Abstract
The incidence of methicillin-resistant Staphylococcus aureus (MRSA) infective endocarditis (IE) is increasing. This study compared clinical characteristics and mortality in patients with methicillin-sensitive S. aureus (MSSA) IE versus MRSA IE, based on a prospectively collected series of 72 consecutive patients with definite S. aureus IE according to the modified Duke criteria between June 2000 and December 2006. Sixteen of 72 IE patients (22%) were caused by MRSA. Nosocomial origin, surgical site infection, surgery in the previous 6 months, the presence of a catheter and persistent bacteremia were significantly associated with MRSA. MSSA patients had significantly more unknown origin of bacteremia and experienced a significantly higher rate of major embolism than MRSA patients. MSSA patients underwent more frequently combined surgical and antimicrobial therapy, and MRSA patients were treated more frequently with antimicrobial therapy due to a contraindication to surgery. The 6-month mortality was higher in patients with MRSA than MSSA. In the MSSA group treated with antimicrobial therapy without an indication to surgery, all patients survived, and in the combined surgical and antimicrobial group 29% died. The mortality in MRSA patients was lowest if combined surgical and antimicrobial therapy was performed. Both in MSSA and MRSA patients with antimicrobial therapy due to a contraindication to surgery, the mortality was extremely high. These data suggest that in S. aureus IE patients with a nosocomial origin, the presence of a catheter or recent surgery, initial therapy should include antimicrobial agents active against MRSA. Antimicrobial therapy alone with close monitoring of the therapeutic effect and signs of complicated course is an acceptable approach in selected patients with MSSA IE. Denial of surgery because of local or general factors in patients that meet criteria for surgical intervention in acute IE is prognostically ominous.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite progress in diagnostic and therapeutic strategies, infective endocarditis (IE) is still associated with a high overall mortality rate of 20–25% [1]. Staphylococcus aureus has emerged as the most common cause of IE [2–6], and is associated with a worse prognosis compared to other microorganisms. Worldwide, rates of methicillin-resistant S. aureus (MRSA) IE are increasing. Only a few series have compared clinical features and outcome in patients with MRSA IE versus methicillin-sensitive S. aureus (MSSA) IE [4, 7, 8]. The current investigation reports the 6.5-year experience of a single tertiary care center with 72 consecutive patients with S. aureus IE, comparing clinical characteristics and mortality in MSSA IE versus MRSA IE. We focused on the therapeutic approach, and evaluated the role for antimicrobial therapy alone, with close monitoring of the therapeutic effect and signs of complicated course in patients with MSSA IE and MRSA IE.
Patients and methods
Patient selection
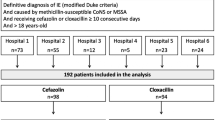
From June 2000 to December 2006, consecutive patients older than 16 years, with definite S. aureus IE according to the modified Duke’s criteria [9], were prospectively registered in a database [5]. Patients were treated according to the American Heart Association guidelines [10, 11], with predefined indications for surgical intervention [12].
Definitions
The portal of entry was defined as a localized focus of S. aureus infection preceding bacteremia (cutaneous origin, catheter-related, surgical site infection, versus unknown origin). The portal of entry was catheter-related if the culture of the catheter tip was positive for S. aureus. Catheters were divided into short-term and long-term catheters. Long-term catheters included a Port-a-cath, a Groshong or a Hickmann catheter. Other central venous catheters were defined as short-term catheters [13, 14].
Nosocomial IE was defined as an infection occurring more than 72 hours after admission to the hospital, or IE acquired in association with a significant invasive procedure performed during a recent hospitalization ≤8 weeks prior to the index hospitalization [15, 16].
The nidus of infection included a prosthetic valve, native valve or other localization of IE.
The presence of foreign material included a catheter, prosthetic valve, pacemaker, orthopedic prosthesis or vascular prosthesis.
Underlying conditions included surgery in the previous 6 months, a pre-existing valvular disorder, prior IE, diabetes mellitus, neoplasm, hepatic cirrhosis, immunosuppression and hemodialysis.
A pre-existing valvular disorder was defined as degenerative or rheumatic valvular disease, bicuspid aortic valve or mitral valve prolapse.
Complications included major embolism, minor embolism, heart failure, septic shock, cardiovascular shock and metastatic infection. Major embolic events were defined as cerebral involvement or peripheral involvement (the limbs, spleen, kidneys or lungs). Minor embolic events included septic emboli at fundoscopic examination (retinal emboli) or cutaneous embolization (skin emboli).
Metastatic infection included septic arthritis, spondylodiscitis and abscess formation in soft tissue.
Persistent fever or persistent bacteremia was defined as fever or positive blood cultures respectively, more than 48 hours after initiation of adequate antimicrobial therapy. Adequate antimicrobial therapy was defined as in vitro sensitivity of S. aureus and adequate dosage of the antibiotic.
Therapy
Treatment modality was divided into combined surgical and antimicrobial therapy, antimicrobial therapy without an indication to surgery and antimicrobial therapy due to a contraindication to surgery. Indications for cardiac surgery included severe valvular dysfunction with heart failure, severe valvular dysfunction without heart failure, abscess or perivalvular extension, failure of conservative medical treatment, and large vegetations with high risk of embolization or (recurrent) embolization during antibiotic treatment. Contraindications to cardiac surgery included major cerebrovascular events with hemorrhagic aspect on CT scan, history of multiple and technically difficult cardiac surgical procedures with inoperability defined during the previous surgery, high operative risk because of cardiopulmonary status, and a poor prognosis for other comorbid conditions e.g. palliative setting.
IE mortality was defined as death attributable to the infection or infection related sequellae.
Data collection
The following data were prospectively collected: epidemiological features including age, gender, nosocomial or community origin of IE, the nidus of infection, methicillin-resistant or -sensitive S. aureus. The portal of entry, underlying conditions, persistent fever and persistent bacteremia were registered. Complications before and during the IE course, including major and minor embolism, heart failure, septic shock, cardiovascular shock and metastatic infection, were noted. IE-related mortality within the 6-month follow-up was assessed.
Statistical analysis
Continuous data were presented as medians and interquartile ranges (IQR), unless stated otherwise. Continuous variables were compared with the Mann-Witney U-test and categorical variables with the chi-squared test or Fisher’s exact test. The patient variables that were analysed in univariable analysis included age, MRSA, gender, the nidus of infection, the origin of IE, the portal of entry, underlying conditions, the presence of a foreign body, persistent fever, persistent bacteremia, treatment modality, complications and outcome. The significance level was P < 0.05. All reported P values were two-sided. Statistical analysis was performed with the SPSS software package (version 10.0, Chicago, IL, USA).
Results
Patient characteristics
Seventy-two consecutive S. aureus IE patients were included. Of these patients, 16 (22%) were caused by MRSA and 56 (78%) by MSSA. The median age of patients with MSSA IE was 67 years (IQR, 50–73) and of patients with MRSA IE 68 years (IQR, 63–75, P = NS). Epidemiological and clinical characteristics of MSSA versus MRSA IE are presented in Table 1. Four of 16 MRSA IE episodes (25%) were of community origin. MSSA IE patients had significantly more unknown origin of bacteremia. MRSA IE involved more frequently prosthetic valves, whereas MSSA IE preferentially affected native valves. There was no significant difference in aortic or mitral valve involvement between MRSA and MSSA patients. In univariable analysis, MRSA IE was significantly associated with a surgical site infection, surgery in the previous 6 months, the presence of a catheter and nosocomial infection. Persistent bacteremia was encountered in 19 patients (26%), and occurred significantly more often in MRSA patients. Other variables significantly associated with persistent bacteremia included a nosocomial origin of IE (P = 0.03), surgery in the previous 6 months (P = 0.04), the presence of a catheter (P = 0.005) and a surgical site infection (P = 0.002). Age, gender, prosthetic or native valve IE, any underlying condition, a cutaneous, unknown or catheter-related portal of entry, a pre-existing valvular defect, the presence of a valvular, orthopedic or vascular prosthesis or pacemaker were not associated with persistent bacteremia.
Complications
Table 2 shows data on complications in MSSA and MRSA patients. MSSA patients experienced a significantly higher rate of major and minor embolic complications than MRSA patients. We investigated whether there was an association between vegetation length and MRSA IE, since only one MRSA patient experienced a major embolism. Transoesophageal echocardiography (TEE) showed a vegetation size of ≥10 mm in 63% of MRSA patients versus in 57% of MSSA patients (P = 0.7).
Treatment
The therapeutic approaches to MSSA and MRSA IE patients were significantly different: MSSA patients underwent more often combined surgical and antimicrobial therapy than MRSA patients (68% versus 38%, P = 0.03) and MRSA patients were treated more frequently with antimicrobial therapy due to a contraindication to surgery than MSSA patients (44% versus 13%, P = 0.005). Seven of 14 patients with MRSA IE had a contraindication to surgery: prior technically difficult cardiac surgery in two, and comorbidities and poor general health in five. Seven of 54 patients with MSSA IE had a contraindication to surgery: complicated cerebral embolism in three, multiorgan failure in two, and poor general health and prior technically challenging cardiac surgery, in one patient each. The rate of antimicrobial therapy without an indication to surgery was similar between MSSA and MRSA patients (20% and 19%, P = 1.0).
Mortality
The overall 6-month mortality rate of patients with S. aureus IE was 26/72 (36%). There was a trend towards higher mortality in patients with MRSA than with MSSA (56% versus 30%, P = 0.06). The mortality rate in community-acquired MRSA patients was 1/4 (25%) versus 8/12 (67%) in nosocomial MRSA patients (P = 0.3). Mortality rates according to MSSA IE versus MRSA IE and to the treatment modality are presented in Table 3. In MSSA patients with antimicrobial therapy without an indication to surgery, the mortality rate was zero, and in patients with combined surgical and antimicrobial therapy 29%. In patients with MRSA, the mortality rate was 17% in the combined surgical and antimicrobial group, and 33% in the antimicrobial group without an indication to surgery. Both in MSSA and MRSA patients with antimicrobial therapy due to a contraindication to surgery, the mortality rate was extremely high, specifically 86% and 100% mortality respectively.
Discussion
Over the past decades, S. aureus has become the most frequent microorganism causing IE. Rates of MRSA are increasing as well, varying from 24% to 51% in recent series [4, 5, 7, 8, 17]. The present study compared clinical characteristics and mortality of 56 MSSA IE patients versus 16 MRSA IE patients, and focused on the therapeutic approach.
The clinical profile of MRSA and MSSA IE patients was different. In particular, patients with MRSA were more likely to have nosocomial IE and MSSA patients community-acquired IE. However, one fourth of MRSA cases were of community origin as well. MRSA IE was more likely to occur in patients with surgery in the previous 6 months, a surgical site infection and the presence of a catheter. MRSA patients had more frequently persistent bacteremia and MSSA patients experienced higher rates of major embolism, findings consistent with previous studies [4, 7, 8, 17]. The reason for the persistence of MRSA bacteremia may be due to the slow eradication of MRSA by vancomycin. Levine et al. found that a slow clinical response was common among patients with MRSA IE who were treated with vancomycin or vancomycin plus rifampin [18]. Yoon et al. showed that the use of vancomycin was associated with persistent bacteremia, albeit non-significantly [7]. Vancomycin is nowadays still the recommended therapy for MRSA IE [11]. However, this recommendation may be challenged, as new agents and combination therapies are studied. MSSA patients experienced significantly higher rates of major embolism than MRSA patients. We investigated whether the reason for this finding was due to the vegetation size, but no difference in vegetation length was found between patients with MRSA and MSSA IE. Several investigators have demonstrated that systemic bacterial infections constitute an independent risk factor for embolism, even in the absence of cardiac involvement. About 10% of bacteremic patients without IE will develop stroke within 1 month of the onset of bacteremia. The mechanisms which could cause thrombo-embolic complications in septic patients are numerous, but activation of the coagulation system is probably the most important [19, 20]. Vaudaux et al. described that, in vitro, some MRSA strains were defective in the production of major surface components such as clumping factor (fibrinogen-binding protein). All strains containing an intact mec element (methicillin resistance) in their chromosomes were found to be defective in adhesion to fibrinogen and fibronectin [21]. Measurement of cell clumping confirmed the lack of the fibrinogen-binding protein-mediated agglutination in the methicillin-resistant transformants. Vaudaux et al. [21] concluded that methicillin resistance altered functional surface expression of fibrinogen and fibronectin adhesins. These findings may offer an explanation for the low incidence of embolism in patients with MRSA.
In this series, patients with MSSA were nearly twice more likely to undergo combined surgical and antimicrobial therapy than MRSA patients, an incidence similar to the one reported by Hsu et al. [17]. Fowler et al. showed similar rates of combined surgical and antimicrobial therapy in MSSA (38%) and MRSA (39%) patients [4]. The most favorable outcome in MSSA patients was found in association with antimicrobial therapy without an indication to surgery, suggesting that there exists a role for watchful waiting in these patients. In patients with MRSA, the outcome was most beneficial in association with combined surgical and antimicrobial therapy. Reasons for inoperability differed between MSSA and MRSA patients. In particular, MRSA patients had mostly prior technically difficult cardiac surgery or an (underlying) unfavorable (comorbid) condition while MSSA patients had mostly complicated cerebral embolism or multiorgan failure.
The mortality rate in patients with MRSA IE was 56%, comparable with data from the literature (50–55%) [7, 17]. The highest mortality rate was registered in nosocomial MRSA patients (67%). Mortality in community-acquired MRSA patients was lower (25%) and resembled more the mortality rate of MSSA IE patients. In agreement with previous studies [4, 7, 8], this study revealed a trend towards higher mortality in patients with MRSA IE than in those with MSSA IE. The reason for this finding may be due to the higher number of MRSA patients with antimicrobial therapy due to a contraindication to surgery, associated with an extremely unfavorable prognosis.
In conclusion, MRSA as the etiologic microorganism should be suspected in patients with S. aureus IE of a nosocomial origin, who underwent surgery in the preceding 6 months or have a catheter or a surgical site infection. In this setting, empirical treatment with antimicrobial therapy active against MRSA should be initiated. Daily blood cultures should be taken since in our study MRSA IE was significantly associated with persistent bacteremia. Septic embolism was caused mainly by IE due to MSSA, and this may be partly explained by the fact that methicillin resistance alters functional surface expression of fibrinogen and fibronectin adhesins. A trend towards higher mortality in patients with MRSA than in MSSA was found. Antimicrobial therapy due to a contraindication to surgery was associated with extreme high mortality. Despite a high operative risk, surgeons should consider proceeding with surgery, if criteria for surgical intervention are fulfilled. S. aureus IE patients with the worst prognosis may benefit from cardiac surgery to improve outcome.
References
Mylonakis E, Calderwood SB (2001) Medical progress: Infective endocarditis in adults. N Engl J Med 345:1318–1330
Mouly S, Ruimy R, Launay O, Arnoult F, Brochet E, Trouillet JL, Leport C, Wolff M (2002) The changing clinical aspects of infective endocarditis: Descriptive review of 90 episodes in a French teaching hospital and risk factors for death. J Infect 45:246–256
Loupa C, Mavroidi N, Boutsikakis I, Paniara O, Deligarou O, Manoli H, Saroglou G (2004) Infective endocarditis in Greece: a changing profile. Epidemiological, microbiological and therapeutic data. Clin Microbiol Infect 10:556–561
Fowler VG Jr, Miro JM, Hoen B, Cabell CH, Abrutyn E, Rubinstein E, Corey GR, Spelman D, Bradley SF, Barsic B, Pappas PA, Anstrom KJ, Wray D, Fortes CQ, Anguera I, Athan E, Jones P, van der Meer JT, Elliott TS, Levine DP, Bayer AS (2005) Staphylococcus aureus endocarditis: a consequence of medical progress. JAMA 293:3012–3021
Hill EE, Herijgers P, Claus P, Vanderschueren S, Herregods MC, Peetermans WE (2007) Infective endocarditis: changing epidemiology and predictors of 6-month mortality: a prospective cohort study. Eur Heart J 28(2):196–203
Cabell CH, Abrutyn E, Fowler VG Jr, Hoen B, Miro JM, Corey GR, Olaison L, Pappas P, Anstrom KJ, Stafford JA, Eykyn S, Habib G, Mestres CA, Wang A (2005) Use of surgery in patients with native valve infective endocarditis: results from the International Collaboration on Endocarditis Merged Database. Am Heart J 150:1092–1098
Yoon HJ, Choi JY, Kim CO, Kim JM, Song YG (2005) A comparison of clinical features and mortality among methicillin-resistant and methicillin-sensitive strains of Staphylococcus aureus endocarditis. Yonsei Med J 46:496–502
Chang FY, MacDonald BB, Peacock JE Jr, Musher DM, Triplett P, Mylotte JM, O’Donnell A, Wagener MM, Yu VL (2003) A prospective multicenter study of Staphylococcus aureus bacteremia: incidence of endocarditis, risk factors for mortality, and clinical impact of methicillin resistance. Medicine (Baltimore) 82:322–332
Li JS, Sexton DJ, Mick N, Nettles R, Fowler VG Jr, Ryan T, Bashore T, Corey GR (2000) Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis 30:633–638
Wilson WR, Karchmer AW, Dajani AS, Taubert KA, Bayer A, Kaye D, Bisno AL, Ferrieri P, Shulman ST, Durack DT (1995) Antibiotic treatment of adults with infective endocarditis due to streptococci, enterococci, staphylococci, and HACEK microorganisms. American Heart Association. JAMA 274:1706–1713
Baddour LM, Wilson WR, Bayer AS, Fowler VG Jr, Bolger AF, Levison ME, Ferrieri P, Gerber MA, Tani LY, Gewitz MH, Tong DC, Steckelberg JM, Baltimore RS, Shulman ST, Burns JC, Falace DA, Newburger JW, Pallasch TJ, Takahashi M, Taubert KA (2005) Infective endocarditis: diagnosis, antimicrobial therapy, and management of complications: a statement for healthcare professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, and the Councils on Clinical Cardiology, Stroke, and Cardiovascular Surgery and Anesthesia, American Heart Association: endorsed by the Infectious Diseases Society of America. Circulation 111:3167–3184
Moon MR, Stinson EB, Miller DC (1997) Surgical treatment of endocarditis. Prog Cardiovasc Dis 40:239–264
Horstkotte D, Follath F, Gutschik E, Lengyel M, Oto A, Pavie A, Soler-Soler J, Thiene G, von Graevenitz A, Priori SG, Garcia MA, Blanc JJ, Budaj A, Cowie M, Dean V, Deckers J, Fernandez Burgos E, Lekakis J, Lindahl B, Mazzotta G, Morais J, Oto A, Smiseth OA, Lekakis J, Vahanian A, Delahaye F, Parkhomenko A, Filipatos G, Aldershvile J, Vardas P (2004) Guidelines on prevention, diagnosis and treatment of infective endocarditis - Executive summary. Eur Heart J 25:267–276
Mermel LA, Farr BM, Sherertz RJ, Raad II, O’Grady N, Harris JS, Craven DE (2001) Guidelines for the management of intravascular catheter related infections. Clin Infect Dis 32:1249–1272
Chen SC, Dwyer DE, Sorrell TC (1992) A comparison of hospital and community-acquired infective endocarditis. Am J Cardiol 70:1449–1452
Terpenning MS, Buggy BP, Kauffman CA (1988) Hospital-acquired infective endocarditis. Arch Intern Med 148:1601–1603
Hsu RB (2005) Risk factors for nosocomial infective endocarditis in patients with methicillin-resistant Staphylococcus aureus bacteremia. Infect Control Hosp Epidemiol 26:654–657
Levine DP, Fromm BS, Reddy BR (1991) Slow response to vancomycin or vancomycin plus rifampin in methicillin-resistant Staphylococcus aureus endocarditis. Ann Intern Med 115:674–680
Valtonen V, Kuikka A, Syrjanen J (1993) Thrombo-embolic complications in bacteraemic infections. Eur Heart J 14(Suppl K):20–23
Syrjanen J (1993) Infection as a risk factor for cerebral infarction. Eur Heart J 14(Suppl K):17–19
Vaudaux PE, Monzillo V, Francois P, Lew DP, Foster TJ, Berger-Bachi B (1998) Introduction of the mec element (methicillin resistance) into Staphylococcus aureus alters in vitro functional activities of fibrinogen and fibronectin adhesins. Antimicrob Agents Chemother 42:564–570
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have no financial interest in this manuscript.
Rights and permissions
About this article
Cite this article
Hill, E.E., Peetermans, W.E., Vanderschueren, S. et al. Methicillin-resistant versus methicillin-sensitive Staphylococcus aureus infective endocarditis. Eur J Clin Microbiol Infect Dis 27, 445–450 (2008). https://doi.org/10.1007/s10096-007-0458-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-007-0458-2