Abstract
The introduction of a pneumococcal conjugate vaccine in Venezuela needs previous studies to assess vaccine efficiency. We conducted a survey of nasopharyngeal pneumococcal carriage in urban children in Caracas and studied the distribution of serotypes. We compared these data with survey data available for invasive strains isolated in the same area and in the same time period. An overall pneumococcal carriage rate of 27% was observed. The most predominant capsular serotypes among carriage isolates were 6B (29%), 19A (13.8%), 23F (10%), 14 (8.3%), 6A (8.3%) and 15B/C (3.3%) and among invasive isolates 6B (25%), 14 (15%), and 19A, 6A, 7F, and 18 (7.5% each). The serotypes/groups 1, 5, 7F and 18, jointly covering 30% of the invasive strains, represented less than 0.7% of the carrier strains. The theoretical coverage of the pneumococcal conjugate vaccine PCV13 for carriage and invasive strains was calculated to be 74% and 90%, respectively. Our study demonstrates important differences for the serotype distribution in disease and carriage isolates and provides a key baseline for future studies addressing the prevalence and replacement of invasive and carriage serotypes after the introduction of the PCV 13 vaccine in Venezuela in the year 2010.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Streptococcus pneumoniae is part of the commensal flora of the upper respiratory tract, colonizing the nasopharyngeal niche. Though colonization with pneumococci is mostly without clinical symptoms, it can progress towards non-invasive and even invasive disease. In addition, pneumococcal carriage is an important source of horizontal spread of this pathogen within the community [1]. The factors that permit pneumococci to spread upon colonization are poorly characterized, and are likely to vary due to differences in virulence characteristics of the organism, e.g. differences in capsular polysaccharide structures, and the immunological state of the host [2, 3].
Pneumococcal carriage studies have been used as an indicator to predict serotype distribution and susceptibility patterns of invasive isolates and to calculate theoretical vaccine coverage [4–7]. However, some serotypes are more frequently associated with nasopharyngeal carriage, whereas others more frequently cause invasive disease [8].
The objective of this study was to determine the prevalence of pneumococcal carriage, the distribution of pneumococcal serotypes, the antibiotic resistance patterns among pneumococi and risk factors for carriage in healthy urban children in Caracas, Venezuela. These data were compared with existing survey data from children with invasive pneumococcal infection in Caracas, collected in the same time-frame, allowing calculation of the relative invasive disease potential of the serotypes.
Materials and methods
Study population
Nasopharyngeal samples were taken from 1,004 healthy children aged 3–65 months attending the Healthy Children Service at Hospital de Niños "J.M. de Los Rios" in Caracas between December 2006 and January 2008. All children were examined during the visit by a pediatrician. Children with an underlying chronic illness (e.g. HIV positive, sickle cell anemia, asplenia, cancer) were not included in the study.
The research protocol was approved by the Ethics Committee of Hospital de Niños "J.M. de Los Rios”. Signed informed consent was obtained from a parent or guardian of each child. Written questionnaires about demographics and medical history were completed by the pediatrician by interviewing one or both parents. Questions involved breast-feeding, day-care attendance, number of family members, number of siblings, smoking habits of family members living in the same household (passive smoking >10 cigarettes at day), living conditions (urban or rural area), use of antibiotics in the last 7, 30 and 60 days, history of upper respiratory tract infections (otitis, sinusitis, rhinitis) or lower respiratory tract infections (pneumonia, bronchitis). Social stratification (scale 1 to 6) was performed by the Graffar method modified by Mendez Castellano. This method is based on four variables: profession of the head of the family, educational level of the mother, main source of income and housing conditions. Following the instructions of the method, we stratified the sample into three levels: low income (scale 4 + 5 + 6), medium income (scale 3) and high income (scale 1 + 2).
Nasopharyngeal sampling
Nasopharyngeal samples were obtained with a flexible swab (Copan Italia) and transported in STGG transport medium at 4–7°C to the Laboratory of the “Instituto de Biomedicina” in Caracas, Venezuela; the samples were plated on blood agar with and without gentamycin and the plates were incubated overnight at 36°C in a CO2-enriched atmosphere. S. pneumoniae isolates were identified according to standard microbiological procedures.
Drug susceptibility testing
Susceptibility of the pneumococcal strains was tested by the disk diffusion method in accordance with the guidelines of the Clinical and Laboratory Standards Institute (CLSI) [9]. Penicillin resistance was screened with 1-μg oxacillin disks (Oxoid). The other antimicrobial drugs (Oxoid) tested were erythromycin (cut-off 15 μg/ml), clindamycin (cut-off 2 μg/ml), tetracycline (cut-off 30 μg/ml), levofloxacin (cut-off 5 μg/ml), linezolid (cut-off 30 μg/ml) and vancomycin (cut-off 30 μg/ml).
Capsular serotyping
A sequential multiplex PCR [10] and the capsular swelling method (Quellung reaction) with commercially available antisera (Statens Serum Institut) were used for determining capsular pneumococci serotypes. For the identification of the 6C serotype only a PCR based assay was used [11].
Invasive pneumococcal isolates
The data of invasive isolates in the same study period were provided by the Regional Report of SIREVA II, available on line on the webpage of Pan American Health Organization [12]. SIREVA is a surveillance program of pneumonia and meningitis caused by H. influenzae, N. meningitidis and S. pneumoniae in children of Latin America and the Caribbean. Venezuela has been part of the program since the year 1998.
Data analysis
Statistical analysis was performed by SPSS version 15.0 for Windows. For the determination of carriage risk factors chi-square test was used for univariate analysis with a 2-sided p < 0.05 considered to be statistically significant. The variables that had p values in univariate analysis of <0.10 were analyzed with a multivariate logistic regression model using the stepwise backward Wald method to confirm independence.
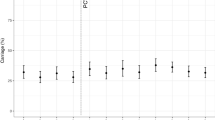
For the estimation of the invasiveness due to the individual serotypes, an empirical odds ratio (OR) was calculated by reference to all the other serotypes or groups using a method published elsewhere [13]. An OR of 1 indicated that the serotype was equally likely to be recovered from invasive disease or from nasopharyngeal carriage, an OR >1 indicated an increased probability for a serotype to cause invasive disease, and an OR <1 indicated a reduced probability for a serotype to cause invasive disease.
Results
Pneumococcal carriage and risk factors
For the carriage study a total of 1,004 children were enrolled and the demographic and clinical characteristics of the study population are summarized in Table 1. The mean age of the children was 16.2 months and the average family size was 5.4 persons. Most children were from the urban centre of Caracas and about 10% lived in a suburb or rural area. In total, 276 pneumococcal isolates were collected of 271 children corresponding with an overall carriage rate for S. pneumoniae of 27% with 1.8% of children (5/271) carrying two different serotypes. No significant difference for the carriage rate was found for the time of the year sampling was performed. Pneumococcal carriage rates of males and females were similar (p = 0.56). Determinants of pneumococcal carriage with univariate analysis were daycare attendance (p = 0.005), presence of siblings (p = 0.006), socio-economical status (p = 0.006), previous antibiotic use (< 7 days) (p = 0.017) and family size (p = 0.010). No significant difference was found for history of URTI or LRTI, breast feeding and parental smoking. When these factors were analyzed by multivariate logistic regression, daycare attendance (odds ratio [OR] 1.63, 95% CI 1.19–2.24) and presence of siblings (OR 1.45 95% CI 1.03–2.03) were positively associated with pneumococcal carriage, whereas previous antibiotic consumption (<7 days) showed a negative association with pneumococcal carriage (Table 2).
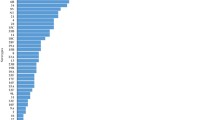
Serotyping of the pneumococcal isolates demonstrated that the most predominant capsular serogroups/serotypes were 6B (29%), 19A (13.8%), 23F (10%), 14 (8.3%), 6A (8.3%) and 15B/C (3.3%). A total of 74% of the isolated strains were serotypes covered by the 13-valent conjugate vaccine. Furthermore, serotype 6C was not detected in this study. With respect to the age-related distribution of pneumococcal serotypes, no statistical differences were observed between age groups.
Comparison of carriage and invasive isolates
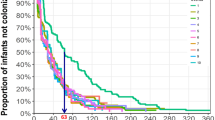
When comparing the serotypes of our study with invasive serotypes registered in 2007 in the Regional Report of SIREVA II [12], we observed that serogroup 6, serotype 19A and serotype 14 accounted for 59.4% (n = 164) of the nasopharyngeal isolates and 55% (n = 22) of invasive isolates with only a minor difference between the prevalence of these serotypes in carriers or diseased children (Fig. 1). However, serotype 23F was significantly more common in carriers (10.1% versus 2.5%) and 19F in invasive disease (5% versus 1.4%). Serotypes 1 and 5 were only recovered from patients with invasive disease, and serotype 7F and 18 were isolated only once from carriers.
The serotype distribution observed for carriage and invasive disease isolates indicates a theoretical coverage of PCV13 of 74% and 90%, respectively. The proportion of carriage isolates displaying serotypes covered by PCV13 was 80% among children aged 0–12 months and 25–36 months, and 100% for children aged 49–65 months (Fig. 2a). For invasive disease isolates the theoretical coverage for PCV13 was 100% among children aged 25–36 months (Fig. 2b).
To compare the probability of invasive disease due to individual serotypes an empirical odds ratio (OR) was calculated using all the other serotypes as reference (Table 3). Among vaccine serotypes/serogroups 18 and 7F were significantly associated with invasive disease (OR ≥16). Serotype 19F, 3 and 14 displayed an invasive disease OR >1, and serotypes 6B, 6A and 19A displayed an invasive disease OR <1, although none of these values reached statistical significance (Table 3).
Resistance to antibiotics
Overall, 50% of pneumococcal isolates in our carriage study were resistant to at least one antibiotic tested, with 35% of the strains resistant to cotrimoxazole, followed by erythromycin (30%), penicillin (28%) and tetracycline (26%). No resistance to vancomycin or linezolid was observed. Multi-drug resistance (resistance to 3 or more drugs) was found in 18% of the strains. Serotypes associated with antibiotic-resistance in carriers were predominantly the serotypes 6B (64%) and 23 F (40%). No significant difference was found for resistance rates between carriage and invasive isolates.
Discussion
This is the first large-scale study to determine carriage rates, serotype distribution, risk factors and antibiotic resistance patterns of S. pneumoniae in urban children in Venezuela. Our study provides a baseline, which allows study of the expected changes in serotype distribution in carriage and invasive disease due to the introduction of the PCV13 vaccination. Currently, the vaccine is not part of the national immunization program in Venezuela, and only available through private hospitals. However, the Ministry of Health has announced the application for all Venezuelan children by the end of 2010.
A total of 1,004 healthy children with a mean age of 16.2 months were enrolled in this study; 30% of them attended daycare centres. The pneumococcal carriage rate of 27% in our study is similar or lower compared with other reports from Latin American countries like Mexico (21.4%), Brazil (35.8%) and Chile (41%) [14–16]. We excluded the possibility that the relatively low carriage rate could have been caused by inadequate sample transport or bad laboratory practice. We have previously shown very high pneumococcal carriage rates of more than 70% in Warao children in Venezuela [17]. For that study, nasopharyngeal samples were transported on ice for up to 5 days before being cultured on blood agar, apparently without affecting the viability of S. pneumoniae. A possible reason for the relatively low carriage rate might be the fact that this survey addressed only healthy children with no signs of a lower/upper respiratory infection at moment of sampling. It is well known that the colonization rates are higher in children with a respiratory tract infection or otitis media compared to healthy populations [1]. In our study any child with signs of upper or lower respiratory tract infection was excluded.
Positive risk factors for pneumococcal carriage in our cohort were daycare attendance and presence of siblings. These findings are in accordance with studies performed by others [18]. Recent antibiotic use showed a negative correlation with pneumococcal carriage.
Interestingly, the serotype distribution in Caracas in carriers differs significantly from the distribution of serotypes in an indigenous population in Venezuela, where in 2006 the most predominant capsular serotypes were 23F (19.6%), 6A (19.6%), 15B (10.5%), 6B (9.2%), 19F (7.2%), 14 (4.6%) and 19A (3.3%) [17]. This clearly shows that in the same country the serotype distribution in carriers can vary greatly among different populations.
The results of the carriage study were compared with the data of invasive isolates for Caracas reported by SIREVA. Overall, the distribution of the serotypes observed in the carriage study matched with the distribution of the serotypes for invasive diseases. For example, serotype 6B was the most important invasive and carriage serotype, counting for 21% and 30% of the isolates, respectively. There was also good concordance between invasive isolates and carriage for the serotypes 19A and 6A. Data of the collaborative SIREVA project [19] showed that between 2000 and 2005 the serotype 14 was the most important invasive isolate in children in Venezuela, accounting for more than 35% of strains. However, in the year 2007 (the year of our carriage study), the above-described carriage study and the SIREVA study for invasive isolates coincide in that this serotype was of minor importance and represented only 7.6 % and 12.5% of the carriage and invasive isolates, respectively. A remarkable discrepancy between carriage and invasive isolates was found for other serotypes. In the carriage study serotypes 1 and 5 were not isolated and serogroup/serotype 18 and 7F only once, in contrast with a significant prevalence of those serotypes among the isolates causing pediatric invasive disease, i.e. 30% of the invasive isolates. Serotypes 1, 7F and 14 were identified as highly invasive but were hardly found in the nasopharynx [20]. In addition, it has been hypothesized that, because of their virulence, serotypes 1 and 5 are rarely detected in carriage studies, as they have a very short stay at the nasopharynx prior to invasive disease [20, 21]. Hence, these serotypes will only rarely be found in carriage studies, even in populations in which they contribute to a high portion of invasive disease isolates [8]. No such information is available for serotype 18, which was isolated from 7.5% of the children in Caracas with invasive disease but less than 1% isolated in this carriage study. In our study the most invasive serotypes were 18, 7F 19F, 3 and 14 with invasive disease ORs >1. In two other studies performed in very different geographic regions in the world, i.e. Papua New Guinea and the United Kingdom, serogroup 18 and serotypes 7F and 14 were also identified as invasive disease serotypes. However, in these studies serotype 19F and 3 were considered not very invasive, showing ORs of 0.6 and 0.3, respectively [13, 22]. This suggests that for these serotypes the capsular polysaccharide is not the only important factor determining the invasiveness of these strains as stated by Breuggemann et al. [13], but that additional factors also influence the invasiveness.
The serotype distribution in carriers and for children with invasive disease indicates a theoretical coverage of 74% and 90%, respectively, for pneumococcal conjugate PCV13 vaccine. The high theoretical coverage of the PCV13 vaccine in comparison with the PCV7 vaccine is mainly due to the serotype 19A, which is significantly present in both carriage and disease in our country. Worldwide, serotype 19A has been reported as an emerging serotype, accounting for an important number of cases of invasive disease, most probably because this serotype has no coverage with the currently licensed pneumococcal conjugate vaccine [23, 24].
The prevalence of antibiotic susceptibility for invasive and nasopharyngeal isolates is comparable and similar to the prevalence of resistance observed in other countries in Latin America [25, 26]. A total of 70% of the drug-resistant strains were VT types implying that the conjugates vaccine is potentially able to reduce the prevalence of drug-resistant pneumococci in our population.
In conclusion, our study demonstrates that the nasopharyngeal isolates reflect the distribution of serotypes/groups observed during invasive disease and susceptibility patterns observed in the invasive disease isolates, although there are differences in rank and some minor invasive serotypes were not isolated among carriers. In developing countries, monitoring pneumococcal carriage is an important and useful ‘surrogate’ tool for serotype prevalence surveillance, as most hospitals lack appropriate microbiology facilities to culture invasive disease isolates. Our study provides important baseline information for future follow-up studies in Caracas upon introduction of PCV13 in the national program, and indicates that children from Caracas will potentially benefit from PCV13 vaccination.
References
Bogaert D, De Groot R, Hermans PW (2004) Streptococcus pneumoniae colonisation: the key to pneumococcal disease. Lancet Infect Dis 4(3):144–154
Gray BM, Converse GM 3rd, Dillon HC Jr (1980) Epidemiologic studies of Streptococcus pneumoniae in infants: acquisition, carriage, and infection during the first 24 months of life. J Infect Dis 142(6):923–933
Hausdorff WP, Bryant J, Kloek C, Paradiso PR, Siber GR (2000) The contribution of specific pneumococcal serogroups to different disease manifestations: implications for conjugate vaccine formulation and use, part II. Clin Infect Dis 30(1):122–140
Mastro TD, Nomani NK, Ishaq Z, Ghafoor A, Shaukat NF, Esko E, Leinonen M, Henrichsen J, Breiman RF, Schwartz B et al (1993) Use of nasopharyngeal isolates of Streptococcus pneumoniae and Haemophilus influenzae from children in Pakistan for surveillance for antimicrobial resistance. Pediatr Infect Dis J 12(10):824–830
Lehmann D, Gratten M, Montgomery J (1997) Susceptibility of pneumococcal carriage isolates to penicillin provides a conservative estimate of susceptibility of invasive pneumococci. Pediatr Infect Dis J 16(3):297–305
Berezin EN, Cardenuto MD, Ferreira LL, Otsuka M, Guerra ML, Brandileone MC (2007) Distribution of Streptococcus pneumoniae serotypes in nasopharyngeal carriage and in invasive pneumococcal disease in Sao Paulo, Brazil. Pediatr Infect Dis J 26 (7):643–645. doi:10.1097/INF.0b013e3180616d0f00006454-200707000-00019
Lauderdale TL, Wagener MM, Lin HM, Huang IF, Lee WY, Hseih KS, Lai JF, Chiou CC (2006) Serotype and antimicrobial resistance patterns of Streptococcus pneumoniae isolated from Taiwanese children: comparison of nasopharyngeal and clinical isolates. Diagn Microbiol Infect Dis 56 (4):421–426. doi:10.1016/j.diagmicrobio.2006.06.006
Hausdorff WP, Feikin DR, Klugman KP (2005) Epidemiological differences among pneumococcal serotypes. Lancet Infect Dis 5(2):83–93
CLSI (2008) Performance standards for antimicrobial susceptibility testing; Eighteenth informational supplement. CLSI Document M100-S18. Clinical and Laboratory Standards Institute, Wayne, PA
Pai R, Gertz RE, Beall B (2006) Sequential multiplex PCR approach for determining capsular serotypes of Streptococcus pneumoniae isolates. J Clin Microbiol 44(1):124–131
Carvalho Mda G, Pimenta FC, Gertz RE, Jr., Joshi HH, Trujillo AA, Keys LE, Findley J, Moura IS, Park IH, Hollingshead SK, Pilishvili T, Whitney CG, Nahm MH, Beall BW (2009) PCR-based quantitation and clonal diversity of the current prevalent invasive serogroup 6 pneumococcal serotype, 6 C, in the United States in 1999 and 2006 to 2007. J Clin Microbiol 47 (3):554–559. doi:10.1128/JCM.01919-08
OPS (2008) Informe Regional de SIREVA II, 2007. Datos por país y por grupos de edad sobre las características de los aislamientos de Streptococcus pneumoniae, Haemophilus influenzae y Neisseria meningitidis, en procesos invasores. Documentos Tecnicos. Tecnologías Esenciales de Salud. THR/EV- 2008/001
Brueggemann AB, Griffiths DT, Meats E, Peto T, Crook DW, Spratt BG (2003) Clonal relationships between invasive and carriage Streptococcus pneumoniae and serotype- and clone-specific differences in invasive disease potential. J Infect Dis 187(9):1424–1432
Solorzano-Santos F, Ortiz-Ocampo LA, Miranda-Novales MG, Echaniz-Aviles G, Soto-Nogueron A, Guiscafre-Gallardo H (2005) Prevalence of Streptococcus pneumoniae serotypes on nasopharyngeal colonization in children of Mexico City. Salud Pública Méx 47(4):276–281
Laval CB, de Andrade AL, Pimenta FC, de Andrade JG, de Oliveira RM, Silva SA, de Lima EC, Fabio JL, Casagrande ST, Brandileone MC (2006) Serotypes of carriage and invasive isolates of Streptococcus pneumoniae in Brazilian children in the era of pneumococcal vaccines. Clin Microbiol Infect 12(1):50–55
Lagos RMA, San Martín O, Seoane M, Maldonado A, Hormazábal JC, Loyola H, Levine MM (2006) Nasopharyngeal (NP) carriage of Streptococcus pneumoniae (S.pn) in a cohort of healthy Chilean new born infants (NBI) followed from age 0 to 24 months (mos). Paper presented at the 5th international symposium on pneumococci and pneumococcal diseases (ISPPD5), Alice Springs, Australia
Rivera-Olivero IA, Bogaert D, Bello T, del Nogal B, Sluijter M, Hermans PW, de Waard JH (2007) Pneumococcal carriage among indigenous Warao children in Venezuela: serotypes, susceptibility patterns, and molecular epidemiology. Clin Infect Dis 45(11):1427–1434
Bogaert D, Engelen MN, Timmers-Reker AJ, Elzenaar KP, Peerbooms PG, Coutinho RA, de Groot R, Hermans PW (2001) Pneumococcal carriage in children in The Netherlands: a molecular epidemiological study. J Clin Microbiol 39(9):3316–3320
Spadola E, Fernandez S, Payares D, Tarazona B, Gabastou J, de Waard JH (2009) Distribucion de serotipos de Streptococcus pneumoniae causantes de enfermedad invasiva en niños menores de 5 años en Venezuela durante los años 1999–2007. Revista de Salud por los Niños de las Americas "SALUDARTE2 7(1):31–41
Porat N, Trefler R, Dagan R (2001) Persistence of two invasive Streptococcus pneumoniae clones of serotypes 1 and 5 in comparison to that of multiple clones of serotypes 6B and 23 F among children in southern Israel. J Clin Microbiol 39(5):1827–1832
Hausdorff WP, Bryant J, Paradiso PR, Siber GR (2000) Which pneumococcal serogroups cause the most invasive disease: implications for conjugate vaccine formulation and use, part I. Clin Infect Dis 30(1):100–121
Smith T, Lehmann D, Montgomery J, Gratten M, Riley ID, Alpers MP (1993) Acquisition and invasiveness of different serotypes of Streptococcus pneumoniae in young children. Epidemiol Infect 111(1):27–39
Pelton SI, Huot H, Finkelstein JA, Bishop CJ, Hsu KK, Kellenberg J, Huang SS, Goldstein R, Hanage WP (2007) Emergence of 19A as virulent and multidrug resistant pneumococcus in Massachusetts following universal immunization of infants with pneumococcal conjugate vaccine. Pediatr Infect Dis J 26 (6):468–472. doi:10.1097/INF.0b013e31803df9ca00006454-200706000-00003
Ardanuy C, Rolo D, Fenoll A, Tarrago D, Calatayud L, Linares J (2009) Emergence of a multidrug-resistant clone (ST320) among invasive serotype 19A pneumococci in Spain. J Antimicrob Chemother 64 (3):507–510. doi:10.1093/jac/dkp210
Camargos P, Fischer GB, Mocelin H, Dias C, Ruvinsky R (2006) Penicillin resistance and serotyping of Streptococcus pneumoniae in Latin America. Paediatr Respir Rev 7(3):209–214. doi:10.1016/j.prrv.2006.04.004
Agudelo CI, Castaneda E, Corso A, Regueira M, de Brandileone MC, Brandao AP, Maldonado A, Hormazabal JC, Tamargo I, Echaniz-Aviles G, Soto A, Viveros MG, Hernandez I, Chamorro G, Weiler N, Sanchez J, Feris JM, Camou T, Garcia G, Spadola E, Payares D, Gabastou JM, Di Fabio JL (2009) Resistance to non-beta-lactam antibiotics in the clinical isolates of Streptococcus pneumoniae of children in Latin America. SIREVA II, 2000–2005. Rev Panam Salud Pública 25(4):305–313
Acknowledgements
This study was financially supported by research grants 0887X1-8802 from Wyeth Venezuela CA. We are grateful to the pediatric department “Niños Sanos” of the Children Hospital JM de los Rios, Caracas, Venezuela, especially Dr. Anabela Fernandez and Dr. Yecenia Pérez, and also of the Tuberculosis Laboratory Xiomara Brito and Domingo Ramos for technical assistance. Both Ismar Rivera-Olivero and Berenice del Nogal are considered first authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rivera-Olivero, I.A., del Nogal, B., Sisco, M.C. et al. Carriage and invasive isolates of Streptococcus pneumoniae in Caracas, Venezuela: the relative invasiveness of serotypes and vaccine coverage. Eur J Clin Microbiol Infect Dis 30, 1489–1495 (2011). https://doi.org/10.1007/s10096-011-1247-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-011-1247-5