Abstract
The association between helminth infections and childhood atopic diseases remains controversial. The majority of studies have been carried out in tropical areas, whereas less information is available from western countries with low intensity of helminth infections. In the Netherlands, the infection of pigs with Ascaris suum is very common, particularly on pig farms with outdoor facilities. This helminth can also infect humans, causing visceral larva migrans. This study aims at determining the prevalence of antibodies against A. suum and its association with allergic symptoms and sensitisation in a population of 4-year-old children living in the Netherlands. Blood samples from 629 children from the prospective birth cohort Prevention and Incidence of Asthma and Mite Allergy (PIAMA) study were examined for Ascaris antibodies. Data on allergic symptoms and sensitisation were collected using questionnaires and radioallergosorbent tests (RAST). A total of 45 out of 629 (7%) were found to be Ascaris-seropositive. In addition, a positive association between Ascaris seropositivity and wheeze in the last year, doctor-diagnosed asthma and food and aero-allergen sensitisation was found. These results support the hypothesis that low-level or transient infection with helminths enhances allergic reactivity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Infection with helminths and their effect on atopic diseases has been discussed for several years [1]. The results so far, however, are controversial, with several factors being suggested to influence whether infection protects or enhances allergic manifestations [2].
In this study, we focus on Ascaris suum, a roundworm of pigs that can also infect humans worldwide. A recent survey in the Netherlands showed that the infection of pigs with A. suum is very common, particularly on pig farms with outdoor facilities [3]. Transmission of this parasite to humans takes place after ingestion of the infective eggs present in soil contaminated with the faeces of infected pigs. After ingestion, the eggs hatch and the larvae penetrate the intestinal wall and migrate to different organs, including the lungs. Humans are accidental hosts for this helminth and, generally, the migrating larvae do not mature to the adult stage, but it induces an inflammatory response. Although generally attributed to Toxocara canis, the migration of A. suum larvae can also result in visceral larva migrans (VLM) characterised by several clinical signs, including wheezing, coughing and shortness of breath [4]. In Denmark, Nejsum et al. have shown by molecular typing, that A. suum is a zoonosis in this country [5]. These authors suggest that the main transmission route for human ascariasis in developed countries appears to be from pigs to people.
Infection with certain helminth species have been suggested to protect against allergic disease. Evidence from experimental studies indicates that these helminths induce a regulatory network that down-modulates not only parasite-induced inflammation, but also other immunopathologies, such as atopic and autoimmune diseases [6]. Several epidemiological studies, however, have shown a positive association between Ascaris infections and the severity of atopic diseases [7, 8]. For these reasons, we were interested in investigating the prevalence of antibodies against A. suum and its possible associations with allergic manifestations in children in the Netherlands.
Materials and methods
Study population and study design
The Prevention and Incidence of Asthma and Mite Allergy (PIAMA) study is a prospective birth cohort study with an initial enrollment of 4,146 pregnant women [9, 10]. The cohort was recruited in 1996–1997 during the second trimester of pregnancy from a series of communities varying from rural villages to large cities in the north, west and centre of the Netherlands. Mothers were classified as allergic or non-allergic on the basis of a validated screening questionnaire [11]. Non-allergic (based on a screening questionnaire) pregnant women were invited to participate in a ‘natural history’ study arm. Pregnant women identified as allergic through a screening questionnaire were allocated to a placebo-controlled intervention arm (initial enrollment of 855), with a random subset of 472 allocated to the natural history arm. The total initial number of participants in the natural history arm was 3,291. The intervention involved the use of mite-impermeable mattress and pillow covers. The study protocol was approved by the Institutional Review Boards of each participating institute, and written informed consent was obtained from all of the participants.
Health outcomes
At 4 years follow up of the birth cohort, a questionnaire based on the ISAAC core questions on the symptoms of asthma, allergic rhinitis and atopic eczema was sent to the participating families. The main outcomes of interest derived from this questionnaire were the prevalence of wheeze, doctor-diagnosed asthma, itchy rash present in the folds of elbows, the back of the knees, the front of the ankles, in the neck or around the eyes or ears, eczema and nasal symptoms with itchy and watery eyes.
During medical examination at age 4 years, venous blood samples were drawn in a sub-cohort (n = 629) of the children [9]. Of these 629 children, 272 were from the intervention arm and 357 were from the natural history arm. Serum samples were used to determine the total and allergen-specific IgE. A high total IgE level was specified as a level equal to or higher than 100 IU/ml. Children were considered as sensitised against inhalant allergens if one or more allergen-specific IgE levels (to house dust mite, cat, dog, birch, Dactylis glomerata [Cocksfoot] and Alternaria alternata) were equal to or higher than 0.35 IU/ml. Sensitisation to food allergens was defined as a high level of allergen-specific IgE to milk or egg (also ≥0.35 IU/ml).
Preparation of Ascaris suum excretory–secretory antigen
The excretory–secretory (E/S) antigen derived from L2 A. suum larvae was prepared using a modified procedure previously described by Savigny [12]. A. suum adult worms were collected from the faeces of naturally infected pigs. Eggs were collected from the uteri of female worms and were allowed to embryonate in 0.1 M H2SO4 in the dark at room temperature for 4–6 weeks. Embryonated eggs were washed with phosphate-buffered saline (PBS, pH 7.2) and incubated in 0.5% sodium hypochlorite for 20 min to soften the egg shells. Following extensive washing with PBS, the eggs were suspended in 5 ml of Modified Eagle Medium (Gibco, NY, USA) and the larvae were freed from the shells after careful homogenisation. Living larvae were separated from egg’ shells and other debris by allowing the larvae to migrate through cotton wool contained in tubes filled with medium at 37°C overnight. The migrating larvae were collected and counted. A suspension of 150 larvae per ml of medium was incubated at 37°C for 6 days, after which the medium was harvested and used as the E/S antigen. The E/S antigen was dialysed and concentrated using a 10-kDa cut-off Amicon Ultra-15 filter (Millipore) by centrifugation for 15 min at 3,550 × g against PBS. The protein concentration was determined by the Micro BCA Protein Assay kit (Pierce Biotechnology). The A. suum E/S antigen was analysed using sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE). For this purpose, the E/S antigen was solubilised under reducing conditions and electrophorised on 8% polyacrylamide gel according to Laemmli [13]. The protein banding pattern was revealed using silver staining (Bio-Rad Laboratories, Hercules, CA, USA)
Determination of phosphorylcholine in the Ascaris suum E/S antigen
Phosphorylcholine is a structural component of a variety of prokaryotic and eukaryotic pathogens and is, in part, responsible for cross-reactivity in the immunodiagnosis of various helminth infections [14]. In order to determine whether the A. suum E/S antigen used in this study contained phosphorylcholine, an enzyme-linked immunosorbent assay (ELISA) was performed. Briefly, a standard calibration curve was made by two-fold serial dilutions of phosphorylcholine-conjugated BSA (PC-BSA) (Biosearch Technologies, Inc., Novato, CA) in carbonate buffer (0.1 mol/l Na2CO3 pH 9.6) starting at 0.5 μg/ml. Microtitre ELISA plates (Nunc, Frickenhausen, Germany) were coated with either PC-BSA or E/S antigen (10 μg/mL), diluted in carbonate buffer and incubated overnight at 37°C. Washes with PBS, 0.05% Tween-20 were performed between every step. Mouse IgA anti-phosphorylcholine (Sigma, USA) diluted in 2% BSA, PBS and 0.05% Tween-20 was added and incubated at 37°C for 1 h. Peroxidase-conjugated goat anti-mouse IgA (Sigma, USA) was then added and incubated for 1 h at 37°C. The substrate H2O2, 0.05% and 5-ASA (5-amino-2-hydroxybenzoic acid) was added and, after 1 h at 22°C, the absorbance was read at 450 nm. Crude antigen of Trichinella spiralis larvae with high content of phosphorylcholine was also included in this assay as a positive control. The lowest detection limit of the assay is 0.0125 μg/ml.
Determination of tropomyosin in the Ascaris suum E/S antigen
Tropomyosin is a highly conserved protein and has been shown to be a pan-allergen in invertebrates, such as shrimps and other crustaceans, molluscs, mites and cockroaches [15]. In addition, tropomyosin has been found in Anisakis simplex [16] and recently in Ascaris lumbricoides [17]. In order to determine whether tropomyosin is present in the E/S antigen of A. suum used in this study, a previously described chimeric ELISA was used [17]. Briefly, microtitre plates were coated with 1 μg/well of anti-tropomyosin (mAb 1A6) overnight at 4°C, in carbonate–bicarbonate buffer pH = 9.6. After washing, plates were incubated either with affinity-purified tropomyosin from A. lumbricoides at 0.5 μg/mL or A. suum E/S antigen at 10 μg/mL. As the detector antibody, serum at 1:10 dilution from a shrimp-allergic patient with strong reactivity to shrimp tropomyosin and which is highly cross-reactive with A. lumbricoides tropomyosin was used. After washing, incubation with 125I-labelled anti-human IgE was performed. Quantification was performed using a chimeric mouse Fab/human Fc epsilon antibody (clone 2B12-IgE) [17].
Ascaris IgG ELISA
The detection of Ascaris IgG antibodies was performed using an ELISA and E/S antigen derived from A. suum larvae [18, 19]. High-binding ELISA microtitre plates (Greiner Bio-One, Frickenhausen, Germany) were coated with E/S antigen (10 μg/mL) diluted in 0.1 M sodium carbonate (Na2CO3) pH 9.6. The plates were incubated overnight (without lids) at 37°C to allow the E/S antigen to dry onto the wells. They were washed three times with PBS (pH 7.2) containing 0.05% v/v Tween-20 (PBS/Tween) between every step. A blocking step was performed by adding to every well 2% bovine serum albumin (BSA) (Boehringer Mannheim, GmbH, Mannheim, Germany) solution in PBS/Tween and incubated for 30 min at 37°C. Serum samples were diluted 1:40 in 2% BSA/PBS/Tween and added to the plates for 1 h at 37°C. Anti-human IgG conjugated to alkaline phosphatase (Dako, Glostrup, Denmark) diluted in 4% BSA/PBS/Tween was added for 1 h at 37°C. The substrate H2O2, 0.05% and 5-ASA was added and, after 1 h at 22°C, the absorbance was read at 450 nm. The extinction value of the tested serum and of the cut-off serum was used to calculate their ratio. A ratio higher or equal to 1.0 was considered to be positive. The cut-off value was defined as the mean absorbance of 20 serum samples from healthy donors plus three times the standard deviation.
The specificity of the Ascaris ELISA used in this study was found to be 90% when the sera from patients with other infections endemic in the Netherlands were tested: Toxocara sp. (n = 10), Toxoplasma gondii (n = 10), Borrelia sp. (n = 10), Treponema pallidum (n = 10) and Bordetella pertusis (100%). Using serum samples from patients with other parasitic infections that are not endemic in the Netherlands: Taenia solium (n = 14), Trichinella sp. (n = 10), Echinococcus granulosus (n = 10), Leishmania sp. (n = 10) and Entamoeba histolytica (n = 10), a specificity of 76% was found. It is important to bear in mind that, for these patients, concomitant Ascaris infections cannot be excluded. The sensitivity of this ELISA was not determined, since serum samples from parasitologically confirmed patients were not available.
Statistical analyses
The associations between Ascaris seropositivity and respiratory and allergic outcomes, total IgE and sensitisation to aero- and food allergens were assessed using logistic regression analysis. Crude odds ratios (ORs) were estimated, as well as ORs adjusted for gender, education of the mother, parental atopy, the presence of older siblings, study arm (intervention or natural history), birth weight, parental smoking, the presence of pets, breast feeding and region (north, central and south areas of the country). All analyses were carried out using SAS for Windows version 8.2 (SAS Institute, Cary, NC, USA).
Results
Prevalence of antibodies against Ascaris suum and its association with allergic symptoms and sensitisation
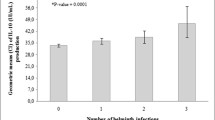
A total of 45 out of 629 (7%) 4-year-old children were found to be positive in the Ascaris IgG ELISA (Fig. 1). Table 1 shows the associations between positive Ascaris IgG ELISA results (ratio ≥1.0) and allergic symptoms and sensitisation. Significant positive associations with wheeze in the last year, doctor-diagnosed asthma and food allergen sensitisation was found. Adjusted ORs and 95% confidence intervals (CI) were for wheeze 2.24 (1.03–4.90), asthma 3.96 (1.53–10.29) and food allergen sensitisation 2.95 (1.47–5.89). Associations with eczema, total IgE (≥100 IU/ml) and aero-allergen sensitisation were positive but not significant. There was no association with itchy rash or nasal/eye symptoms.
Ratio values from the Ascaris IgG ELISA using serum samples of 4-year-old children from the birth cohort PIAMA study. Ratios were calculated by dividing the OD values of the tested serum by the OD of the cut-off serum (0.209). The average OD ± SD of the sera from healthy individuals to define the cut-off value was 0.08 ± 0.043. A ratio higher or equal to 1.0 was considered to be positive
When the analysis was performed using clearly seropositive results (ratio ≥1.1), the positive association with wheeze in the last year and doctor-diagnosed asthma was stronger, and a positive association with aero-allergen sensitisation emerged: adjusted OR for wheeze 2.98 (1.11–8.06), asthma 5.62 (1.78–17.72) and aero-allergen sensitisation 3.90 (1.50–10.16). Association with food allergen sensitisation was positive but not significant (Table 2).
Characterisation of Ascaris suum E/S antigen
In order to characterise the A. suum E/S antigen used in this study, both the phosphorylcholine and tropomyosin content were determined. The results indicate that the phosphorylcholine content in the A. suum E/S was below the detection limit of the assay (<0.0125 μg/ml) compared to 5 μg/ml in the T. spiralis crude larval antigen used as the positive control. The tropomyosin content of the A. suum E/S antigen was also lower than the detection limit of the assay (<30 ng/ml) compared to a 220 ng/ml content of a purified tropomyosin derived from A. lumbricoides.
Figure 2 shows the SDS-PAGE analysis of the A. suum E/S antigen. An 8% SDS-PAGE reveals that the products released by the A. suum L2 larvae range in apparent molecular weight from 20 to 250 kDa.
Discussion
The aim of the present study was to determine the Ascaris seroprevalence among 4-year-old children from the prospective birth cohort PIAMA study carried out in the Netherlands. In addition, we were interested in investigating whether any association exists between Ascaris seropositivity and allergic manifestations.
Although A. lumbricoides is not endemic in the Netherlands, a recent survey has shown that the infection of pigs with A. suum is very common in this country, particularly in animals with outdoor facilities [3]. The eggs of A. suum have been reported in sewage sludge which has been widely used as a fertiliser on agricultural grounds and public parks [19]. Exposure to A. suum could, therefore, affect not only persons working on pig farms but also those living in other areas.
The results from this study indicate an Ascaris seroprevalence of 7% and a positive association between seropositivity and allergic symptoms and sensitisation. Other studies carried out in countries with low intensity of helminth infections include that of Dold et al. in Germany [7]. These authors found, in a cohort of school children, that Ascaris sensitisation was positively associated with sensitisation to inhalant allergens and they support the hypothesis that low-level contact with helminths enhances allergic reactivity. Recently, Hunninghake et al. examined the relationship between sensitisation to A. lumbricoides and measures of asthma morbidity and severity in a Costa Rican population [8]. The authors conclude that Ascaris sensitisation may be an important marker of severe atopy and disease morbidity in children with asthma in areas with a low prevalence of helminthiasis.
A systematic literature review and meta-analysis carried out by Leonardi-Bee et al. [20] indicates that A. lumbricoides was associated with significantly increased odds of asthma. These authors come to the conclusion that not all parasite infections protect against asthma.
Infection with other helminths has also been reported to be positively associated with allergic manifestations. Desowitz et al. described in 1981 the prevalence of antibodies to T. canis and Dirofilaria immitis in asthmatic and non-asthmatic children born and raised in Hawaii. They found a significantly higher prevalence of parasite-specific IgE antibodies in the asthma patients than in the non-asthmatic population [21]. In the Netherlands, Buijs et al. carried out cross-sectional studies among elementary school children, concluding that allergic manifestations occur more often in Toxocara-seropositive children [22]. In a study on Toxocara seroprevalence and childhood asthma carried out in Malaysia, the authors report that children with asthma had a higher Toxocara seropositivity than the non-asthmatic controls [23]. Using murine models, we have recently shown that the infection of mice with T. canis leads to the exacerbation of experimental allergic airway inflammation [24]. The mechanism underlining this positive association is not fully understood; however, the type of immune response induced in addition to the tissue damage caused by the migrating larvae may contribute to the enhancement of allergic manifestations. Furthermore, a parasite which is not well adapted to the human host (e.g. A. suum, Toxocara sp.) may be causing more damage and, therefore, promoting allergic reactivity compared to a parasite which has evolved to infect humans.
Interestingly, infection with Ascaris sp. has also been reported to be negatively associated with allergic manifestations. Cooper et al. conducted a cross-sectional study among school-aged children in Pichincha, Ecuador. The authors investigated the effect of geo-helminth infections on atopy and found that infections with A. lumbricoides or Ancylostoma duodenale were associated with significant protective effects against allergen skin test reactivity among school-aged children living in an endemic region of the rural tropics [25, 26].
A negative association between allergic manifestation and infection with other helminths such as schistosomes in tropical areas have also been reported [27]. This protective effect, however, have been shown to depend on the intensity and chronicity of infection [28]. In chronic helminth infection, the suppression of allergies has been suggested to be mediated by the induction of a T-cell hypo-responsiveness state that includes T-cell anergy, increased frequency of regulatory T cells and elevated production of IL-10 and transforming growth factor-β (TGF-β) [1]. Failure in inducing this type of response may explain the lack of protection against allergy by certain helminth species.
A possible explanation for how a parasite like Ascaris sp. could have both a protective and enhancing effect on allergic manifestations may depend also on the intensity of infection and whether it is an acute or chronic infection. Other factors that may influence the association between worm infections and allergies are the parasite species involved, infection of a definitive vs. accidental host, timing and the frequency of exposure.
The results from this study show a positive association between Ascaris ELISA results and wheeze in the last year, doctor-diagnosed asthma, in addition to food sensitisation. When Ascaris ELISA results with higher ratios (≥1.1) were analysed, the association with wheeze in the last year and doctor-diagnosed asthma was stronger, and a positive association with aero-allergen sensitisation emerged, whereas food allergen sensitisation was weaker. Several factors may influence these findings, including the inoculum size. We have previously reported that mice infected with either a high or a low T. canis inoculum size showed, in a dose-dependent manner, increased levels of parasite-specific antibodies [29]. Whether various inoculum sizes of A. suum may influence the development of different types of allergic manifestations is an interesting question that remains to be addressed.
In the present study, an IgG ELISA using E/S antigen derived from A. suum was used. The use of secreted products from roundworms have been reported to increase the specificity of the assays used for the immunodiagnosis of VLM due to their lower content of cross-reactive molecules as compared to crude larval or adult antigen. Our results confirm this observation, since cross-reactive molecules such as phosphorylcholine and tropomyosin that are usually found in somatic helminth antigens were not detectable in the A. suum E/S antigen. The products released by the A. suum L2 larvae used in this study were shown to contain different molecular weight proteins, as described in early studies by Kennedy and Qureshi [30] on the characterisation of this helminth antigens. Toxocara sp., the roundworm of dogs and cats which have been reported to cross-react in the A. suum ELISA [31], is endemic in the Netherlands. Double infection with Ascaris sp. and Toxocara sp. could not be excluded [19]; however, all of the serum samples used in this study with positive Ascaris ELISA results were found to be negative in the Toxocara ELISA and, the other way round, the Toxocara-positive serum samples were negative in the Ascaris ELISA (data not shown). These findings indicate that the Ascaris seropositivity found is not influenced by concomitant Toxocara infections or by the presence of cross-reactive molecules such as phosphorylcholine or pan-allergens such as tropomyosin.
In conclusion, we found a positive association between Ascaris seropositivity and allergic symptoms and sensitisation in a population of 4-year-old children in the Netherlands. The results from this study suggest that zoonotic tissue-migrating helminths may contribute to the development of allergic manifestations, particularly in countries with a low prevalence of helminth infections.
References
Fallon PG, Mangan NE (2007) Suppression of TH2-type allergic reactions by helminth infection. Nat Rev Immunol 7:220–230
Cooper PJ (2009) Interactions between helminth parasites and allergy. Curr Opin Allergy Clin Immunol 9:29–37
Eijck IA, Borgsteede FH (2005) A survey of gastrointestinal pig parasites on free-range, organic and conventional pig farms in the Netherlands. Vet Res Commun 29:407–414
Crompton DW (2001) Ascaris and ascariasis. Adv Parasitol 48:285–375
Nejsum P, Parker ED Jr, Frydenberg J, Roepstorff A, Boes J, Haque R, Astrup I, Prag J, Skov Sørensen UB (2005) Ascariasis is a zoonosis in Denmark. J Clin Microbiol 43:1142–1148
Maizels RM, Yazdanbakhsh M (2008) T-cell regulation in helminth parasite infections: implications for inflammatory diseases. Chem Immunol Allergy 94:112–123
Dold S, Heinrich J, Wichmann HE, Wjst M (1998) Ascaris-specific IgE and allergic sensitization in a cohort of school children in the former East Germany. J Allergy Clin Immunol 102:414–420
Hunninghake GM, Soto-Quiros ME, Avila L, Ly NP, Liang C, Sylvia JS, Klanderman BJ, Silverman EK, Celedón JC (2007) Sensitization to Ascaris lumbricoides and severity of childhood asthma in Costa Rica. J Allergy Clin Immunol 119:654–661
Brunekreef B, Smit J, de Jongste J, Neijens H, Gerritsen J, Postma D, Aalberse R, Koopman L, Kerkhof M, Wilga A, van Strien R (2002) The prevention and incidence of asthma and mite allergy (PIAMA) birth cohort study: design and first results. Pediatr Allergy Immunol 13(Suppl 15):55–60
Koopman LP, Smit HA, Heijnen ML, Wijga A, van Strien RT, Kerkhof M, Gerritsen J, Brunekreef B, de Jongste JC, Neijens HJ (2001) Respiratory infections in infants: interaction of parental allergy, child care, and siblings—The PIAMA study. Pediatrics 108:943–948
Lakwijk N, van Strien RT, Doekes G, Brunekreef B, Gerritsen J (1998) Validation of a screening questionnaire for atopy with serum IgE tests in a population of pregnant Dutch women. Clin Exp Allergy 28:454–458
Savigny DH (1975) In vitro maintenance of Toxocara canis larvae and a simple method for the production of Toxocara ES antigen for use in serodiagnostic tests for visceral larva migrans. J Parasitol 61:781–782
Laemmli UK (1970) Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature 227:680–685
Lal RB, Ottesen EA (1988) Enhanced diagnostic specificity in human filariasis by IgG4 antibody assessment. J Infect Dis 158:1034–1037
Reese G, Ayuso R, Lehrer SB (1999) Tropomyosin: an invertebrate pan-allergen. Int Arch Allergy Immunol 119:247–258
Asturias JA, Eraso E, Martínez A (2000) Cloning and high level expression in Escherichia coli of an Anisakis simplex tropomyosin isoform. Mol Biochem Parasitol 108:263–267
Santos AB, Rocha GM, Oliver C, Ferriani VP, Lima RC, Palma MS, Sales VS, Aalberse RC, Chapman MD, Arruda LK (2008) Cross-reactive IgE antibody responses to tropomyosins from Ascaris lumbricoides and cockroach. J Allergy Clin Immunol 121:1040–1046
Nakamura-Uchiyama F, Tokunaga Y, Suzuki A, Akao N, Hiromatsu K, Hitomi S, Nawa Y (2006) A case of Ascaris suum visceral larva migrans diagnosed by using A. suum larval excretory–secretory (ES) antigen. Scand J Infect Dis 38:221–224
van Knapen F, Buijs J, Kortbeek LM, Ljungström I (1992) Larva migrans syndrome: toxocara, ascaris, or both? Lancet 340:550–551
Leonardi-Bee J, Pritchard D, Britton J (2006) Asthma and current intestinal parasite infection: systematic review and meta-analysis. Am J Respir Crit Care Med 174:514–523
Desowitz RS, Rudoy R, Barnwell JW (1981) Antibodies to canine helminth parasites in asthmatic and nonasthmatic children. Int Arch Allergy Appl Immunol 65:361–366
Buijs J, Borsboom G, Renting M, Hilgersom WJ, van Wieringen JC, Jansen G, Neijens J (1997) Relationship between allergic manifestations and Toxocara seropositivity: a cross-sectional study among elementary school children. Eur Respir J 10:1467–75
Chan PW, Anuar AK, Fong MY, Debruyne JA, Ibrahim J (2001) Toxocara seroprevalence and childhood asthma among Malaysian children. Pediatr Int 43:350–353
Pinelli E, Brandes S, Dormans J, Gremmer E, van Loveren H (2008) Infection with the roundworm Toxocara canis leads to exacerbation of experimental allergic airway inflammation. Clin Exp Allergy 38:649–658
Cooper PJ, Chico ME, Rodrigues LC, Ordonez M, Strachan D, Griffin GE, Nutman TB (2003) Reduced risk of atopy among school-age children infected with geohelminth parasites in a rural area of the tropics. J Allergy Clin Immunol 111:995–1000
Schäfer T, Meyer T, Ring J, Wichmann HE, Heinrich J (2005) Worm infestation and the negative association with eczema (atopic/nonatopic) and allergic sensitization. Allergy 60:1014–1020
Yazdanbakhsh M, Matricardi PM (2004) Parasites and the hygiene hypothesis: regulating the immune system? Clin Rev Allergy Immunol 26:15–24
Smits HH, Hammad H, van Nimwegen M, Soullie T, Willart MA, Lievers E, Kadouch J, Kool M, Kos-van Oosterhoud J, Deelder AM, Lambrecht BN, Yazdanbakhsh M (2007) Protective effect of Schistosoma mansoni infection on allergic airway inflammation depends on the intensity and chronicity of infection. J Allergy Clin Immunol 120:932–940
Pinelli E, Brandes S, Dormans J, Fonville M, Hamilton CM, der Giessen J (2007) Toxocara canis: effect of inoculum size on pulmonary pathology and cytokine expression in BALB/c mice. Exp Parasitol 115:76–82
Kennedy MW, Qureshi F (1986) Stage-specific secreted antigens of the parasitic larval stages of the nematode Ascaris. Immunology 58:515–522
Lozano MJ, Martín HL, Díaz SV, Mañas AI, Valero LA, Campos BM (2004) Cross-reactivity between antigens of Anisakis simplex s.l. and other ascarid nematodes. Parasite 11:219–223
Acknowledgements
The PIAMA study was funded primarily by grants from the Dutch Asthma Funds, the Ministry of the Environment and ZonMw, the Netherlands Organisation for Health Research and Development.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pinelli, E., Willers, S.M., Hoek, D. et al. Prevalence of antibodies against Ascaris suum and its association with allergic manifestations in 4-year-old children in the Netherlands: the PIAMA birth cohort study. Eur J Clin Microbiol Infect Dis 28, 1327–1334 (2009). https://doi.org/10.1007/s10096-009-0785-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-009-0785-6