Abstract
Methicillin-resistant Staphylococcus aureus (MRSA) infections are increasingly being reported among cystic fibrosis (CF) populations worldwide. In this paper, we sought to examine at the epidemiology, the molecular characterisation and the antibiotic resistance of MRSA isolates in our cohort of CF patients. All MRSA strains were collected prospectively at the University Hospital of Catania, Italy, during a two-year study between mid 2005 to mid 2007 and underwent molecular, pathotype and susceptibility characterisations. Our study demonstrates persisting infections with both hospital-associated (HA-) and community-associated (CA-)MRSA, including Panton–Valentine leukocidin (PVL)-positive strains, in our CF population with an overall prevalence of 7.8%. We demonstrated that, in these patients, persistence was sustained by either identical clones that underwent subtle changes in their toxin content or by different clones over time. The isolation of MRSA in our CF population aged 7–24 years was associated with an increased severity of the disease even if, due to the small sample of patients included and the paucity of data on the clinical outcome, these results cannot be conclusive. Furthermore, three strains were heteroresistant vancomycin-intermediate S. aureus (hVISA), questioning the use of glycopeptides in the treatment of MRSA infections in these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There has recently been an increasing number of reports worldwide dealing with the isolation of Staphylococcus aureus, particularly methicillin-resistant S. aureus (MRSA), in cystic fibrosis (CF) patients, with prevalences ranging from 0.1% in 1995 to 18.9% today [1–3].
Despite this increasing frequency of isolation and the serious potential morbidity from MRSA in these patients, very little is known about its clinical significance and even less is known about the molecular characteristics of the virulence and resistance of these clones.
With regard to the clinical significance of MRSA in the lung of CF patients deterioration of the lung function and MRSA isolation was addressed in many papers, but the importance of isolating this microorganism was poorly stressed; however, in a recent longitudinal study, the persistent presence of MRSA correlated with worsening X-ray images, leading to significantly more courses of intravenous antibiotics affecting patient growth and, eventually, to a more rapid decline in lung function [4–9].
With regard to the biological characterisation of the microorganism, MRSA is an extraordinarily flexible pathogen, able to cause infections in patients with known risk factors [10], but recently, it was isolated in the community worldwide, causing infections in healthy people with rapid and severe onset and was sometimes responsible for severe outcome. Community-associated methicillin-resistant S. aureus (CA-MRSA) are known to be genetically different from the nosocomial strains and to have enhanced virulence, due to a complex make-up of toxins and enzymes. CA-MRSA generally harbour small mobile chromosomal mec cassettes (SCCmec) types IV, V, VI or VII and several subtypes, especially type IV, that mediate methicillin resistance [11–13]. These cassettes, in these strains, are, in some cases associated with the Panton–Valentine leukocidin (PVL) and other virulence factors, usually not found in hospital-associated methicillin-resistant S. aureus (HA-MRSA) [14, 15].
In Europe and in Italy, in contrast to what has happened in the USA, where the diffusion of CA-MRSA is due to the almost exclusive spread of two major clones (ST1 USA400 and ST8 USA300), many different clones belonging to diverse sequence types (STs) have been isolated [13, 15–19]. This is true in many community infections but not in CF, in which many studies have failed to demonstrate an association between PVL and MRSA or, when found, the strains were not characterised [7, 20, 21]. A recent large cohort of Italian patients with CF and CA-MRSA were all found to be negative for the PVL gene [22].
Furthermore, less is known about the source of the MRSA clones infecting these patients who, due to their natural clinical history, are considered to be out-patients attending, during their lives, various specific centres or hospital wards. The lifestyle of these patients is surely a risk factor for the acquisition of MRSA and the paucity of papers dealing with this problem, which stimulated us to carry out this research.
The purpose of this 2-year prospective study was to determine the frequency with which MRSA was acquired in our CF population attending the University Hospital of Catania, Italy, as well as evaluating persistence and carrying out the molecular characterisation of the strains, including identifying their virulence content. MRSA were also evaluated for their resistance to antibiotics and their presence and persistence was correlated with lung function during the study period.
Materials and methods
Study design and staphylococcal isolation
In the period between February 2005 to October 2007, 64 patients attending our CF centre were screened during routine examinations. Respiratory cultures (217, collection was patient-dependent) were plated onto horse blood, colistin nalidixic acid, MacConkey, mannitol salt agar and Burkholderia cepacia selective plates (Oxoid, Basingstoke, UK). Our purpose was to study only the S. aureus isolated; however, all of the colonies were carefully examined for the eventual presence of small colony variants (SCVs) (none were found).
The FEV1 was registered for each patient.
Isolates were identified based on positive tube coagulase and API-Staph (bioMérieux, Marnes-la-Coquette, France), and a positive amplification of the 16S S. aureus rDNA (data not shown). The resistance to methicillin was confirmed by the presence of the mecA gene [23]. All patients positive for MRSA were longitudinally monitored and all MRSA serial isolates were included in the study.
Molecular characterisation of MRSA isolates
To determine if the 14 MRSA isolates were CA-MRSA and/or HA-MRSA associated clones, the following were carried out: genomic macro-restriction profiling using pulsed-field gel electrophoresis (PFGE) [24], multilocus sequence typing (MLST) as previously described [23], SCCmec typing by multiplex polymerase chain reaction (PCR) followed by different multiplex PCR protocols, focusing on the mec gene complex and the ccr gene complex [25–27].
Pathotype and biofilm determination
A complete pathotype including the capsular type, the membership to an agr group and the adhesin and toxin gene content was performed by using both conventional PCR and a new protocol, established in our laboratory, of multiplex PCR as previously described [13, 28].
Furthermore, due to the importance of biofilm production in CF patients, all strains were tested for their ability to produce biofilm by a spectrophotometrical quantitative assay. Each strain was grown in Tryptone Soy Broth (Oxoid, Basingstoke, UK), with the addition of 0.25% glucose (TSBG). These assays were performed in microtitre plates as previously described [29–32].
Antibiotic susceptibility testing and heteroresistance determination
Antibiotic susceptibility was determined for the following antibiotics: methicillin, vancomycin, teicoplanin, tobramycin, levofloxacin (Sigma Chemical Co., St. Louis, MO, USA), linezolid (Pfizer Inc., New York, NY, USA), tigecycline (Wyeth Pharmaceuticals, Collegeville, PA) and daptomycin (Novartis, Basel, Switzerland). Minimum inhibitory concentrations (MICs) were performed in cation-adjusted Mueller–Hinton broth following the >Clinical and Laboratory Standards Institute (CLSI) guidelines [33]. Heteroresistance was determined by the macro Etest (AB Biodisk, Solna, Sweden) and confirmed by population analysis profile (PAP) as previously described [34–36]. Briefly, colonies from cultures grown overnight on tryptic soy agar were inoculated into tryptic soy broth. After incubation for 24 h, dilutions of 10−3 (105 CFU/ml) and 10−6 (102 CFU/ml) were prepared in saline, and 50 μl were inoculated onto brain heart infusion agar plates containing 4.0, 6.0, 8.0, 12.0 and 16.0 mg of vancomycin/litre and 4.0, 8.0, 16.0 and 32.0 mg of teicoplanin/litre, respectively. The results were compared to the Mu3 (heteroresistant vancomycin-intermediate S. aureus [hVISA]) and Mu50 (VISA) standard strains, kindly provided by the Network on Antimicrobial Resistance in Staphylococcus aureus (NARSA, http://www.narsa.net/).
Results
During the study period, 5 out of the 64 patients were found to be infected only with MRSA (7.8%). In these five patients, co-colonisation with methicillin-sensitive S. aureus (MSSA) was observed in patients 3, 4 and 5, whereas no co-infection with Pseudomonas aeruginosa and/or B. cepacia was observed. Table 1 shows the age, the FEV1 index and the antibiotic therapy of the five patients who were positive for MRSA, and the main genetic and virulence characteristics of the 14 isolates. All strains were mecA-positive, with oxacillin MICs varying from 2–4 (considered to be low susceptible or resistant by the CLSI standards) to >256 mg/L and belonged to the agr type I. The isolates possessed the capsular antigen type 5 and showed different PFGE profiles when all patients were compared, but almost identical multiple isolates in the same patient. The comparison of the macrorestriction profiles with the STs showed that, in two cases (patients 1 and 2), the MRSA isolated were nosocomial clones circulating in Italy and in Europe, i.e. ST22 (EMRSA 15) and ST247, while the others (patients 4 and 5) corresponded to CA-MRSA isolates, belonging to different STs, i.e. ST8, 291 and 72; only in patient 3 (ST8) was it difficult to assign these isolates to HA-MRSA or CA-MRSA, only on the bases of their molecular features, considering this clone to be a bridge between hospital and community-associated strains. As previously observed in these patients, despite the use of the correct antibiotic courses, each clone tended to persist inside the lung, with diverse duration related to the reactivation of symptoms of each patient. The only exception was patient 5, in whom, after the initial isolation of a PVL-positive ST8-CA-MRSA IVa, identified as a USA300 clone variant (without the ACME genomic island), the strain was replaced by ST72 and these latter strains possessed an identical or closely related PFGE profile.
All strains were medium or strong biofilm producers (Table 1), and this result seemed to be consistent with the ability of these microorganisms to adhere to and persist in the lungs of these patients.
The presence of mecA and mecR/I was determined and, while all strains possessed the mecA gene, only seven contained ∆mecR (class B mec complex) and the same strains had an SCCmec cassette organised similarly to type IV (ST22), type IVc and IVa (ST8), all possessing recombinases ccrA2B2, while type I (ST247) showed recombinases ccrA1B1. In the other seven strains, it was impossible to define a structured SCCmec, at least by using the multiplex PCR protocols [25–27].
Further studies involving sequencing will be necessary to determine the hypothetical structure of these mec regions.
Concerning the analysis of virulence gene content, a core group of adhesins, i.e. icaA, clfA/B, fnbA, sdrE, spa and atl, were present in all strains. With regard to the toxin core genes, haemolysins (hl-s) and leukocidin E (lukE) were always present, while the group of accessory toxin genes, i.e. sea, sec, splB, tst and lukS/F-PVL, were present in various percentages inside the strains tested. Only patients 4 and 5 were infected by PVL-positive strains at the beginning, while in both patients, the serial isolates, although MRSA, were subsequently found to be different. With regard to other toxins, enterotoxin A (sea) was present in the isolates of patients 1 and 3, while leukocidin E (lukE) was distributed in all isolates, as stated before. MRSA strains isolated in patient 4, despite belonging to the same ST and PFGE types, showed subtle changes in their virulence gene content, having lost the lukS/F gene present in the first isolate, but continuing to contribute to the worsening lung function of the patient, even with the PVL-negative strains. Furthermore, the MRSA ST291 isolated in this patient lacked the association between splB and lukE, commonly localised on the pathogenic genomic island vSaβ [37]. A different situation was observed in patient 5, in whom after the first infection sustained by a variant of USA300 (ST8-IVa, ACME-negative) PVL and TSST-1 positive, four strains belonging to ST72 were found. These strains were PVL-negative, but one of them still maintained the toxic-shock syndrome toxin-1 (TSST-1). Generally speaking, among adhesion genes, cna was never detected in our strains, while among toxin genes, eta, sed and sej were never detected.
As shown in Table 1, the age of the five patients ranged from 7 to 24 years and in patients 1, 2 and 5, a history of worsening pulmonary obstruction, as demonstrated by a decrease in the FEV1 index, was found.
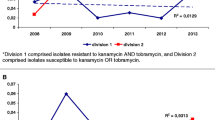
All MRSA strains were tested for their susceptibility to some anti Gram-positive antibiotics. As shown in Table 2, multiple isolates of the same patient maintained the same level of susceptibility. All strains were resistant to tobramycin, 10/14 were resistant to levofloxacin and all strains were susceptible to linezolid and tigecycline. Eight out of the 14 strains showed MICs ≥1 mg/L to vancomycin and two strains showed MICs of 1.5 mg/L to daptomycin. Macro Etest and PAP analysis were performed to look for the possible presence of subpopulations in the presence of high concentrations of vancomycin and, due to the importance of one dilution difference in the MIC for vancomycin, all isolates were included. Among the 14 strains, three isolates and their surviving replicates (see Table 2) showed heteroresistant subpopulations with both methods and in two strains with MICs of 2–4 mg/L, a quasi-VISA behaviour, i.e. similar to the MU50 strain, was found. It is interesting to note that, in these patients, the hVISA strains were CA-MRSA belonging to ST8. The two strains with daptomycin MICs of 1 mg/L were not hVISA.
Discussion
This study on MRSA in the CF patients attending the Catania CF centre allowed us to make the following observations. First, 7.8% of our CF population harboured MRSA; among these, we excluded the presence of SCVs due to the absence of typical phenotypic characteristics (small colony size, reduced growth rate and pigmentation, haemolysis-negative growth on MRSA and weak coagulase production).
This prevalence is in agreement with data obtained in a recent survey in Italy [22], but less than that reported in studies from other countries [38].
Of the 14 longitudinally isolated strains in these patients, all were shown to be agr type I and capsular type 5; four strains were HA-MRSA, eight were CA-MRSA, with only two of them carrying the PVL gene, and two strains (3A and 3B) showed characteristics halfway between the ancient HA-MRSA and the contemporary CA-MRSA. Persistence was observed in all patients, two of them chronically infected as defined by three or more cultures containing MRSA in the study period [7]. The homogeneous isolation of agr-I, cap5 strains in the CF patients demonstrated that they can colonise better the lung, surviving host defences due to the anti-phagocyte properties of capsular type 5 strains and their biofilm production. With regard to the pathogenicity of MRSA, the strains showed strong adhesion properties demonstrated by the constant presence of spa, clfA/B, atl and icaA. This characteristic makes these strains able to adhere to and invade host tissues where the sessile state is the best style in the lung of these patients.
Two patients were infected with two widespread HA-MRSA clones, i.e. ST22-HA-MRSA-IV and ST247-HA-MRSA-I, while in the other three patients, different CA-MRSA were detected. We are able to demonstrate in this paper the isolation of ST8, ST291 and ST72 variably associated with SCCmec DNA type IVa and IVc but also with not-typeable characteristics by using multiplex PCR protocols, as described. In these strains, recombination events probably took place and further studies will be necessary to characterise these mecDNA regions. A PVL-positive USA300 variant (ACME-negative) was found, for the first time, in our CF population, being already present, even if rarely, in our country [15]. Patients 4 and 5 were infected with PVL-positive strains at the beginning; interestingly in both cases, the second cultures were negative, while all other cultures were positive again with PVL-negative CA-MRSA. In patients 1, 2 and 5, there was an association between persistent virulent MRSA isolation and decreased lung functionality, as previously demonstrated [7, 39].
Some interesting comments can be made on these clones. ST247 is a well-known nosocomial MRSA clone with a worldwide distribution, while ST22, although nosocomially associated, is considered to be a bridge between the true nosocomial isolates and the community ones. With regard to the community-associated strains, two different groups of organisms were found. One is related to two different ST8 clones, in which only one was identified as a PVL-positive USA300 variant (ACME-negative), while the other, ST8-MRSA-IVc, was a PVL-negative strain.
The other group of CA-MRSA clones, i.e. ST291 and ST72, had different features in common: first, their community origin and second, the untypeability of the SCCmec DNA and a low-level resistance to oxacillin, despite the presence of the mecA gene. ST291 is a double-locus variant of ST398, a PVL-negative clone of swine origin, able to colonise or infect humans [40]. Human infections sustained by this clone have been documented, in particular, endocarditis, ventilator-associated pneumonia and wound infections [41]. Some of the ST398 human isolates harbour the PVL gene, thereby, illustrating the capacity of this clone to pick up additional virulence factors. One of our ST291 strains was PVL-positive, while the subsequent isolates were not. ST72 has been frequently isolated among methicillin-susceptible strains worldwide, and ST72-MRSA-IV has been documented as a coloniser or a community-associated strain in infected patients from Asia and South America [42, 43]. Our ST72 MRSA was untypeable and, due to its characteristics, could be considered as a precursor of the new CA-MRSA clones that are becoming more diffuse all around the world.
Regarding the antibiotic resistance characteristics of these 14 MRSA strains isolated in CF patients, together with the characteristic of resistance to the usual drugs, eight of these strains showed a reduced susceptibility to vancomycin. Furthermore, two strains showed a reduced susceptibility to daptomycin.
The presence of heteroresistance to vancomycin, described by other authors, was also demonstrated in our CF patients in both ST8 clones, possessing, in two cases, a quasi-VISA behaviour if compared with the standard strain MU50 [44].
As reported by many authors, heteroresistance can be associated with clinical vancomycin failure and this situation can be more severe in patients in whom the persistence of microorganisms in the lung is frequent [12, 45].
In conclusion, the present study demonstrates persisting infections with both HA-MRSA and CA-MRSA in our CF population, with an overall prevalence of 7.8%. The double colonisation by both hospital-associated and community-associated strains has already been observed, but these authors did not check for persistence and did not find any association with declining lung function [21]. We demonstrate that, in these patients, persistence was sustained by either identical clones that underwent subtle changes in their toxin content or by different clones over time. The isolation of MRSA in our CF population aged 7–24 years was associated with an increased severity of the disease even if, due to the small sample of patients included and the paucity of data on the clinical outcome, these results cannot be conclusive.
Furthermore, the presence of hVISA strains questions the use of glycopeptides in the treatment of MRSA infections in these patients.
References
Campana S, Taccetti G, Ravenni N, Masi I, Audino S, Sisi B, Repetto T, Döring G, de Martino M (2004) Molecular epidemiology of Pseudomonas aeruginosa, Burkholderia cepacia complex and methicillin-resistant Staphylococcus aureus in a cystic fibrosis center. J Cyst Fibros 3(3):159–163
Goodrich JS, Sutton-Shields TN, Kerr A, Wedd JP, Miller MB, Gilligan PH (2009) Prevalence of community-associated methicillin-resistant Staphylococcus aureus in patients with cystic fibrosis. J Clin Microbiol 47(4):1231–1233
Nadesalingam K, Conway SP, Denton M (2005) Risk factors for acquisition of methicillin-resistant Staphylococcus aureus (MRSA) by patients with cystic fibrosis. J Cyst Fibros 4(1):49–52
Boxerbaum B, Jacobs MR, Cechner RL (1988) Prevalence and significance of methicillin-resistant Staphylococcus aureus in patients with cystic fibrosis. Pediatr Pulmonol 4:159–163
Branger C, Fournier JM, Loulergue J, Bouvet A, Goullet P, Boutonnier A, de Gialluly C, Couetdic G, Chomarat M, Jaffar-Banjee MC, Mariani P (1994) Epidemiology of Staphylococcus aureus in patients with cystic fibrosis. Epidemiol Infect 112:489–500
Thomas SR, Gyi KM, Gaya H, Hodson ME (1998) Methicillin-resistant Staphylococcus aureus: impact at a national cystic fibrosis centre. J Hosp Infect 40:203–209
Dasenbrook EC, Merlo CA, Diener-West M, Lechtzin N, Boyle MP (2008) Persistent methicillin-resistant Staphylococcus aureus and rate of FEV1 decline in cystic fibrosis. Am J Respir Crit Care Med 178(8):814–821
Miall LS, McGinley NT, Brownlee KG, Conway SP (2001) Methicillin resistant Staphylococcus aureus (MRSA) infection in cystic fibrosis. Arch Dis Child 84(2):160–162
Ren CL, Morgan WJ, Konstan MW, Schechter MS, Wagener JS, Fisher KA, Regelmann WE; Investigators and Coordinators of the Epidemiologic Study of Cystic Fibrosis (2007) Presence of methicillin resistant Staphylococcus aureus in respiratory cultures from cystic fibrosis patients is associated with lower lung function. Pediatr Pulmonol 42(6):513–518
Boyce JM (1992) Methicillin-resistant Staphylococcus aureus in hospitals and long-term care facilities: microbiology, epidemiology, and preventive measures. Infect Control Hosp Epidemiol 13(12):725–737
Deurenberg RH, Stobberingh EE (2009) The molecular evolution of hospital- and community-associated methicillin-resistant Staphylococcus aureus. Curr Mol Med 9(2):100–115
Sakoulas G, Moise-Broder PA, Schentag J, Forrest A, Moellering RC Jr, Eliopoulos GM (2004) Relationship of MIC and bactericidal activity to efficacy of vancomycin for treatment of methicillin-resistant Staphylococcus aureus bacteremia. J Clin Microbiol 42(6):2398–2402
Stefani S, Bongiorno D, Cafiso V, Campanile F, Crapis M, Cristini F, Sartor A, Scarparo C, Spina D, Viale P (2009) Pathotype and susceptibility profile of a community-acquired methicillin-resistant Staphylococcus aureus strain responsible for a case of severe pneumonia. Diagn Microbiol Infect Dis 63(1):100–104
Higuchi W, Takano T, Teng LJ, Yamamoto T (2008) Structure and specific detection of staphylococcal cassette chromosome mec type VII. Biochem Biophys Res Commun 377:752–756
Stefani S, Monaco M, Campanile F, Cafiso V, Sanchini A, Marone P, Pantosti A (2009) Characterisation of Panton–Valentine leukocidine positive methicillin-resistant Staphylococcus aureus in Italy. In: Proceedings of the 19th European Congress of Clinical Microbiology and Infectious Diseases (ECCMID), Helsinki, Finland, May 2009, abstract number P1573
Denis O, Deplano A, De Beenhouwer H, Hallin M, Huysmans G, Garrino MG, Glupczynski Y, Malaviolle X, Vergison A, Struelens MJ (2005) Polyclonal emergence and importation of community-acquired methicillin-resistant Staphylococcus aureus strains harbouring Panton–Valentine leucocidin genes in Belgium. J Antimicrob Chemother 56(6):1103–1106
Otter JA, French GL (2008) The emergence of community-associated methicillin-resistant Staphylococcus aureus at a London teaching hospital, 2000–2006. Clin Microbiol Infect 14(7):670–676
Tristan A, Bes M, Meugnier H, Lina G, Bozdogan B, Courvalin P, Reverdy ME, Enright MC, Vandenesch F, Etienne J (2007) Global distribution of Panton–Valentine leukocidin-positive methicillin-resistant Staphylococcus aureus, 2006. Emerg Infect Dis 13(4):594–600
Valentini P, Parisi G, Monaco M, Crea F, Spanu T, Ranno O, Tronci M, Pantosti A (2008) An uncommon presentation for a severe invasive infection due to methicillin-resistant Staphylococcus aureus clone USA300 in Italy: a case report. Ann Clin Microbiol Antimicrob 7:11
Boyle MP, Ross T, Goldberg JD, Podliska MZ, Cai M, Mogayzel PJ, Carroll KC (2005) Molecular epidemiology of MRSA infection in cystic fibrosis and its clinical implications. Pediatr Pulmonol 28:288–289
Glikman D, Siegel JD, David MZ, Okoro NM, Boyle-Vavra S, Dowell ML, Daum RS (2008) Complex molecular epidemiology of methicillin-resistant Staphylococcus aureus isolates from children with cystic fibrosis in the era of epidemic community-associated methicillin-resistant S. aureus. Chest 133(6):1381–1387
Campana S, Cocchi P, Döring G, Taccetti G, Moroney SM (2007) Emergence of an epidemic clone of community-associated methicillin-resistant Panton–Valentine leucocidin-negative Staphylococcus aureus in cystic fibrosis patient populations. J Clin Microbiol 45(9):3146
Campanile F, Bongiorno D, Borbone S, Venditti M, Giannella M, Franchi C, Stefani S (2007) Characterization of a variant of the SCCmec element in a bloodstream isolate of Staphylococcus intermedius. Microb Drug Resist 13(1):7–10
Mato R, Campanile F, Stefani S, Crisóstomo MI, Santagati M, Sanches SI, de Lencastre H (2004) Clonal types and multidrug resistance patterns of methicillin-resistant Staphylococcus aureus (MRSA) recovered in Italy during the 1990s. Microb Drug Resist 10(2):106–113
Kondo Y, Ito T, Ma XX, Watanabe S, Kreiswirth BN, Etienne J, Hiramatsu K (2007) Combination of multiplex PCRs for staphylococcal cassette chromosome mec type assignment: rapid identification system for mec, ccr, and major differences in junkyard regions. Antimicrob Agents Chemother 51(1):264–274
Milheiriço C, Oliveira DC, de Lencastre H (2007) Multiplex PCR strategy for subtyping the staphylococcal cassette chromosome mec type IV in methicillin-resistant Staphylococcus aureus: ‘SCCmec IV multiplex’. J Antimicrob Chemother 60(1):42–48
Oliveira DC, de Lencastre H (2002) Multiplex PCR strategy for rapid identification of structural types and variants of the mec element in methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother 46(7):2155–2161
Lina G, Boutite F, Tristan A, Bes M, Etienne J, Vandenesch F (2003) Bacterial competition for human nasal cavity colonization: role of Staphylococcal agr alleles. Appl Environ Microbiol 69(1):18–23
Cafiso V, Bertuccio T, Santagati M, Campanile F, Amicosante G, Perilli MG, Selan L, Artini M, Nicoletti G, Stefani S (2004) Presence of the ica operon in clinical isolates of Staphylococcus epidermidis and its role in biofilm production. Clin Microbiol Infect 10:1081–1088
Cafiso V, Bertuccio T, Santagati M, Demelio V, Spina D, Nicoletti G, Stefani S (2007) agr-Genotyping and transcriptional analysis of biofilm-producing Staphylococcus aureus. FEMS Immunol Med Microbiol 51(1):220–227
Christensen GD, Simpson WA, Younger JJ, Baddour LM, Barrett FF, Melton DM, Beachey EH (1985) Adherence of coagulase-negative staphylococci to plastic tissue culture plates: a quantitative model for the adherence of staphylococci to medical devices. J Clin Microbiol 22:996–1006
Ziebuhr W, Krimmer V, Rachid S, Lössner I, Götz F, Hacker J (1999) A novel mechanism of phase variation of virulence in Staphylococcus epidermidis: evidence for control of the polysaccharide intercellular adhesin synthesis by alternating insertion and excision of the insertion sequence element IS256. Mol Microbiol 32:345–356
Clinical and Laboratory Standards Institute (CLSI) (2009) Performance standards for antimicrobial susceptibility testing. CLSI M100 and S19 vol. 29, no. 3. CLSI, Wayne, PA, USA
Borbone S, Campanile F, Bongiorno D, Perez M, Stefani S (2009) Heteroresistance to glycopeptides in Italian methicillin-resistant Staphylococcus aureus isolates. In: Proceedings of the 49th Interscience Conference on Antimicrobial Agents and Chemotherapy (ICCAC), San Francisco, CA, September 2009, C2-114
Cassone M, Campanile F, Pantosti A, Venditti M, Stefani S (2004) Identification of a variant “Rome clone” of methicillin-resistant Staphylococcus aureus with decreased susceptibility to vancomycin, responsible for an outbreak in an intensive care unit. Microb Drug Resist 10(1):43–49
Campanile F, Bongiorno D, Borbone S, Falcone M, Giannella M, Venditti M, Stefani S (2008) In vitro activity of daptomycin against methicillin- and multi-resistant Staphylococcus haemolyticus invasive isolates carrying different mec complexes. Diagn Microbiol Infect Dis 61(2):227–231
Baba T, Takeuchi F, Kuroda M, Yuzawa H, Aoki K, Oguchi A, Nagai Y, Iwama N, Asano K, Naimi T, Kuroda H, Cui L, Yamamoto K, Hiramatsu K (2002) Genome and virulence determinants of high virulence community-acquired MRSA. Lancet 359(9320):1819–1827
Cystic Fibrosis Foundation (CFF) (2007) Patient registry: annual data report 2006. CFF, Bethesda, MD, USA
Elizur A, Orscheln RC, Ferkol TW, Atkinson JJ, Dunne WM Jr, Buller RS, Armstrong JR, Mardis ER, Storch GA, Cannon CL (2007) Panton–Valentine leukocidin-positive methicillin-resistant Staphylococcus aureus lung infection in patients with cystic fibrosis. Chest 131(6):1718–1725
Wulf M, Voss A (2008) MRSA in livestock animals—an epidemic waiting to happen? Clin Microbiol Infect 14(6):519–521
Witte W, Strommenger B, Stanek C, Cuny C (2007) Methicillin-resistant Staphylococcus aureus ST398 in humans and animals, Central Europe. Emerg Infect Dis 13(2):255–258
Park C, Shin HH, Kwon EY, Choi SM, Kim SH, Park SH, Choi JH, Yoo JH, Lee DG, Shin WS (2009) Two variants of staphylococcal cassette chromosome mec type IVA in community-associated meticillin-resistant Staphylococcus aureus strains in South Korea. J Med Microbiol 58(Pt 10):1314–1321
Schuenck RP, Nouér SA, Winter Cde O, Cavalcante FS, Scotti TD, Ferreira AL, Giambiagi-de Marval M, dos Santos KR (2009) Polyclonal presence of non-multiresistant methicillin-resistant Staphylococcus aureus isolates carrying SCCmec IV in health care-associated infections in a hospital in Rio de Janeiro, Brazil. Diagn Microbiol Infect Dis 64(4):434–441
Denis O, Nonhoff C, Byl B, Knoop C, Bobin-Dubreux S, Struelens MJ (2002) Emergence of vancomycin-intermediate Staphylococcus aureus in a Belgian hospital: microbiological and clinical features. J Antimicrob Chemother 50(3):383–391
Soriano A, Marco F, Martínez JA, Pisos E, Almela M, Dimova VP, Alamo D, Ortega M, Lopez J, Mensa J (2008) Influence of vancomycin minimum inhibitory concentration on the treatment of methicillin-resistant Staphylococcus aureus bacteremia. Clin Infect Dis 46(2):193–200
Acknowledgement
We gratefully acknowledge the Network on Antimicrobial Resistance in Staphylococcus aureus (NARSA) for providing the Mu3 (NRS2) and Mu50 (NRS1) control strains and Antony Bridgewood for the language revision of the manuscript. Partial support for this study was provided by grants from the Italian Minister of Health and from MIUR-Cofin 2007, 2007SCA9RK.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cafiso, V., Bertuccio, T., Spina, D. et al. Methicillin resistance and vancomycin heteroresistance in Staphylococcus aureus in cystic fibrosis patients. Eur J Clin Microbiol Infect Dis 29, 1277–1285 (2010). https://doi.org/10.1007/s10096-010-1000-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-010-1000-5