Abstract
The soluble form of urokinase-type plasminogen activator receptor (suPAR) is a new inflammatory marker. High suPAR levels have been shown to associate with mortality in cancer and in chronic infections like HIV and tuberculosis, but reports on the role of suPAR in acute bacteremic infections are scarce. To elucidate the role of suPAR in a common bacteremic infection, the serum suPAR levels in 59 patients with Staphylococcus aureus bacteremia (SAB) were measured using the suPARnostic™ ELISA assay and associations to 1-month mortality and with deep infection focus were analyzed. On day three, after the first positive blood culture for S. aureus, suPAR levels were higher in 19 fatalities (median 12.3; range 5.7–64.6 ng/mL) than in 40 survivors (median 8.4; range 3.7–17.6 ng/mL, p = 0.002). This difference persisted for 10 days. The presence of deep infection focus was not associated with elevated suPAR levels as compared to patients with no deep infection focus. suPAR was found to be prognostic for mortality in receiver operator characteristic (ROC) curve analysis, which was not observed for serum C-reactive protein (CRP); the area under the curve (AUC) for suPAR was 0.754 (95% confidence interval [CI], 0.615–0.894, p = 0.003) and for CRP, it was 0.596 (95% CI, 0.442–0.750, p = 0.253). The optimal suPAR cut-off value in predicting 1-month mortality was 9.25 ng/mL. In conclusion, our study demonstrates that the new promising biomarker, serum suPAR concentration, was able to predict mortality in SAB.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Staphylococcus aureus is the second most common pathogen in bacteremic infections, and it still carries high mortality [1, 2]. The clinical course of S. aureus bacteremia (SAB) is determined by its complications, particularly by the development of deep infections and thromboembolic events [3–6]. Prognostic markers that would assist in the detection of complications or risk of mortality would be useful in order to allocate the use of limited healthcare resources to those who would benefit the most.
At least 170 different biomarkers have been evaluated for clinical use in bacteremic infections, but only a few are used in daily clinical practice [7]. Low protein C levels were shown to correlate to increased mortality in sepsis [8]. The use of protein C in diagnostics is helpful in the most severely ill patients [8]. Procalcitonin (PCT) has been shown to be useful in assessing the severity of sepsis. PCT has been found to be useful in discerning bacterial infections from other causes of inflammatory response [9]. C-reactive protein (CRP) is a part of an acute phase response [10] and it is used in the detection of sepsis or organ dysfunction [11]. In everyday practice, CRP changes have been used to observe the treatment response, while the decline of CRP level has been shown to be one of the earliest markers of improved condition [12]. Though CRP seems to be a good marker of systemic inflammation and an important clinical tool in severe infections [13], it has not been found to be helpful as a prognostic factor [14]. A biomarker that would be easy and rapid to analyze and would predict complications and risk for mortality in severe bacteremic infections is still needed.
Soluble urokinase plasminogen activator receptor (suPAR) is a new promising biomarker. suPAR is the soluble form of the urokinase-type plasminogen activator receptor (uPAR/CD87), which is expressed on several different cell types, including monocytes, macrophages, and neutrophils [15, 16]. suPAR is derived from proteolytical cleavage and release from the cell membrane-bound uPAR [17]. suPAR is present in various sites, such as serum or plasma, urine, and cerebrospinal fluid [18–20]. Elevated suPAR levels have been shown to reflect the level of inflammation and immune activation [21, 22], and have been associated with poor prognosis in a number of chronic infectious diseases, such as HIV [23], tuberculosis [24], and in certain types of cancer [24–26].
Plasma suPAR levels might be useful also in acute infections, although the exact biochemical and molecular mechanisms of its function have not yet been described in detail [27]. uPAR/CD87 has been released in patients with urosepsis [28]. Elevated plasma suPAR levels ≥10.1 ng/mL on admission have been detected to be markers of poor prognosis in pneumococcal bacteremia [29]. In Plasmodium falciparum malaria, the serum levels of suPAR were associated with the degree of parasitemia in children [30]. However, in systemic inflammatory response syndrome (SIRS), suPAR had only a limited value as a single marker in detecting bacterial causes from non-bacterial causes of inflammation [31].
The aim of the present study was to evaluate whether serum suPAR levels could be useful in the detection of complications like deep infection foci or risk for mortality in SAB by using a new commercially available assay to analyze plasma suPAR levels.
Patients and methods
Patient population
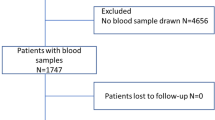
Patients with SAB and belonging to one of the three groups, (1) patients with fatal outcome, (2) patients with a deep infection focus, and (3) patients without deep infection focus, were included from a larger prospective study. The aim was to include at least 15 patients in each group where serum samples from the first 10 days after the positive blood culture for SAB were available (with the exception of deceased patients). In total, 59 numerically ordered patients were included for this study from only one study site, Helsinki University Central Hospital.
The original prospective study consisted of 430 patients with blood culture positive for S. aureus recruited consecutively from five university hospitals and seven tertiary care hospitals in Finland between January and May 1999 and between January 2000 and August 2002 [6]. The trial aimed primarily to examine the potential of two fluoroquinolones (trovafloxacin or levofloxacin) to reduce the high mortality and complication rates in SAB, when added to the standard treatment. The exclusion criteria have been published earlier in the original article [6]. Each patient was recruited into the study only once in order to avoid double inclusion in repeated bacteremia. The protocol was approved by the ethics committees of all study sites. Written informed consent was obtained from all patients or their representatives.
Definitions
Intravenous drug users (IDUs) were defined as patients who had injected drugs within the past 6 months before randomization based on a history taken on admission. SAB was hospital-acquired if the first positive blood culture was obtained ≥48 h after admission or the patient was a resident in a long-term care facility or had attended hemodialysis within the preceding two months. Prognosis or severity of underlying diseases were characterized as healthy, nonfatal, or ultimately or rapidly fatal disease according to the criteria of McCabe and Jackson [32]. Infection focus was documented by clinical, bacteriological, radiological, or pathological investigations. Intravenous catheter-associated bacteremia was defined using the guidelines of the Infectious Disease Society of America (IDSA) [33]. Deep infection focus was classified as endocarditis, pneumonia, deep-seated abscess, osteomyelitis, septic arthritis, meningitis, septic thrombophlebitis, mediastinitis, urinary tract infection, infection of a prosthetic device, or recurrent SAB, as described in our previously published article [34]. Altered mental status was classified as unconsciousness or severe confusion.
Analytical methods
The serum samples were drawn on average on the third, fourth, or tenth day, and one month after the first positive blood culture and stored frozen at −70°C until analyzed. The mean time interval from the blood culture to the first suPAR sample collection was three days (standard deviation [SD] 1.1; range 2–5 days). The suPAR level was measured using the suPARnostic™ kit (ViroGates, Copenhagen, Denmark) (V-suPAR), as described in detail elsewhere [31]. The kit comes with catching monoclonal antibody pre-coated plates and a horseradish peroxidase (HRP)-labeled detection monoclonal antibody, which is added to the sample dilution buffer. Then, 25 μl of sample is mixed with 225 μl of dilution buffer and 100 μl in duplicates are added to the pre-coated plate and incubated for 1 h. Following washing, 100 μl of substrate is added for 20 min and the reaction stopped with 100 μl 0.5 M H2SO4. The plates are measured at 450 nM with a reference distance of 630 nM. The within-assay coefficient of variation (CV) was 3.4% and the inter-assay CV was 4.11%. The CVs were comparable to those reported in the manufacturer’s kit insert of 2.7% and 3.0%, respectively.
Serum concentrations of CRP were measured in the study site laboratory by standard laboratory methods. The serum or plasma (use of plasma instead of serum commenced 18.3.2002) was subjected to automatic immunoturbidimetric analysis using the analyzers 917 or Modular PP Analyzer (Hitachi Ltd., Tokyo, Japan) and Tina-quant CRP reagents (Roche Diagnostics). The normal value of CRP concentration was <10 mg/L for both methods.
Statistics
Statistical analyses were performed using SPSS® version 17.0 (SPSS Inc., Chicago, IL, USA). The associations between categorical variables were analyzed by the χ2-test or Fisher’s exact test, as appropriate. Odds ratios (ORs) with 95% confidence intervals (CIs) were calculated in order to estimate the significance of differences in the groups. Non-parametric comparisons between groups were done using the Kruskal–Wallis H- and the Mann–Whitney U-tests. In the multivariate logistic regression analysis, covariates were added in a stepwise method in the order of strength of their association with the outcome variable. When a new explanatory variable was shown to contribute to the variance, its influence on the variables already in the model and possible collinearity with them was assessed. All tests were two-tailed and p < 0.05 was considered as significant.
Results
Patients were divided into three groups, i.e., those with a fatal outcome (n = 19) and those with a verified deep infection (n = 25) and without deep infection focus (n = 15) (Table 1). All deceased patients also had a deep infection focus: they differed from the other groups by being significantly older and more often having a fatal underlying disease, and none of them were IDUs (Table 1).
The serum suPAR levels were significantly higher in patients who died compared to the two groups of surviving patients on the third, fourth, and tenth days after the first positive blood culture for S. aureus (Table 2, Fig. 1a). No difference was observed in the serum suPAR concentrations between surviving patients with a deep infection focus or without it. In addition, no differences in suPAR levels between any patient groups were found one month after the bacteremic event. However, at this time point, there were only two patients left in the patient group with fatal outcome.
Serum soluble urokinase plasminogen activator receptor (suPAR) concentrations in 59 patients on the third day after the first positive blood culture for Staphylococcus aureus. In a, the patients have been divided into three groups according to outcome: those with a fatal outcome during 30 days and those with and without a deep infection focus. In b, the patients are divided according to the 30-day mortality. The number of patients in each group is shown below at the bottom of the figure and the horizontal lines denote the median suPAR concentration
To investigate the value of suPAR as a prognostic marker for fatal outcome, the patient material was dichotomized based on the one-month survival. The suPAR levels on days three, four, ten, and 30 were compared according to survival. On day three, the median suPAR level of the fatalities was significantly higher (12.3 ng/mL; n = 19, range 5.7–64.6 ng/mL) than the median suPAR level of the survivors (8.4 ng/mL; n = 40, range 3.7–17.6 ng/mL) (p = 0.002) (Fig. 1b). The difference in suPAR levels remained significant for the entire first week: on day four, the median suPAR level of the fatalities was 11.50 ng/mL (n = 18, range 4.70–20.60 ng/mL) and of the survivors, it was 7.1 ng/mL (n = 40, range 2.50–15.20 ng/mL) (p = 0.001). On day seven, the median suPAR concentration of the fatalities was 11.75 ng/mL (n = 16, range 6.10–17.80 ng/mL) and of the survivors, it was 6.5 ng/mL (n = 40, range 2.3–17.30 ng/mL) (p < 0.0001).
To analyze possible confounding factors or selection bias in the patient material, we also analyzed associations of the patient characteristics and underlying diseases with the one-month mortality. Out of the patients with fatal outcome, 14 (74%) were >65 years old as compared to 14 (35%) survivors (p = 0.011). Ultimately or rapidly fatal underlying diseases were found in 14 (74%) fatalities as compared to only 12 (30%) survivors (p = 0.002). Differences in the distribution of age >65 years (OR, 5.2; 95% CI, 1.6–17.4; p = 0.011), underlying diseases (OR, 6.5; 95% CI, 1.9–22.2; p = 0.002), and suPAR levels >9.25 ng/mL (OR, 7.8; 95% CI, 2.2–28.2; p = 0.002) were all significantly associated with the mortality. Moreover, differences in the clinical parameters at the beginning of SAB (during the first three days after the first positive blood culture) were assessed based on the survival. Altered mental status during the first three days was associated with the mortality (OR, 4.1, 95% CI, 1.1–15.3; p = 0.042). In addition, during the first three days, three patients among the fatalities were given treatment for hypotension, while none of the survivors needed it (p = 0.030), but no OR was calculated due to the insufficient number of patients.
Receiver operator curve (ROC) characteristics were calculated for day three suPAR levels and compared with CRP in order to analyze the sensitivity of these markers as predictors of fatal outcome (Fig. 2). The area under the curve (AUC) of the ROC curve was significant only for suPAR (p = 0.003). The optimal cut-off value for suPAR on day three was 9.25 ng/mL [sensitivity 0.79 (95% CI, 0.69–0.88), specificity 0.68 (95% CI, 0.61–0.75), and positive likelihood ratio 2.5].
Receiver operator characteristic (ROC) curves of serum suPAR and C-reactive protein (CRP) with respect to the one-month mortality in Staphylococcus aureus bacteremia. The ROC curve for suPAR is shown by the continuous line and for CRP by the dashed line. The area under the curve (AUC) (95% CI) for day three suPAR was 0.754 (0.615–0.894) (p = 0.003) and for day three CRP, it was 0.596 (95% CI, 0.442–0.750) (p = 0.253)
In the multivariate binary logistic regression analysis for the one-month mortality, covariates tested in the same model were suPAR dichotomized at 9.25 ng/mL and the presence of cerebral symptoms on the first three days (Table 3). In this analysis, suPAR was found to be independently associated with the increased mortality (OR, 8.0; 95% CI, 2.1–30.5; p = 0.002), while presence of cerebral symptoms was not (OR, 4.3; 95% CI, 1.3–13.9; p = 0.059). Other factors showing an association with the one-month mortality were age >65 years and ultimately or rapidly fatal underlying disease according to McCabe’s classification. However, both age and fatal underlying diseases were collinear with dichotomized suPAR, and to avoid confounding in the analysis, they were not analyzed together with the suPAR. Due to the limited number of cases, the need for treatment for hypotension in the beginning of the SAB was omitted from the multivariate analysis.
Discussion
In the present study, serum suPAR levels were evaluated for the first time in SAB. Serum suPAR concentrations at the beginning of SAB were found to be significantly higher in fatalities than in survivors. This difference remained significant in repeated measurements on days three, four, and ten after the first positive blood culture. However, a deep infection focus was not associated with elevated suPAR levels on any day. Only elevated suPAR level significantly predicted mortality and it showed higher sensitivity and specificity than the CRP level.
Our findings are in accordance with the two previous studies on pneumococcal bacteremia which showed that suPAR concentrations were significantly higher in patients with fatal outcome as compared to surviving patients [29, 35]. In one of these studies, the CRP level had no predictive value for mortality [29], whereas in the other study, CRP also predicted fatal outcome [35]. In these studies, suPAR levels were measured only once either on admission or 12–36 h after the positive blood culture was achieved. Our results clearly indicate that the predictive value of suPAR is not affected by the time point of measurement. Elevated suPAR levels during the first 10 days of SAB could, at any time, predict fatal outcome. The predictive value of suPAR measurement in gram-negative bacteria is still not known, but suPAR levels have been reported to be elevated approximately to the same level as in our study [28]. Together with this data, it indicates that high suPAR concentrations are predictive for fatal outcome in bacteremic gram-positive infections.
It was surprising that high suPAR levels were not associated with deep infection foci. This has not been investigated previously. In one study of pneumococcal bacteremia, patients with multiple infection sites were excluded [29] and in another study including patients with either pneumonia or meningitis, the possible impact of multiple infection sites to suPAR levels was not analyzed [35]. Deep infection foci seem to be very common in SAB and they were found in 84% of the patients in our study and with equally high occurrence in other studies as well [4, 6, 28]. The high prevalence of deep infection foci might be one reason why suPAR levels did not differ in patients with a deep infection focus or without. However, suPAR might not be diagnostic in finding deep infection foci and it has been claimed to be a more prognostic than diagnostic marker in infections [29, 31].
Elevated suPAR levels have been found to reflect the level of inflammation and immune activation [21, 22], but the mechanisms behind predicting effect for the mortality are not clarified. The fact is that high suPAR levels have been associated with poor prognosis also in more slowly progressing infections like HIV [23] and tuberculosis [24], or even in certain cancers [24–26]. The suPAR levels that discern the risk of mortality seem to be variable in different infections. In HIV, higher two-year mortality was attributed to values of suPAR >6 ng/mL [36]. In a large patient cohort from West Africa without any observed infection, a log-linear relationship was found between suPAR levels <15 ng/mL and increased mortality [37]. In SAB, we found that suPAR with a cut-off value of 9.25 ng/mL was predictive for mortality. This value is comparable to cut-off values in earlier pneumococcal studies, where cut-off values of 10 ng/mL and 10.3 ng/mL were presented [29, 35]. In our material, suPAR concentrations above 9.25 ng/mL had a specificity of 0.68 and a sensitivity of 0.79 for mortality, which lie within the acceptable range for a clinical measurement. suPAR concentrations below this had a negative predictive value (NPV) of 0.87, but levels above this limit had a positive predictive value (PPV) of only 0.54. We presented that individual variation in suPAR concentrations was quite wide, as evidenced by Fig. 1. Although high suPAR levels were predictive for mortality, many surviving patients also had high suPAR concentrations above the cut-off level, suggesting that high levels should be interpreted with caution in an individual patient. In our study, the patient samples were serum instead of plasma, which was used in previous studies. Serum has been shown to have slightly higher suPAR concentrations compared to plasma [38]. However, serum and plasma suPAR levels are strongly correlated, but the use of serum can partly explain the detected individual variations in suPAR levels.
suPAR measurements are shown to be higher in older persons [39] and this correlation was confirmed in the present study. Patients over 65 years of age had significantly higher suPAR levels than younger patients. We found that advanced age >65 years and, also, the presence of fatal underlying diseases were strongly correlated to higher mortality. Both of these factors have also previously been related to higher mortality in SAB [3, 5]. However, we could not clarify the relationship between age and underlying diseases on suPAR levels as predictors for mortality because these parameters could not be analyzed together in a multivariate analysis due to linkage. Females have been shown to have slightly higher suPAR concentrations as compared to males, which was not observed in our study [40].
In conclusion, we demonstrated that the new promising biomarker, serum suPAR concentration, was able to predict mortality in SAB. The results encourage future studies where the mechanism of this association could be clarified and the mortality predictive association confirmed in a larger patient cohort.
References
Conterno LO, Wey SB, Castelo A (1998) Risk factors for mortality in Staphylococcus aureus bacteremia. Infect Control Hosp Epidemiol 19(1):32–37
Benfield T, Espersen F, Frimodt-Møller N et al (2007) Increasing incidence but decreasing in-hospital mortality of adult Staphylococcus aureus bacteraemia between 1981 and 2000. Clin Microbiol Infect 13(3):257–263
Mylotte JM, Tayara A (2000) Staphylococcus aureus bacteremia: predictors of 30-day mortality in a large cohort. Clin Infect Dis 31(5):1170–1174
Fowler VG Jr, Olsen MK, Corey GR et al (2003) Clinical identifiers of complicated Staphylococcus aureus bacteremia. Arch Intern Med 163(17):2066–2072
Fätkenheuer G, Preuss M, Salzberger B et al (2004) Long-term outcome and quality of care of patients with Staphylococcus aureus bacteremia. Eur J Clin Microbiol Infect Dis 23(3):157–162
Ruotsalainen E, Järvinen A, Koivula I et al (2006) Levofloxacin does not decrease mortality in Staphylococcus aureus bacteraemia when added to the standard treatment: a prospective and randomized clinical trial of 381 patients. J Intern Med 259(2):179–190
Pierrakos C, Vincent JL (2010) Sepsis biomarkers: a review. Crit Care 14(1):R15
Yan SB, Helterbrand JD, Hartman DL, Wright TJ, Bernard GR (2001) Low levels of protein C are associated with poor outcome in severe sepsis. Chest 120(3):915–922
Hatzistilianou M (2010) Diagnostic and prognostic role of procalcitonin in infections. ScientificWorldJournal 10:1941–1946
Black S, Kushner I, Samols D (2004) C-reactive protein. J Biol Chem 279(47):48487–48490
Póvoa P (2002) C-reactive protein: a valuable marker of sepsis. Intensive Care Med 28(3):235–243
Póvoa P, Coelho L, Almeida E et al (2006) Early identification of intensive care unit-acquired infections with daily monitoring of C-reactive protein: a prospective observational study. Crit Care 10(2):R63
Lobo SM, Lobo FR, Bota DP et al (2003) C-reactive protein levels correlate with mortality and organ failure in critically ill patients. Chest 123(6):2043–2049
Silvestre J, Póvoa P, Coelho L et al (2009) Is C-reactive protein a good prognostic marker in septic patients? Intensive Care Med 35(5):909–913
Blasi F, Carmeliet P (2002) uPAR: a versatile signalling orchestrator. Nat Rev Mol Cell Biol 3(12):932–943
Plesner T, Behrendt N, Ploug M (1997) Structure, function and expression on blood and bone marrow cells of the urokinase-type plasminogen activator receptor, uPAR. Stem Cells 15(6):398–408
Huai Q, Mazar AP, Kuo A et al (2006) Structure of human urokinase plasminogen activator in complex with its receptor. Science 311(5761):656–659
De Witte H, Sweep F, Brünner N et al (1998) Complexes between urokinase-type plasminogen activator and its receptor in blood as determined by enzyme-linked immunosorbent assay. Int J Cancer 77(2):236–242
Sier CF, Sidenius N, Mariani A et al (1999) Presence of urokinase-type plasminogen activator receptor in urine of cancer patients and its possible clinical relevance. Lab Invest 79(6):717–722
Garcia-Monco JC, Coleman JL, Benach JL (2002) Soluble urokinase receptor (uPAR, CD 87) is present in serum and cerebrospinal fluid in patients with neurologic diseases. J Neuroimmunol 129(1–2):216–223
Ostrowski SR, Piironen T, Høyer-Hansen G et al (2005) High plasma levels of intact and cleaved soluble urokinase receptor reflect immune activation and are independent predictors of mortality in HIV-1-infected patients. J Acquir Immune Defic Syndr 39(1):23–31
Fevang B, Eugen-Olsen J, Yndestad A et al (2009) Enhanced levels of urokinase plasminogen activator and its soluble receptor in common variable immunodeficiency. Clin Immunol 131(3):438–446
Sidenius N, Sier CF, Ullum H et al (2000) Serum level of soluble urokinase-type plasminogen activator receptor is a strong and independent predictor of survival in human immunodeficiency virus infection. Blood 96(13):4091–4095
Eugen-Olsen J, Gustafson P, Sidenius N et al (2002) The serum level of soluble urokinase receptor is elevated in tuberculosis patients and predicts mortality during treatment: a community study from Guinea-Bissau. Int J Tuberc Lung Dis 6(8):686–692
Sier CF, Sidenius N, Mariani A et al (1999) Presence of urokinase-type plasminogen activator receptor in urine of cancer patients and its possible clinical relevance. Lab Invest 79(6):717–722
Sier CF, Stephens R, Bizik J et al (1998) The level of urokinase-type plasminogen activator receptor is increased in serum of ovarian cancer patients. Cancer Res 58(9):1843–1849
Thunø M, Macho B, Eugen-Olsen J (2009) suPAR: the molecular crystal ball. Dis Markers 27(3):157–172
Florquin S, van den Berg JG, Olszyna DP et al (2001) Release of urokinase plasminogen activator receptor during urosepsis and endotoxemia. Kidney Int 59(6):2054–2061
Wittenhagen P, Kronborg G, Weis N et al (2004) The plasma level of soluble urokinase receptor is elevated in patients with Streptococcus pneumoniae bacteraemia and predicts mortality. Clin Microbiol Infect 10(5):409–415
Perch M, Kofoed P, Fischer TK et al (2004) Serum levels of soluble urokinase plasminogen activator receptor is associated with parasitemia in children with acute Plasmodium falciparum malaria infection. Parasite Immunol 26(5):207–211
Kofoed K, Andersen O, Kronborg G et al (2007) Use of plasma C-reactive protein, procalcitonin, neutrophils, macrophage migration inhibitory factor, soluble urokinase-type plasminogen activator receptor, and soluble triggering receptor expressed on myeloid cells-1 in combination to diagnose infections: a prospective study. Crit Care 11(2):R38
Jackson GG, Arana-Sialer JA, Andersen BR, Grieble HG, McCabe WR (1962) Profiles of pyelonephritis. Arch Intern Med 110:63–75
Mermel LA, Farr BM, Sherertz RJ et al (2001) Guidelines for the management of intravascular catheter-related infections. Clin Infect Dis 32(9):1249–1272
Ruotsalainen E, Sammalkorpi K, Laine J et al (2006) Clinical manifestations and outcome in Staphylococcus aureus endocarditis among injection drug users and nonaddicts: a prospective study of 74 patients. BMC Infect Dis 6:137
Møller HJ, Moestrup SK, Weis N et al (2006) Macrophage serum markers in pneumococcal bacteremia: prediction of survival by soluble CD163. Crit Care Med 34(10):2561–2566
Schneider UV, Nielsen RL, Pedersen C et al (2007) The prognostic value of the suPARnostic ELISA in HIV-1 infected individuals is not affected by uPAR promoter polymorphisms. BMC Infect Dis 7:134
Rabna P, Andersen A, Wejse C et al (2009) High mortality risk among individuals assumed to be TB-negative can be predicted using a simple test. Trop Med Int Health 14(9):986–994
Lomholt AF, Christensen IJ, Høyer-Hansen G et al (2010) Prognostic value of intact and cleaved forms of the urokinase plasminogen activator receptor in a retrospective study of 518 colorectal cancer patients. Acta Oncol 49(6):805–811
Andersen O, Eugen-Olsen J, Kofoed K, Iversen J, Haugaard SB (2008) Soluble urokinase plasminogen activator receptor is a marker of dysmetabolism in HIV-infected patients receiving highly active antiretroviral therapy. J Med Virol 80(2):209–216
Stephens RW, Pedersen AN, Nielsen HJ et al (1997) ELISA determination of soluble urokinase receptor in blood from healthy donors and cancer patients. Clin Chem 43(10):1868–1876
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mölkänen, T., Ruotsalainen, E., Thorball, C.W. et al. Elevated soluble urokinase plasminogen activator receptor (suPAR) predicts mortality in Staphylococcus aureus bacteremia. Eur J Clin Microbiol Infect Dis 30, 1417–1424 (2011). https://doi.org/10.1007/s10096-011-1236-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-011-1236-8