics). Isolates that failed to type using the serotyping kit were deemed non-typable (NT) by latex agglutination.
MLST
DNA was extracted from each strain using a DNeasy kit (Qiagen). Internal fragments (size ~400–500 bp) of seven housekeeping genes, chosen for GBS characterisation by the use of MLST, were amplified from DNA extract by PCR. The seven loci were pheS (phenylalanyl transfer RNA synthetase), atr (amino-acid transporter protein), tkt (transketolase), glcK (glucose kinase), sdhA (L-serine dehydratase), glnA (glutamine synthetase) and adhP (alcohol dehydrogenase).
The MLST analysis of macrolide-resistant strains was performed as described elsewhere [7]. Alleles for the seven loci were analysed on the MLST website (http://pubmlst.org/sagalactiae), and its combination provided an allelic profile or sequence type (ST). The STs were grouped with the eBURST program [14] into clonal complexes (CCs) whose members shared at least five of the seven MLST loci [15]; otherwise, an ST was considered to be a singleton.
Antimicrobial resistance phenotype and determinants
Antimicrobial susceptibility was tested using VITEK2 (bioMérieux). VITEK2 susceptibility testing was performed according to the manufacturer’s instructions by using the AST-P586 card. The results obtained after a maximum of 15 h of incubation were analysed and interpreted by AES 4.02 software. The minimum inhibitory concentrations (MICs) determined by the system identified the class of microbial susceptibility as susceptible, intermediate or resistant according to the interpretative criteria published by Clinical and Laboratory Standards Institute (CLSI) guidelines [16]. The phenotypic characterisation of macrolide-resistant strains was performed by double-disc diffusion testing as described previously [17]. Erythromycin (15 μg) and clindamycin (2 μg) discs were placed 20 mm apart. Isolates resistant to erythromycin with blunting of the clindamycin inhibition were of the iMLSB phenotype, isolates that demonstrated resistance to both erythromycin and clindamycin were of the cMLSB phenotype, isolates showing resistance to erythromycin without blunting of the clindamycin inhibition zone were of the M phenotype and isolates resistant to clindamycin yet susceptible to erythromycin belonged to the L phenotype. Interpretative criteria were in accordance to the CLSI guidelines [16]. A multiplex PCR was used to identify the ermB, ermTR and mefA/E genes from the GBS strains, using primers (Table 2) and conditions previously reported [17, 18], and a separate PCR was used to amplify the linB gene [19, 20].
Statistical analysis
Fisher’s exact test was used to evaluate the differences in the distributions of isolates. A p-value of < 0.05 was considered to be significant.
Results
Serotypes and the alp family genes
All 58 GBS isolates resistant to macrolides were serotyped by the latex agglutination method. Four strains were non-typable (NT). Overall, the most represented serotypes isolated were types V (33 isolates), Ia (7 isolates) and III (6 isolates). Serotype Ib was represented by three isolates, while serotypes II and IV were represented by two isolates each. One strain belonged to serotype VI. No strains of serotypes VII and VIII were found. The presence of a particular Alp gene in relation to the serotype was also noted (Table 3). Of the 27 alp2-3-positive strains isolated, 22 were of serotype V; 9 of 17 epsilon-positive strains corresponded to serotype V and five corresponded to serotype Ia; rib-positive strains were present in almost all of the serotypes isolated. Conversely, a certain serotype commonly corresponded to a particular Alp gene: serotype Ib and II presented rib, serotype IV carried either rib and epsilon, most serotype V strains (81%) possessed alp2-3, serotype Ia carried mainly epsilon, while serotype III carried mainly rib. Different associations of alp genes were presented in a single strain.
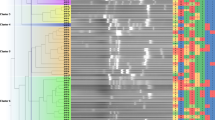
MLST of GBS
The MLST analysis of 58 macrolide-resistant strains demonstrated the existence of different genetic lineages, inclusively among strains expressing the same serotype (Table 4). In particular, 40 STs were observed. Despite the high number, all STs were grouped into five CCs; 11 singleton STs were identified that were not a part of a cluster. The eBURST groups were: CC-1 (including STs: 1, 2, 6, 86, 153, 170, 186, 196, 242, 297, 318, 333, 364, 433, 436, 455, 466; n = 29, 50%); CC-46 (including STs: 46, 243, 268, 273; n = 5, 8.6%); CC-24 (including STs: 24, 33, 163, 444; n = 4, 6.8%); CC-27 (including STs: 106, 181; n = 3, 5.1%); CC-352 (including ST-352 and ST-460; n = 2, 3.4%) and singletons (STs: 55, 129, 168, 171, 185, 198, 231, 247, 413, 434, 457, 461, 480; n =15 (25.8%). There was a statistically significant association (p < 0.05) between CC-1 and the surface protein alp2-3 and epsilon genes, and between CC-1 and serotype V. Furthermore, a statistically significant correlation was observed between CC-27 and the surface protein rib gene.
Macrolide resistance phenotypes and genotypes
Erythromycin resistance was possessed by 15% of the strains (58 out of 388). Most of the resistant isolates (33 isolates, 56.8%) belonged to serotype V. The majority of resistant isolates belonged to the cluster CC-1 (29/58, 50%). Fifty-four of 58 erythromycin-resistant isolates displayed half the cMLSB resistance phenotype and the other half the M resistance phenotype, while the iMLSB phenotype was found in four isolates (Table 5).
We isolated four strains with unidentified antibiotic resistance genotypes. These unknown resistant strains were found to have the cMLSB resistance phenotypes. Most of the screened strains presented solely a single resistance gene. An exception occurred for five strains that exhibited a combination of ermB and mefA/E genes (four isolates) and of ermB and ermA genes (subclass ermTR) (one isolate). Twenty-two GBS strains carried the ermB gene and twenty-seven possessed the mefA/E gene (Table 4). All ermB gene-positive isolates expressed the cMLSB resistance phenotype, while the M resistance phenotype was expressed by all of the isolates found to carry the mefA/E gene.
Discussion
One of the properties specific for GBS seems to be a remarkably clonal population structure, with strong differences in the degree of divergence within particular clonal groups. In this study, 58 isolates belonged to 40 STs. Other studies showed the presence of various STs among the collection of isolates [7, 15, 21]. Despite this high genetic diversity, the STs belonged to relatively few CCs, five in this study. The degree of variability of pathogenic factors, such as serotype and surface protein genes, differed for various CCs. Some CCs such as CC27 are more homogeneous, while others, e.g. CC1 and CC23, are much more internally variable [7, 15, 22]. These differences among CCs may be due to different capabilities for horizontal gene transfer, whose mechanism remains unclear in GBS.
It has been hypothesised previously that the spread of strains of particular surface protein profiles and serotypes reflects the selection of the best evolutionary lineages by the immune system [13]. In this study, we found that the five major CCs comprised isolates presenting serotype–surface protein gene combinations (serotype V-alp2-3; serotype III-rib) already reported [13, 23].
Nonetheless, a different combination (serotype Ia–epsilon) was observed in this study, suggesting that new successfully selected clones may be emerging.
Among the 58 GBS strains studied, all capsular serotypes except VII and VIII were found. Globally, serotype V (56.8%) was the most common, followed by serotypes Ia (12%) and III (10%), contrasting with the low prevalence of serotypes Ib (5%), II and IV (3.4%). However, other studies showed a predominance of other serotypes (IV in the United Arab Emirates, and VI to VIII in Japan) [24, 25], which could reflect the specificities of immune responses that may vary according to the studied population.
In our study, the majority of resistant isolates belonged to serotype V and the CC-1 clonal group, and such an association was already found [4].
Other studies have also identified serotype V GBS strains associated with erythromycin resistance [26–28].
For a long time, GBS remained fully susceptible to penicillin [3, 4, 29], the first-line drug used in the treatment and prophylaxis of infections caused by this pathogen. The current alternatives for patients allergic to penicillin include macrolides and lincosamides. However, 19% of the S. agalactiae isolates were resistant to erythromycin and 53% of these presented resistance to clindamycin [30]. Regarding the erythromycin resistance among strains of S. agalactiae, our results (15%) were similar to what has already been observed in Italy, Spain, Portugal, Germany, France and Canada [4, 29, 31–34], but differ considerably from the 3.8% reported in the Czech Republic [35] and 38–41.9% reported in the United States [3, 17]. Together with social determinants and differences of healthcare structures, the factors most frequently associated with these large discrepancies in antimicrobial resistance are the antibiotic consumption and its inappropriate use [36]. The erythromycin resistance level observed, i.e. 15%, indicates the need for careful surveillance in the future, especially as the first penicillin-non-susceptible GBS were reported in USA and Japan [37, 38]; this dangerous phenomenon may lead to the further limitation of treatment options.
In our study, there was a predominance of cMLSB and M phenotypes, indicating that erythromycin resistance was mediated by the two principal mechanisms: methylation of 23S ribosomal RNA, determined by erm genes, and active drug efflux by pumps encoded by mef genes. To our knowledge, this is the first time that this high proportion of M phenotypes has been reported in Italy (46.5%). It has important implications. Firstly, on the laboratory reporting of clindamycin susceptibility results, as clindamycin can be reported as susceptible, and, secondly, it may influence the antibiotic choice, as clindamycin may still be a therapeutic option, even if the organism is resistant to erythromycin.
There were four isolates in the collection for which no resistance mechanism was found. These isolates may harbour mutations in genes coding for 23S rRNA or ribosomal proteins L4 and L22. Interestingly, there was one isolate of the cMLSB phenotype that had both ermA subclass ermTR and ermB genes; the coexistence of both genes has been documented previously [39]. Also, four isolates that displayed M phenotypes harboured both mefA/E, genes as well as ermB genes. This finding implies differential gene expression, as only the mefA/E gene was expressed.
In summary, GBS strains isolated represent a complex population where the detection of a correlation among clonal clusters, serotypes, surface-associated proteins and resistance genes show a clonal spread.
Finally, as erythromycin resistance rates in GBS have increased, continued surveillance is advisable and local statistics will be of crucial value in guiding empirical antibiotic therapy. It also highlights the role of efflux on macrolide resistance in GBS, which may have an impact on antibiotic choice in clinical practice. The current study provides a baseline from which future trends in macrolide resistance can be monitored.
References
Baker CJ (2000) Group B streptococcal infections. In: Stevens DL, Kaplan EL (eds) Streptococcal infections: clinical aspects, microbiology, and molecular pathogenesis. Oxford University Press, New York, pp 222–237
Acikgoz ZC, Almayanlar E, Gamberzade S, Gocer S (2004) Macrolide resistance determinants of invasive and noninvasive group B streptococci in a Turkish hospital. Antimicrob Agents Chemother 48:1410–1412
Borchardt SM, DeBusscher JH, Tallman PA, Manning SD, Marrs CF, Kurzynski TA, Foxman B (2006) Frequency of antimicrobial resistance among invasive and colonizing Group B streptococcal isolates. BMC Infect Dis 6:57
Gherardi G, Imperi M, Baldassarri L, Pataracchia M, Alfarone G, Recchia S, Orefici G, Dicuonzo G, Creti R (2007) Molecular epidemiology and distribution of serotypes, surface proteins, and antibiotic resistance among group B streptococci in Italy. J Clin Microbiolol 45:2909–2916
Leclercq R (2002) Mechanisms of resistance to macrolides and lincosamides: nature of the resistance elements and their clinical implications. Clin Infect Dis 34:482–492
Arpin C, Daube H, Tessier F, Quentin C (1999) Presence of mefA and mefE genes in Streptococcus agalactiae. Antimicrob Agents Chemother 43:944–946
Jones N, Bohnsack JF, Takahashi S, Oliver KA, Chan MS, Kunst F, Glaser P, Rusniok C, Crook DWM, Harding RM, Bisharat N, Spratt BG (2003) Multilocus sequence typing system for group B Streptococcus. J Clin Microbiol 41:2530–2536
Slotved HC, Kong F, Lambertsen L, Sauer S, Gilbert GL (2007) Serotype IX, a proposed new Streptococcus agalactiae serotype. J Clin Microbiol 45:2929–2936
Cieslewicz MJ, Chaffin D, Glusman G, Kasper D, Madan A, Rodrigues S, Fahey J, Wessels MR, Rubens CE (2005) Structural and genetic diversity of group B Streptococcus capsular polysaccharides. Infect Immun 73:3096–3103
Sinha A, Lieu TA, Paoletti LC, Weinstein MC, Platt R (2005) The projected health benefits of maternal group B streptococcal vaccination in the era of chemoprophylaxis. Vaccine 23:3187–3195
Gilbert GL (2004) Vaccines for other neonatal infections: are group B streptococcal infections vaccine-preventable? Expert Rev Vaccines 3:371–374
Creti R, Fabretti F, Orefici G, von Hunolstein C (2004) Multiplex PCR assay for direct identification of group B streptococcal α-protein-like protein genes. J Clin Microbiol 42:1326–1329
Lindahl G, Stålhammar-Carlemalm M, Areschoug T (2005) Surface proteins of Streptococcus agalactiae and related proteins in other bacterial pathogens. Clin Microbiol Rev 18:102–127
Feil EJ, Li BC, Aanensen DM, Hanage WP, Spratt BG (2004) eBURST: inferring patterns of evolutionary descent among clusters of related bacterial genotypes from multilocus sequence typing data. J Bacteriol 186:1518–1530
Bisharat N, Jones N, Marchaim D, Block C, Harding RM, Yagupsky P, Peto T, Crook DW (2005) Population structure of group B Streptococcus from a low-incidence region for invasive neonatal disease. Microbiology 151:1875–1881
Clinical and Laboratory Standards Institute (CLSI) (2010) Performance standards for antimicrobial susceptibility testing, M100-S20 (2010), M02-A10 and M07-A8. CLSI, Wayne, PA
Gygax SE, Schuyler JA, Kimmel LE, Trama JP, Mordechai E, Adelson ME (2006) Erythromycin and clindamycin resistance in group B streptococcal clinical isolates. Antimicrob Agents Chemother 50:1875–1877
Sutcliffe JA, Grebe T, Tait-Kamradt A, Wondrack L (1996) Detection of erythromycin-resistant determinants by PCR. Antimicrob Agents Chemother 40:2562–2566
De Azavedo JCS, Yeung RH, Bast DJ, Duncan CL, Borgia SB, Low DE (1999) Prevalence and mechanisms of macrolide resistance in clinical isolates of group A streptococci from Ontario, Canada. Antimicrob Agents Chemother 43:2144–2147
Desjardins M, Delgaty KL, Ramotar K, Seetaram C, Toye B (2004) Prevalence and mechanisms of erythromycin resistance in group A and group B Streptococcus: implications for reporting susceptibility results. J Clin Microbiol 42:5620–5623
Sadowy E, Matynia B, Hryniewicz W (2010) Population structure, virulence factors and resistance determinants of invasive, non-invasive and colonizing Streptococcus agalactiae in Poland. J Antimicrob Chemother 65:1907–1914
Brochet M, Couvé E, Zouine M, Vallaeys T, Rusniok C, Lamy MC, Buchrieser C, Trieu-Cuot P, Kunst F, Poyart C, Glaser P (2006) Genomic diversity and evolution within the species Streptococcus agalactiae. Microbes infect 8:1227–1243
Quentin R, Huet H, Wang FS, Geslin P, Goudeau A, Selander RK (1995) Characterization of Streptococcus agalactiae strains by multilocus enzyme genotype and serotype: identification of multiple virulent clone families that cause invasive neonatal disease. J Clin Microbiol 33:2576–2581
Amin A, Abdulrazzaq YM, Uduman S (2002) Group B streptococcal serotype distribution of isolates from colonized pregnant women at the time of delivery in United Arab Emirates. J Infect 45:42–46
Lachenauer CS, Kasper DL, Shimada J, Ichiman Y, Ohtsuka H, Kaku M, Paoletti LC, Ferrieri P, Madoff LC (1999) Serotypes VI and VIII predominate among group B streptococci isolated from pregnant Japanese women. J Infect Dis 179:1030–1033
Diekema DJ, Andrews JI, Huynh H, Rhomberg PR, Doktor SR, Beyer J, Shortridge VD, Flamm RK, Jones RN, Pfaller MA (2003) Molecular epidemiology of macrolide resistance in neonatal bloodstream isolates of group B streptococci. J Clin Microbiol 41:2659–2661
Lin FY, Azimi PH, Weisman LE, Philips JB 3rd, Regan J, Clark P, Rhoads GG, Clemens J, Troendle J, Pratt E, Brenner RA, Gill V (2000) Antibiotic susceptibility profiles for group B streptococci isolated from neonates, 1995–1998. Clin Infect Dis 31:76–79
von Both U, Ruess M, Mueller U, Fluegge K, Sander A, Berner R (2003) A serotype V clone is predominant among erythromycin-resistant Streptococcus agalactiae isolates in a southwestern region of Germany. J Clin Microbiol 41:2166–2169
Figueira-Coelho J, Ramirez M, Salgado MJ, Melo-Cristino J (2004) Streptococcus agalactiae in a large Portuguese teaching hospital: antimicrobial susceptibility, serotype distribution, and clonal analysis of macrolide-resistant isolates. Microb Drug Resist 10:31–36
Florindo C, Viegas S, Paulino A, Rodrigues E, Gomes JP, Borrego MJ (2010) Molecular characterization and antimicrobial susceptibility profiles in Streptococcus agalactiae colonizing strains: association of erythromycin resistance with subtype III-1 genetic clone family. Clin Microbiol Infect 16(9):1458–1463
Fluegge K, Supper S, Siedler A, Berner R (2004) Antibiotic susceptibility in neonatal invasive isolates of Streptococcus agalactiae in a 2-year nationwide surveillance study in Germany. Antimicrob Agents Chemother 48:4444–6
Gonzalez JJ, Andreu A; Spanish Group for the Study of Perinatal infection from the Spanish Society for Clinical Microbiology and Infectious Diseases (2005) Multicenter study of the mechanisms of resistance and clonal relationships of Streptococcus agalactiae isolates resistant to macrolides, lincosamides, and ketolides in Spain. Antimicrob Agents Chemother 49:2525–2527
de Azavedo JC, McGavin M, Duncan C, Low DE, McGeer A (2001) Prevalence and mechanisms of macrolide resistance in invasive and noninvasive group B streptococcus isolates from Ontario, Canada. Antimicrob Agents Chemother 45:3504–3508
Fitoussi F, Loukil C, Gros I, Clermont O, Mariani P, Bonacorsi S, Le Thomas I, Deforche D, Bingen E (2001) Mechanisms of macrolide resistance in clinical group B streptococci isolated in France. Antimicrob Agents Chemother 45:1889–1891
Motlová J, Straková L, Urbásková P, Sak P, Sever T (2004) Vaginal and rectal carriage of Streptococcus agalactiae in the Czech Republic: incidence, serotypes distribution and susceptibility to antibiotics. Indian J Med Res 119:84–87
Bronzwaer SL, Cars O, Buchholz U, Mölstad S, Goettsch W, Veldhuijzen IK, Kool JL, Sprenger MJ, Degener JE; European Antimicrobial Resistance Surveillance System (2002) A European study on the relationship between antimicrobial use and antimicrobial resistance. Emerg Infect Dis 8:278–282
Dahesh S, Hensler ME, Van Sorge NM, Gertz RE Jr, Schrag S, Nizet V, Beall BW (2008) Point mutation in the group B streptococcal pbp2x gene conferring decreased susceptibility to β-lactam antibiotics. Antimicrob Agents Chemother 52:2915–2918
Kimura K, Suzuki S, Wachino J, Kurokawa H, Yamane K, Shibata N, Nagano N, Kato H, Shibayama K, Arakawa Y (2008) First molecular characterization of group B streptococci with reduced penicillin susceptibility. Antimicrob Agents Chemother 52:2890–2897
Bingen E, Fitoussi F, Doit C, Cohen R, Tanna A, George R, Loukil C, Brahimi N, Le Thomas I, Deforche D (2000) Resistance to macrolides in Streptococcus pyogenes in France in pediatric patients. Antimicrob Agents Chemother 44:1453–1457
Acknowledgements
We are sincerely obliged to Ilaria Medeghini for her excellent technical assistance
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
De Francesco, M.A., Caracciolo, S., Gargiulo, F. et al. Phenotypes, genotypes, serotypes and molecular epidemiology of erythromycin-resistant Streptococcus agalactiae in Italy. Eur J Clin Microbiol Infect Dis 31, 1741–1747 (2012). https://doi.org/10.1007/s10096-011-1495-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-011-1495-4