Abstract
Sternal wound infection (SWI) is a serious complication after cardiac surgery. In a previous randomized controlled trial, the addition of local collagen-gentamicin in the sternal wound before wound closure was found to significantly reduce the incidence of postoperative wound infections compared with the routine intravenous prophylaxis of isoxazolyl-penicillin only. The aims of the present study were to analyse the microbiological findings of the SWIs from the previous trial as well as to correlate these findings with the clinical presentation of SWI. Differences in clinical presentation of SWIs, depending on the causative agent, could be identified. Most infections had a late, insidious onset, and the majority of these were caused by staphylococci, predominantly coagulase-negative staphylococci. The clinically most fulminant infections were caused by gram-negative bacteria and presented early after surgery. Local administration of gentamicin reduced the incidence of SWIs caused by all major, clinically important bacterial species. Propionibacterium acnes was identified as a possible cause of SWI and may be linked to instability in the sternal fixation. There was no indication of an increase in the occurrence of gentamicin-resistant bacterial isolates in the treatment group. Furthermore, the addition of local collagen-gentamicin reduced the incidence of SWIs caused by methicillin-resistant coagulase-negative staphylococci. This technique warrants further evaluation as an alternative to prophylactic vancomycin in settings with a high prevalence of methicillin-resistant Staphylococcus aureus.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sternal wound infection (SWI) is a serious complication after cardiac surgery, with a reported incidence of 0.25–25% [1–12] and a mortality rate of up to 31% [1, 10, 13, 14]. Sternal wound infections also constitute an economic burden to the healthcare system, with reported costs for their treatment of US $14,000–40,000 [15–21]. Staphylococcal species are the most common pathogens, accounting for 30–80% of SWIs [1, 5, 22–24].
Intravenous (i.v.) antibiotic prophylaxis is routinely practised in the setting of cardiac surgery. Beta-lactam antibiotics (cephalosporins or, commonly used in Sweden, isoxazolyl-penicillins) are used most frequently. However, most coagulase-negative staphylococci (CoNS) are methicillin resistant, due to the presence of the mecA gene, and are therefore resistant to all beta-lactam antibiotics [25]. (For these CoNS, the abbreviation MRSE [methicillin-resistant Staphylococcus epidermidis] will be used, although these CoNS were not typed to species level). Methicillin-resistant Staphylococcus aureus (MRSA) has also emerged as a potential pathogen in postoperative SWIs. The use of vancomycin, often the only antibiotic effective against MRSA and MRSE, as prophylaxis is discouraged because of the risk of selection of resistant bacteria, with subsequent ecological and therapeutic consequences [26]. Furthermore, vancomycin is intrinsically a less active antistaphylococcal agent than are beta-lactam antibiotics. In a recent meta-analysis, i.v. beta-lactam antibiotics were superior to glycopeptides, such as vancomycin, in preventing SWI after cardiac surgery [27].
In a previous randomized controlled trial (Local Gentamicin for Sternal Wound Infection Prophylaxis (LOGIP) trial) [1], the addition of local collagen-gentamicin in the sternal wound before wound closure significantly reduced the incidence of postoperative wound infections compared with routine i.v. prophylaxis of isoxazolyl-penicillin alone. The same trend, although not statistically significant, was observed in another similar study [28]. The aims of the present study were to analyse the microbiological findings of SWIs from the LOGIP trial with regard to antibiotic prophylaxis and to establish how the microbiological findings influenced clinical manifestation of SWIs.
Materials and methods
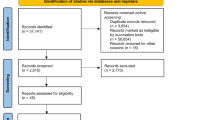
The LOGIP trial and its primary endpoint have been described elsewhere [1]. Briefly, 2,000 cardiac surgery patients at two cardiothoracic centres (Linköping and Örebro, Sweden) were randomised to routine prophylaxis with i.v. isoxazolyl-penicillin only (control group) or to the same prophylaxis combined with application of collagen-gentamicin (260 mg gentamicin) sponges (Collatamp-G; at the time of the trial, Schering-Plough, Stockholm, Sweden; presently Innocoll Pharmaceuticals, Athlone, Ireland) in the sternotomy wound before wound closure (treatment group). The primary endpoint was any SWI within 2 months postoperatively. Evaluations (which were double-blind and made on an intention-to-treat basis) in 967 and 983 patients in the control and treatment groups, respectively, showed that the total incidence of SWI was 9.0% in the control group compared with 4.3% in the treatment group. There was no significant difference in total 60-day mortality (1.9 vs. 1.8% in the treatment and control groups, respectively), or in median length of postoperative stay (6 days in both groups).
Bacterial samples
In patients who underwent surgical revision of the wound due to SWI, we collected five bacterial samples from the wound for bacterial culture, of which at least two were tissue samples. The samples were cultured aerobically and anaerobically for at least 5 days on blood agar medium (Columbia II Agar 4.25% w/v, horse blood, defibrinized, 6% v/v; SVA, Uppsala, Sweden) as well as in enrichment broth (fastidious anaerobe broth 29.7% w/v; Lab M, Lancashire, UK; and D+ glucose 10.0% w/v; J.T. Baker, Deventer, Holland) for 7 days. In infected patients handled at referring hospitals, cultures were collected on clinical indication only, and the isolates were not regularly stored for further analysis.
For the purpose of the present study, all results from the bacterial cultures were reviewed by a specialist in infectious diseases and/or clinical microbiology who was blinded to the group to which the patient had been allocated. In cases with multiple pathogens, the probable primary causative agent was purposely selected where possible, and agents that were considered to be contaminants were excluded from further analysis.
Routine microbiological diagnostic procedures were used for identification of bacterial isolates. Susceptibility testing was performed by the disc diffusion method (Oxoid, Hampshire, UK) and determination of minimal inhibitory concentrations (MICs) by the E test (AB Biodisk, Solna, Sweden); all breakpoints used were those recommended by the Swedish Reference Group for Antibiotics (http://www.srga.org). Staphylococcal isolates with an MIC of ≤1 mg/l for oxacillin, ≤1 mg/l for gentamicin/netilmicin, and ≤4 mg/l for vancomycin were considered susceptible.
Clinical presentation
The interval from surgery to presentation of SWI was noted and related to microbiological findings. The symptoms of SWI, as reported by the patient and/or documented in the patient’s medical record, were classified as one or more of the following: secretion from the wound, redness of the wound, feeling of unstable sternal fixation, and presence of fever >38.5°C (during the SWI or within 3 days before diagnosis of SWI). The highest plasma level of C-reactive protein (p-CRP) during the SWI or within 3 days before diagnosis of SWI was recorded, where available, and related to the microbiological findings.
The infections were classified, according to the criteria for definition and classification of surgical site infections from the Centers for Disease Control and Prevention, as superficial, deep incisional (involving the sternum/sternal wires), or deep organ/space (involving the mediastinum/pericardium) infections [26]. The superficial infections were further divided into subcutaneous infections or cutaneous infections, the latter including most superficial infections, such as infected crusts.
Cost
The cost of the treatment of the SWI was used as a measurement of the general clinical severity of the infection and was related to the microbiological findings. Cost was calculated as reported previously [21]. The analysis was made from the perspective of the healthcare provider, excluding societal costs, using predominantly gross costing.
Statistical analysis
For categorical variables (to compare proportions), a two-sided p value was calculated with Pearson’s chi-square test or with Fisher’s exact test when expected frequencies were <5. For continuous variables, the Mann–Whitney test was used. A p value of less than 0.05 was considered significant. No correction for multiple analyses was applied. For the statistical analyses, Statistica 7.0 software (StatSoft, Tulsa, OK, USA) and SPSS 13.0 software (SPSS, Chicago, IL, USA) were used.
Results
Bacterial samples
A total of 129 SWIs were analysed. The microbial findings and their relative frequencies within each treatment group are shown in Table 1. Both the absolute and the relative incidence of each of the three clinically important agents, S. aureus, CoNS, and gram-negative bacteria, were lower in the treatment group. Propionibacterium acnes was the only agent for which there was no absolute reduction in the rate of infections in the treatment group.
Antibiotic susceptibility data were available for gentamicin in 47 of 77 (61%) cases of SWIs caused by staphylococcal species; for methicillin, data were available in 62 of 77 (81%) cases. All S. aureus isolates tested were susceptible to both gentamicin and methicillin. There was a significant difference in the number of SWIs caused by gentamicin-susceptible CoNS (15 in the control group and 5 in the treatment group, p = 0.022) but not in SWIs caused by gentamicin-resistant CoNS (six and five SWIs in the treatment and control groups, respectively), (Fig. 1). There was a parallel difference in both methicillin-susceptible CoNS and MRSE, with seven MRSE infections in the treatment group and 16 in the control group (p = 0.05). Determination of MIC values for gentamicin by the E test was performed for 20 CoNS isolated from 8 of the 11 patients with CoNS who were reoperated on at one of the centres because of SWI. The MIC values ranged from <0.016 to 32 mg/l. No high-level gentamicin-resistant CoNS, i.e. with an MIC value >256 mg/l, was found. All staphylococci that were tested against vancomycin (48 of 77) were susceptible.
Patterns of antibiotic susceptibility for gentamicin (top) and methicillin (bottom) in the treatment and control groups among the staphylococci isolated from the sternal wound infections. Susceptibility was determined in 47 (61%) and 62 (81%) of all staphylococcal wound infections for gentamicin and methicillin, respectively. CoNS coagulase-negative staphylococci, R resistant, S susceptible
Detailed comparisons of antibiotic susceptibility for each of the groups of agents other than staphylococci were not performed.
Clinical presentation
Timing of the first presentation of symptoms of SWI was possible to establish in 108 of the 129 cases (in 79 and 86% in the treatment and control groups, respectively). The interval between surgery and symptoms of SWI was shortest for infections caused by gram-negative bacteria (median 5 days, range 2–20 days) and longest for infections caused by S. aureus (median 20 days, range 5–62 days) (p = 0.008) (Fig. 2).
Secretion from the wound was the most common symptom of SWI and was present in 84.5% of all cases and in 92% of all staphylococcal infections (Table 2). Infections caused by S. aureus and gram-negative bacteria were characterized by high p-CRP levels and a high proportion of patients with fever. However, patients with SWIs caused by S. aureus had a lower reported frequency of sternal instability (3.6%) than patients with infections caused by gram-negative bacteria (40.0%) or P. acnes (38.5%) (p = 0.01 and p < 0.01, respectively). Patients with P. acnes, in contrast, showed comparatively low p-CRP levels, despite early presentation of these infections.
There was a difference in the effect of local gentamicin on different symptoms of SWI, with a significant reduction in symptoms of redness (2.9 vs. 6.1%, p = 0.001) and secretion from the wound (3.7 vs. 7.5%, p < 0.001) in the treatment group compared with the control group, but no reduction in the symptom of sternal instability (1.3 and 1.1% in the treatment and control groups, respectively).
Cost
Sternal wound infections caused by gram-negative bacteria were associated with few less serious (and few late) infections and with the highest mean cost for their treatment (Table 2 and Fig. 3). In some patients with SWI caused by S. aureus, infections were costly, but in another, larger patient group with S. aureus, infections were less serious and mostly late-onset. Cases caused by CoNS demonstrated a similar heterogeneity, with a small proportion of very costly and severe SWIs. In fact, two out of three SWIs with a treatment cost exceeding EUR 100,000 were caused by CoNS, while the third case was caused by gram-negative bacteria (Pseudomonas aeruginosa) (Fig. 3).
Discussion
In this study, postoperative SWIs were associated with different clinical presentations and characteristics, depending on the microbiological findings. Sternal wound infections caused by gram-negative bacteria were clinically severe and were characterised by early onset, high p-CRP levels, a high proportion of cases with an unstable sternum, and the highest mean cost for their treatment. By contrast, staphylococcal infections (both S. aureus and CoNS) usually presented later and with local symptoms, with secretion from the wound as their predominant manifestation.
Differences in the clinical appearance of the SWI with regard to the causative microbial agent have been recognised by others [22, 29]. Somewhat surprisingly, in our study S. aureus infections had a later onset of symptoms than did infections caused by CoNS, even though S. aureus is generally considered a more virulent agent. However, S. aureus infections constituted a heterogenic group, with a smaller proportion of early, more severe infections and a larger proportion of late, superficial infections. The late presentation of most SWIs in our study is notable but is in accordance with the findings in other studies with complete follow-up [2, 9]. A follow-up with registration of all SWIs until discharge from the cardiothoracic unit not only underestimates the magnitude of the problem; it also carries the risk of providing a skewed picture with an over-representation of gram-negative infections.
The clinical presentation of sternal instability or dehiscence is complex with regard to infection. It is an obvious consequence of a fulminant mediastinitis with destruction of sternal bone tissue, and it has been described as a risk factor for the development of SWI [8, 12, 29, 30]. Pure mechanical instability, without clinical infection, has been described as being comparatively frequent even in the presence of positive cultures [23], but in the LOGIP trial we only found one case with negative cultures. In orthopaedic surgery, it has been recommended that the cutoff for a definite diagnosis of prosthetic joint infection at revision arthroplasty be three or more operative specimens that yield an indistinguishable organism [31]. In the LOGIP trial, all cases with bacterial growth in two or more samples of undistinguishable isolates with the same antimicrobial susceptibility pattern were classified as an SWI. Obviously, the number and quality as well as the interpretation of the bacterial samples from the wound are of importance in defining an SWI.
The role of CoNS and P. acnes deserves attention in the context of sternal instability. Propionibacterium acnes is known to cause postoperative wound infections, particularly in neurosurgery, but its role in postoperative SWI is unclear [23]. A high proportion of sternal dehiscence and an early onset despite low p-CRP levels characterised the SWIs caused by P. acnes in our study. Therefore, the possibility of primary mechanical sternal instability with secondary contamination of P. acnes should be considered, although clinical signs of wound infection were frequently present. Preliminary analyses of the P. acnes isolates have revealed that they were not clonally identical, excluding the outbreak of a single strain. Further analysis of the SWIs with growth of P. acnes and characterisation of these isolates is warranted. The association between CoNS and sternal instability has been well documented [23, 29, 30]. Both CoNS and P. acnes belong to the normal skin flora and are agents with low virulence potential. Hence, it is conceivable that host factors such as unstable sternal fixation play an important role in the pathogenesis of these infections. In orthopaedic surgery, a stable, rigid fixation of fractures has been shown to reduce the infection rate, despite the presence of foreign material, in both experimental and clinical studies [32–34]. In cardiac surgery, a prospective randomized trial demonstrated a lower incidence of SWI with a modified technique of sternal fixation [35].
One aim of applying local gentamicin was to find an ecologically appealing and at the same time efficient alternative to vancomycin as a prophylaxis for SWIs caused by MRSE and MRSA. The analyses of antibiotic resistance showed that local application of gentamicin resulted in a parallel reduction in SWI caused by both methicillin-susceptible and methicillin-resistant CoNS strains. There were no MRSA infections in our study; however, surgical wound infections caused by MRSA, including SWI, are a well-recognised and growing concern internationally. A reduction in MRSA infections would therefore be of clinical importance, especially since the results from studies on routine i.v. vancomycin prophylaxis in cardiac surgery have been disappointing [27].
Beta-lactam agents in combination with aminoglycosides, as well as the addition of a single dose of gentamicin to vancomycin or to daptomycin, have shown potent activity against MRSA in vitro [36, 37]. Although the possibility of aminoglycoside resistance among MRSA must be considered, recent reports from Europe and the USA indicate that most MRSA strains may be susceptible to gentamicin [38, 39]. The use of local gentamicin in conjunction with i.v. antibiotics could therefore offer an attractive alternative to vancomycin and deserves attention and evaluation in surgical settings with high prevalence rates of MRSA.
Theoretically, routine application of local gentamicin could lead to selection of gentamicin-resistant strains over time. However, compared with i.v. treatment, the short, single, and very high peak in local gentamicin concentration does not favour selection of resistant strains [40]. Furthermore, local gentamicin could lead to a reduction in the number of SWIs caused by CoNS isolates classified as gentamicin resistant according to the breakpoint of ≤4 mg/l, since very high tissue concentrations are achieved by local application [40]. No high-level gentamicin-resistant CoNS were found among those isolates obtained during reoperation. In our study, local gentamicin neither increased nor reduced the incidence of SWI caused by gentamicin-resistant CoNS. It is too early to draw definite conclusions on this issue based on these results because of the small number of bacterial samples. The technique warrants careful monitoring when introduced as a clinical routine.
In summary, differences in the clinical presentation of SWIs were identified with different causative agents. The most common agents were staphylococci (CoNS followed by S. aureus), and many infections caused by these pathogens were late-onset. The clinically most severe infections, measured by the cost of their treatment, were caused by CoNS, although gram-negative bacteria generally caused the most fulminant infections and were associated with an early onset. The role of P. acnes in SWI, especially in combination with sternal dehiscence, remains unclear. Local gentamicin reduced the incidence of SWIs caused by all major clinically important bacterial species except P. acnes. No indication of any increase in the occurrence of gentamicin-resistant isolates was detected, but this issue needs further surveillance in the future. The addition of local collagen-gentamicin reduced the incidence of SWIs caused by MRSE and deserves evaluation as an alternative to vancomycin as prophylaxis in areas with a high prevalence of MRSA.
References
Friberg Ö, Svedjeholm R, Söderquist B, Granfeldt H, Vikerfors T, Källman J (2005) Local gentamicin reduces sternal wound infections after cardiac surgery: a randomized controlled trial. Ann Thorac Surg 79:153–161
Jonkers D, Elenbaas T, Terporten P, Nieman F, Stobberingh E (2003) Prevalence of 90-days postoperative wound infections after cardiac surgery. Eur J Cardio-thorac Surg 23:97–102
Wilson AP, Weavill C, Burridge J, Kelsey MC (1990) The use of the wound scoring method “ASEPSIS” in postoperative wound surveillance. J Hosp Infect 16:297–309
Wilson AP, Treasure T, Gruneberg RN, Sturridge MF, Ross DN (1988) Antibiotic prophylaxis in cardiac surgery: a prospective comparison of two dosage regimens of teicoplanin with a combination of flucloxacillin and tobramycin. J Antimicrob Chemother 21:213–223
Sharma M, Berriel-Cass D, Baran JJ (2004) Sternal surgical-site infection following coronary artery bypass graft: prevalence, microbiology, and complications during a 42-month period. Infect Control Hosp Epidemiol 25:468–471
Stahle E, Tammelin A, Bergstrom R, Hambreus A, Nystrom SO, Hansson HE (1997) Sternal wound complications—incidence, microbiology and risk factors. Eur J Cardio-thorac Surg 11:1146–1153
Antunes PE, Bernardo JE, Eugenio L, de Oliveira JF, Antunes MJ (1997) Mediastinitis after aorto-coronary bypass surgery. Eur J Cardio-thorac Surg 12:443–449
Baskett RJ, MacDougall CE, Ross DB (1999) Is mediastinitis a preventable complication? A 10-year review. Ann Thorac Surg 67:462–465
Hall JC, Hall JL, Edwards MG (1998) The time of presentation of wound infection after cardiac surgery. J Qual Clin Pract 18:227–231
Ridderstolpe L, Gill H, Granfeldt H, Ahlfeldt H, Rutberg H (2001) Superficial and deep sternal wound complications: incidence, risk factors and mortality. Eur J Cardio-thorac Surg 20:1168–1175
The Parisian Mediastinitis Study Group (1996) Risk factors for deep sternal wound infection after sternotomy: a prospective, multicenter study [see comments]. J Thorac Cardiovasc Surg 111:1200–1207
Losanoff JE, Richman BW, Jones JW (2002) Disruption and infection of median sternotomy: a comprehensive review. Eur J Cardio-thorac Surg 21:831–839
De Feo M, Gregorio R, Della Corte A, Marra C, Amarelli C, Renzulli A et al (2001) Deep sternal wound infection: the role of early debridement surgery. Eur J Cardio-thorac Surg 19:811–816
Astudillo R, Vaage J, Myhre U, Karevold A, Gardlund B (2001) Fewer reoperations and shorter stay in the cardiac surgical ward when stabilising the sternum with the Ley prosthesis in post-operative mediastinitis. Eur J Cardio-thorac Surg 20:133–139
Hollenbeak CS, Murphy D, Dunagan WC, Fraser VJ (2002) Nonrandom selection and the attributable cost of surgical-site infections. Infect Control Hosp Epidemiol 23:177–182
Hollenbeak CS, Murphy DM, Koenig S, Woodward RS, Dunagan WC, Fraser VJ (2000) The clinical and economic impact of deep chest surgical site infections following coronary artery bypass graft surgery. Chest 118:397–402
Jenney AW, Harrington GA, Russo PL, Spelman DW (2001) Cost of surgical site infections following coronary artery bypass surgery. Aust NZ J Surg 71:662–664
Loop FD, Lytle BW, Cosgrove DM, Mahfood S, McHenry MC, Goormastic M et al (1990) J. Maxwell Chamberlain memorial paper. Sternal wound complications after isolated coronary artery bypass grafting: early and late mortality, morbidity, and cost of care. Ann Thorac Surg 49:179–186
Mauldin PD, Weintraub WS, Becker ER (1994) Predicting hospital costs for first-time coronary artery bypass grafting from preoperative and postoperative variables. Am J Cardiol 74:772–775
Taylor GJ, Mikell FL, Moses HW, Dove JT, Katholi RE, Malik SA et al (1990) Determinants of hospital charges for coronary artery bypass surgery: the economic consequences of postoperative complications. Am J Cardiol 65:309–313
Friberg Ö, Dahlin L-G, Levin L-Å, Magnusson A, Granfeldt H, Källman J et al (2006) Cost effectiveness of local collagen-gentamicin as prophylaxis for sternal wound infections in different risk groups. Scand Cardiovasc J 40:117–125
Tegnell A, Aren C, Öhman L (2000) Coagulase-negative staphylococci and sternal infections after cardiac operation. Ann Thorac Surg 69:1104–1109
Tammelin A, Hambraeus A, Stahle E (2002) Mediastinitis after cardiac surgery: improvement of bacteriological diagnosis by use of multiple tissue samples and strain typing. J Clin Microbiol 40:2936–2941
Tang GH, Maganti M, Weisel RD, Borger MA (2004) Prevention and management of deep sternal wound infection. Semin Thorac Cardiovasc Surg 16:62–69
Chambers HF (1997) Methicillin resistance in staphylococci: molecular and biochemical basis and clinical implications. Clin Microbiol Rev 10:781–791
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR (1999) Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol 20:250–278, quiz 279–280
Bolon MK, Morlote M, Weber SG, Koplan B, Carmeli Y, Wright SB (2004) Glycopeptides are no more effective than beta-lactam agents for prevention of surgical site infection after cardiac surgery: a meta-analysis. Clin Infect Dis 38:1357–1363
Eklund AM, Valtonen M, Werkkala KA (2005) Prophylaxis of sternal wound infections with gentamicin-collagen implant: randomized controlled study in cardiac surgery. J Hosp Infect 59:108–112
Gårdlund B, Bitkover CY, Vaage J (2002) Postoperative mediastinitis in cardiac surgery—microbiology and pathogenesis. Eur J Cardio-thorac Surg 21:825–830
Fynn-Thompson F, Vander Salm TJ (2004) Methods for reduction of sternal wound infection. Semin Thorac Cardiovasc Surg 16:77–80
Atkins BL, Athanasou N, Deeks JJ, Crook DW, Simpson H, Peto TE et al The OSIRIS Collaborative Study Group (1998) Prospective evaluation of criteria for microbiological diagnosis of prosthetic-joint infection at revision arthroplasty. J Clin Microbiol 36:2932–2939
Friedrich B, Klaue P, Worlock P, Slack R, Harvey L, Mawhinney R et al (1977) Mechanical stability and post-traumatic osteitis: an experimental evaluation of the relation between infection of bone and internal fixation. Injury 9:23–29
Worlock P, Slack R, Harvey L, Mawhinney R (1994) The prevention of infection in open fractures: an experimental study of the effect of fracture stability. Injury 25:31–38
Koury M, Ellis E 3rd (1992) Rigid internal fixation for the treatment of infected mandibular fractures. J Oral Maxillofac Surg 50:434–443 (discussion 443–434)
Bottio T, Rizzoli G, Vida V, Casarotto D, Gerosa G (2003) Double crisscross sternal wiring and chest wound infections: a prospective randomized study. J Thorac Cardiovasc Surg 126:1352–1356
Huang V, Rybak MJ (2005) Pharmacodynamics of cefepime alone and in combination with various antimicrobials against methicillin-resistant Staphylococcus aureus in an in vitro pharmacodynamic infection model. Antimicrob Agents Chemother 49:302–308
Tsuji BT, Rybak MJ (2005) Short-course gentamicin in combination with daptomycin or vancomycin against Staphylococcus aureus in an in vitro pharmacodynamic model with simulated endocardial vegetations. Antimicrob Agents Chemother 49:2735–2745
Ghebremedhin B, Konig W, Konig B (2005) Heterogeneity of methicillin-resistant Staphylococcus aureus strains at a German university hospital during a 1-year period. Eur J Clin Microbiol Infect Dis 24:388–398
Fridkin SK, Hageman JC, Morrison M, Sanza LT, Como-Sabetti K, Jernigan JA et al (2005) Methicillin-resistant Staphylococcus aureus disease in three communities. N Engl J Med 352:1436–1444
Friberg Ö, Jones I, Sjöberg L, Söderquist B, Vikerfors T, Källman J (2003) Antibiotic concentrations in serum and wound fluid after local gentamicin or intravenous dicloxacillin prophylaxis in cardiac surgery. Scand J Infect Dis 35:251–254
Acknowledgements
This study was funded by grants from the Research Committee of Örebro County Council, which, together with Schering-Plough AB (Stockholm, Sweden), financed the original LOGIP trial. The sponsors had no role in the study design, the analysis, or the interpretation of data, or in the writing or the decision to submit this paper for publication.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Friberg, Ö., Svedjeholm, R., Källman, J. et al. Incidence, microbiological findings, and clinical presentation of sternal wound infections after cardiac surgery with and without local gentamicin prophylaxis. Eur J Clin Microbiol Infect Dis 26, 91–97 (2007). https://doi.org/10.1007/s10096-006-0252-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-006-0252-6