Abstract
Pneumocystis jiroveci pneumonia is a common infection in patients with AIDS but an infrequent cause of pneumonia in cancer patients. Little is known about the impact of cancer type and hematopoietic stem cell transplantation on the presentation and outcome of P. jiroveci pneumonia in cancer patients. A retrospective cohort study of all patients with cancer and P. jiroveci pneumonia cared for at The M.D. Anderson Cancer Center during 1990–2003 was conducted. Eighty episodes of P. jiroveci pneumonia in 79 patients were identified. In most (67%) episodes, patients had a hematologic malignancy. In 23 (29%) episodes, patients had undergone hematopoietic stem cell transplantation. Twenty-seven percent of patients with histopathologically confirmed P. jiroveci pneumonia had nodular infiltrates on the radiographic study. Pleural effusion and pneumothorax were more common in patients with hematopoietic stem cell transplantation than in those with solid tumors. Clinical suspicion of P. jiroveci pneumonia was less common in patients with nodular infiltrates than in those without such a radiographic finding (7 vs. 39%; p=0.002). Twenty-six of 76 (34%) patients with data available died of P. jiroveci pneumonia. Predictors of death by univariate analysis included older age, tachypnea, high APACHE II score, use of mechanical ventilation or vasopressors, lower arterial pH level, absence of interstitial component, pneumothorax, and comorbid conditions (all p<0.05). Multivariate analysis identified the use of mechanical ventilation as an independent predictor of death. Death attributable to P. jiroveci pneumonia appeared to be higher in patients with hematopoietic stem cell transplantation. The clinical presentation of P. jiroveci pneumonia in cancer patients may be affected by the category of cancer and the history of hematopoietic stem cell transplantation. P. jiroveci pneumonia remains a rare yet severe infection in cancer patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pneumocystis jiroveci formerly Pneumocystis carinii pneumonia (PCP) is a well-recognized life-threatening infection in patients with AIDS, leukemia, and lymphoma, in patients who have undergone hematopoietic stem cell transplantation (HSCT), and in patients receiving high doses of systemic corticosteroids [1–7]. The AIDS pandemic brought a surge in studies on PCP, since PCP is a common infection in AIDS patients [2]. PCP is less common among cancer patients, including those who have undergone HSCT [2, 8–10].
Several studies have contrasted the clinical manifestations of PCP in patients with and in patients without AIDS [11–13]. To our knowledge, however, few data have been published on the impact of different types of cancer and hematopoietic stem cell transplantation (HSCT) on the presentation and outcome of PCP in cancer patients [14].
We sought to determine the incidence of, the risk factors for, and the clinical characteristics and outcome of PCP in cancer patients according to type of cancer and history of HSCT. To that end, we reviewed our 14-year experience at our tertiary cancer center.
Patients and methods
Patient identification
To identify patients with cancer and PCP, we reviewed the pathology and autopsy reports for all patients with cancer cared for at The University of Texas M.D. Anderson Cancer Center between January 1990 and December 2003. This study was approved by the Institutional Review Board.
Definitions
PCP was defined as the identification of P. jiroveci by Gomori methenamine silver staining in a respiratory specimen (e.g., bronchoalveolar lavage specimen or lung tissue) or in autopsy material from a patient with clinical or radiographic evidence of pneumonia. Coinfections were defined as other infections that occurred within 1 month of the episode of PCP. A high dose of corticosteroids was defined as a cumulative dose of at least 600 mg of a prednisone equivalent within the 1 month before the diagnosis of PCP. Breakthrough infection was defined as PCP occurring in a patient who received prophylactic agents with known activity against P. jiroveci (e.g., trimethoprim-sulfamethoxazole [TMP-SMX], pentamidine) administered for at least 7 days before the diagnosis of PCP. Neutropenia was defined as a neutrophil count of less than 500 neutrophils/ml. Lymphopenia was defined as a lymphocyte count of less than 1,000 lymphocytes/ml. AIDS was defined according to standardized criteria [15].
Prophylaxis and outcome of P. jiroveci pneumonia
PCP prophylaxis was administered routinely to patients who underwent hematopoietic stem cell transplantation (HSCT) and to patients with lymphoid malignancies treated with purine analogs or corticosteroids. In patients undergoing allogeneic HSCT, PCP prophylaxis consisted of TMP-SMX double-strength twice a day from day 8 before HSCT through day 2 before HSCT. After engraftment, TMP-SMX was reinitiated and administered twice a week and was continued for 1 year after HSCT. In patients who were allergic to sulfa drugs, inhaled administration of pentamidine every 3 weeks was substituted for TMP-SMX.
In patients undergoing autologous HSCT, PCP prophylaxis consisted of TMP-SMX twice a day from admission through day 2 before HSCT. After absolute neutrophil counts reached 1,500 cells/ml, TMP-SMX was reinitiated and administered twice a week and was continued for 6 months after HSCT. Similarly, pentamidine every 3 weeks was used for sulfa-allergic patients.
Death was attributed to PCP if death was due to progressive respiratory failure in a patient with documented PCP.
Statistical analysis
Fisher’s exact test was used to analyze the distribution of all groups. Survival was estimated using the Kaplan-Meier nonparametric method, with the log-rank test used to determine statistical significance. Univariate and multivariate Cox proportional hazards regression analyses were conducted to evaluate the crude effects of each potential predictor on PCP-associated death. All tests were two-sided. Differences were considered statistically significant when p was less than 0.05. Statistical analysis was performed using SPSS version 11.0 statistical software (SPSS, Chicago, IL, USA).
Results
Incidence and patient characteristics
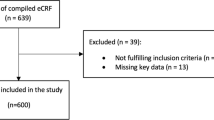
Of the patients with cancer seen at our institution during the study period, 79 had PCP. One of these patients had two separate episodes of PCP, for a total of 80 episodes. The incidence of PCP was 41 cases per 100,000 patients. The incidence among patients with hematologic malignancies was higher than the incidence among patients with solid tumors (187 vs. 16 cases per 100,000 patients; p<0.001). The incidence among patients who underwent HSCT was 386 cases per 100,000 patients; the incidence was similar in patients who underwent allogeneic HSCT and in those who underwent autologous HSCT. The incidence among cancer patients and among patients who underwent HSCT remained stable by year over the study period.
The patient characteristics associated with episodes of PCP are presented in Table 1. The median age at diagnosis of PCP was 48 years (range, 7–82 years). The majority of episodes of PCP occurred in patients with hematologic malignancies (53 of 80 [66%]), most of whom had either leukemia (49%) or lymphoma (45%). Twenty-three (29%) patients had undergone HSCT, of whom 13 had undergone allogeneic HSCT. The median time from HSCT to PCP diagnosis was 263 days (range, 13–1,956 days). Four of the 13 patients who had undergone allogeneic HSCT developed PCP at least 1 year after transplantation (range, 148–486 days); of these, three had graft-versus-host disease and were receiving high-dose corticosteroids. Four of the ten patients who had undergone autologous HSCT developed PCP at least 6 months after transplantation (range, 13–1,956 days); of these, two were receiving high-dose corticosteroids.
Several patient characteristics varied according to the underlying condition (Table 1). Clinical suspicion of PCP was less common in patients with hematologic malignancies than in those with solid tumors (Table 1). The median duration of symptoms before admission was comparable in patients with hematologic malignancies and in those with solid tumors.
In 50 (63%) episodes, chemotherapy or immunosuppressive drugs had been administered to the patient within 1 month before the diagnosis of PCP (Table 1). Five (6%) patients were treated with a regimen containing purine analogs (e.g., fludarabine, cladribine, pentostatin). In 54 (68%) episodes, corticosteroids had been administered to the patient within 1 month before the diagnosis of PCP. In 31 of these cases, high-dose corticosteroids were given. The cumulative dose of corticosteroids at the time of diagnosis of PCP was lower in patients with hematologic malignancies than in those who underwent HSCT (Table 1).
Ten of the 67 (15%) cancer patients with known HIV serostatus were HIV positive, and all ten had AIDS. Prior treatment with corticosteroids, chemotherapy, or immunosuppressive drugs was more common in cancer patients without AIDS than in those with AIDS (p≤0.01).
Clinical presentation of P. jiroveci pneumonia at diagnosis
All patients but one were symptomatic at the time of diagnosis, mainly with fever (86%), dyspnea (75%), and dry cough (70%). In 40 (50%) episodes, patients were admitted to the intensive care unit; in 32 of these episodes, mechanical ventilation was required (Table 1). Admission to the intensive care unit was more common in patients with solid tumors than in those with hematologic malignancies (Table 1).
At diagnosis of infection, neutropenia was uncommon (11%), whereas lymphopenia was common (78%) (Table 1). The duration of lymphopenia was significantly longer in patients with hematologic malignancies than in those who underwent HSCT (p=0.009) (Table 1). Data on CD4+ T-lymphocyte counts within 6 months of infection were available for 14 episodes; the median cell count was 46 cells/mm3 (range, 4–750 cells/mm3). The median CD4+ T-cell count was 19 cells/mm3 (range, 4–57 cells/mm3) among AIDS patients and 55 cells/mm3 (range, 13–750 cells/mm3) among non-AIDS patients. There was a trend (p=0.07) toward a higher median serum lactate dehydrogenase (LDH) level at diagnosis of infection in patients with solid tumors compared to patients who underwent HSCT (Table 1). AIDS patients had a significantly higher median serum LDH level at diagnosis of infection compared to those without AIDS (median 1,438 IU/l, range 820–28,736 IU/l, vs. median 981, range 352–47,810 IU/l; p=0.02).
Information on PCP prophylaxis was not regularly reported except for patients who underwent HSCT. Seven HSCT patients were receiving PCP prophylaxis at the onset of infection (median, 67 days; range, 3–230 days). For the entire cohort of patients, six cases of breakthrough PCP were identified, most of which (5 of 6 [83%]) occurred in HSCT patients. Five cases occurred in patients receiving inhaled (3 patients) or intravenous (2 patients) pentamidine, and one occurred in a patient receiving TMP-SMX prophylaxis. In 57 (71%) episodes, patients had coinfections. The most common copathogens were cytomegalovirus (42%), Staphylococcus aureus (21%), Aspergillus spp. (16%), and Stenotrophomonas maltophilia (11%). In 46 of these cases, the coinfection involved the lungs.
Diagnosis
In 73 (91%) episodes, the diagnosis of PCP was based on the identification of P. jiroveci in only one respiratory sample. The rate of identification of P. jiroveci was significantly higher with bronchoalveolar lavage specimens than with lung tissue specimens (72 of 73 specimens [99%] vs. 15 of 19 specimens [79%]; p=0.005). In some patients, PCP was diagnosed by more than one method. In six patients, PCP was diagnosed postmortem. Four of the 15 (27%) patients with histopathologically confirmed PCP had nodular infiltrates on the radiographic evaluation.
In most cases (90%), there were bilateral infiltrates on the initial radiographic study. Pleural effusion was more common in patients who underwent HSCT than in those with solid tumors (Table 1). There was a trend (p=0.06) toward a higher occurrence of spontaneous pneumothorax in patients who underwent HSCT than in patients with solid tumors (Table 1). Clinical suspicion of PCP was less common in patients with nodular infiltrates than in those without such a radiographic finding (7 vs. 39%, p=0.002).
Therapy and outcome
Antimicrobial therapy was given in 79 of 80 (99%) episodes. As initial therapy, the most common antimicrobial regimen used for PCP consisted of TMP-SMX monotherapy in 53 (67%) episodes. In 21 (27%) episodes, patients were treated with combination antimicrobial therapy. There was a trend toward combination antimicrobial therapy being more common in sicker patients who required mechanical ventilation than in patients who did not (57 vs. 36%; p=0.09). The most common combination was TMP-SMX plus pentamidine (in eight episodes). Five patients with PCP and suspected invasive aspergillosis received TMP-SMX plus caspofungin. Outcome was available for four of them, two of whom died of PCP.
Twenty-six of 76 (34%) patients with outcome data available died of PCP. The median duration of therapy for patients who recovered from PCP was 2 days (range, 11–34 days). Paradoxical worsening in response to TMP-SMX therapy was observed in seven episodes in which patients received TMP-SMX prior to adjunctive corticosteroid therapy. In the majority of cases (91%), patients received adjunctive corticosteroid therapy (Table 1). There was a trend toward adjunctive corticosteroid therapy being more common in sicker patients who required mechanical ventilation than in patients who did not (42 vs. 0%; p=0.07). There were also trends toward administration of corticosteroids being more common in patients who eventually died of infection (100 vs. 88%, p=0.08), and tapering of corticosteroids being less common in patients who eventually died of infection (76 vs. 50%; p=0.06).
Death attributable to PCP appeared to be more common in patients with HSCT than in patients who did not undergo HSCT (48 vs. 29%; p=0.1). Mortality due to PCP was similar among patients with autologous and allogeneic transplantation.
Predictors of death due to PCP by univariate and multivariate analyses are shown in Table 2. There was a trend toward a lower absolute neutrophil count at diagnosis of infection in patients who died of PCP compared to those who survived (median 2,300 vs. 4,000 cells/ml; p=0.07). The absence of an interstitial component, either alone or combined with another radiographic pattern, was associated with death due to PCP (Table 2). There was a trend toward pleural effusion being more common in patients who died of PCP than in those who survived (10 of 26 [38%] vs. 10 of 50 [20%]; p=0.08). Spontaneous pneumothorax was significantly associated with fatal outcome (Table 2). Patients who required mechanical ventilation were 28.9 times as likely to die of PCP as were patients without such intervention (Table 2).
Discussion
In our study, the type of malignancy and the history of HSCT influenced the clinical presentation of PCP in cancer patients. In addition, our data show that PCP remains an uncommon yet important cause of life-threatening infection in cancer patients.
Among patients seen at our cancer center, the incidence of PCP did not decrease between 1990 and 2003, which might reflect the absence of major changes in both diagnostic methods and prophylactic strategies against PCP at our institution during the study period. Our finding of a higher incidence of PCP among patients with hematologic malignancies might be due primarily to a higher net state of immunosuppression caused by the underlying disease and the intensity of chemotherapy in these patients. However, our data support prior reports that a subset of patients with solid tumors develop PCP [1, 9]. The most likely explanations are the increasing use of high doses of systemic corticosteroids, especially in patients with primary brain cancer or metastatic cancer [1, 7], and the less common use of prophylaxis against PCP in this patient population.
In our series, PCP was mainly a late complication of HSCT, as previously described [16]. PCP has rarely been reported in patients who underwent autologous HSCT [8, 16]. Interestingly, we found that almost half of the patients who developed PCP after HSCT had undergone autologous transplantation. This finding might result from the different duration of PCP prophylaxis among recipients of allogeneic and autologous stem cell transplants. In fact, in a report from another transplant center where PCP prophylaxis was continued for 1 year after HSCT in all HSCT recipients, no cases of PCP in autologous transplant recipients were reported over a 7-year period [16]. Our findings confirmed many previous reports that corticosteroids are a major risk factor for PCP, particularly among patients with solid tumors [1, 3, 7, 17–19]. Our data also support the previous finding that cytomegalovirus coinfection is common in patients with PCP [5, 13]. We found that the late onset of PCP in our HSCT patients was associated with receipt of high doses of corticosteroids and with cytomegalovirus coinfection. This subset of HSCT patients might benefit from prolonged PCP prophylaxis until these risk factors subside.
Almost one-fourth of PCP cases at our center were unsuspected, indicating that a high level of suspicion is key to the early diagnosis of this infection. We found that the presence of nodular infiltrates on the initial radiographic studies was associated with a low level of suspicion of PCP. Previous studies have indicated that typical radiographic features of PCP are bilateral interstitial infiltrates; pleural effusions and pneumothorax are rarely observed [6, 20, 21]. According to our data, these last two radiographic findings may actually occur not infrequently in HSCT patients.
We found that the diagnostic yield of cytologic examination of bronchoalveolar lavage specimens for P. jiroveci was high, as previously reported in both AIDS and non-AIDS patients [17, 22–25]. Before the AIDS era, invasive procedures for diagnosing PCP were associated with a low diagnostic yield (<65%) as well as considerable morbidity and mortality [5].
PCP prophylaxis is commonly underutilized in cancer patients [18]. The cancer patients who would benefit most from preventive strategies against PCP have not been characterized in prospective trials. On the basis of retrospective series, PCP prophylaxis should be administered to cancer patients who are anticipated to require prolonged systemic corticosteroid therapy [17, 19]. Guidelines for PCP prophylaxis in this group of patients have been recently proposed [19]. Extrapolating from prophylactic strategies devised for AIDS patients, prophylaxis might be beneficial. For example, in our series, patients had very low CD4+ lymphocyte counts, and such decreased counts might suggest a risk for PCP. In a recent study that evaluated non-AIDS patients with PCP, most of whom had cancer, 91% had CD4+ lymphocytes counts lower than 300 cells/mm3 at the time of diagnosis [25].
Treatment of PCP has changed little since the 1970s [9]. TMP-SMX has become the standard therapy in cancer patients [1, 3, 9, 22, 26, 27, 28]. However, the current treatment of PCP in cancer patients is suboptimal, particularly among those with hematologic malignancies [18]. The echinocandins are novel broad-spectrum antifungal agents that inhibit the β-(1,3)-glucan synthesis, an action that damages fungal cell walls [29]. In animal models, these agents are active against the cystic form of P. jiroveci [30–32]. Caspofungin, an echinocandin, was used in combination with TMP-SMX in a very small number of patients in our series. As a result, the role of echinocandins in cancer patients with PCP remains unclear. It has been suggested that 2 weeks of antimicrobial therapy against PCP is sufficient for the majority of cancer patients [3, 9]. In our series, however, 3 weeks of treatment was associated with a better outcome.
The mortality rate from PCP in our series was high (34%), and the rate was apparently higher among patients who had undergone HSCT. Mortality rates have been reported to be as high as 50% in HSCT recipients [16]. Recent data have shown that the mortality associated with PCP in AIDS patients has declined markedly and steadily over the last decade [33], whereas the mortality rate associated with PCP in patients with cancer has remained unaltered over the last four decades [8].
In conclusion, the type of cancer and the history of HSCT may modify the clinical presentation of PCP infection in cancer patients. PCP remains a rare yet important cause of life-threatening infection in cancer patients. Several risk factors associated with fatal outcome in cancer patients with PCP have been identified. A high index of suspicion, identification of patients at high risk, and early therapy are required to improve the morbidity and mortality associated with this infection in cancer patients.
References
Sepkowitz KA, Brown AE, Telzak EE, Gottlieb S, Armstrong D (1992) Pneumocystis carinii pneumonia among patients without AIDS at a cancer hospital. JAMA 267:832–837
Morris A, Lundgren JD, Masur H, Walzer PD, Hanson DL, Frederick T et al (2004) Current epidemiology of Pneumocystis pneumonia. Emerg Infect Dis 10:1713–1720
Sepkowitz KA (1993) Pneumocystis carinii pneumonia in patients without AIDS. Clin Infect Dis 17(Suppl 2):S416–S422
Schliep TC, Yarrish RL (1999) Pneumocystis carinii pneumonia. Semin Respir Infect 14:333–343
Walzer PD, Perl DP, Krogstad DJ, Rawson PG, Schultz MG (1974) Pneumocystis carinii pnenumonia in the United States. Epidemiologic, diagnostic, and clinical features. Ann Intern Med 80:83–93
Thomas CF Jr, Limper AH (2004) Pneumocystis pneumonia. N Engl J Med 350:2487–2498
Lionakis MS, Kontoyiannis DP (2003) Glucocorticoids and invasive fungal infections. Lancet 362:1828–1838
Sepkowitz KA (2002) Opportunistic infections in patients with and patients without acquired immunodeficiency syndrome. Clin Infect Dis 34:1098–1107
Sepkowitz KA (1992) Pneumocystis carinii pneumonia among patients with neoplastic disease. Semin Respir Infect 7:114–121
Meyers JD, Pifer LL, Sale GE, Thomas ED (1979) The value of Pneumocystis carinii antibody and antigen detection for diagnosis of Pneumocystis carinii pneumonia after marrow transplantation. Am Rev Respir Dis 120:1283–1287
Kovacs JA, Hiemenz JW, Macher AM et al (1984) Pneumocystis carinii pneumonia: a comparison between patients with the acquired immunodeficiency syndrome and patients with other immunodeficiencies. Ann Intern Med 100:663–671
Russian DA, Levine SJ (2001) Pneumocystis carinii pneumonia in patients without HIV infection. Am J Med Sci 321:56–65
Limper AH, Offord KP, Smith TF, Martin WJ 2nd (1989) Pneumocystis carinii pneumonia. Differences in lung parasite number and inflammation in patients with and without AIDS. Am Rev Respir Dis 140:1204–1209
Roblot F, Godet C, Le Moal G et al (2002) Analysis of underlying diseases and prognosis factors associated with Pneumocystis carinii pneumonia in immunocompromised HIV-negative patients. Eur J Clin Microbiol Infect Dis 21:523–531
Centers for Disease Control (1993) Revised classification system for HIV infection and expanded surveillance case definition for AIDS among adolescents and adults. MMWR Morbid Mortal Wkly Rep 41:no. RR-17
Vasconcelles MJ, Bernardo MV, King C, Weller EA, Antin JH (2000) Aerosolized pentamidine as pneumocystis prophylaxis after bone marrow transplantation is inferior to other regimens and is associated with decreased survival and an increased risk of other infections. Biol Blood Marrow Transplant 6:35–43
Yale SH, Limper AH (1996) Pneumocystis carinii pneumonia in patients without acquired immunodeficiency syndrome: associated illness and prior corticosteroid therapy. Mayo Clin Proc 71:5–13
Pagano L, Fianchi L, Mele L et al (2002) Pneumocystis carinii pneumonia in patients with malignant haematological diseases: 10 years’ experience of infection in GIMEMA centres. Br J Haematol 117:379–386
Worth LJ, Dooley MJ, Seymour JF, Mileshkin L, Slavin MA, Thursky KA (2005) An analysis of the utilisation of chemoprophylaxis against Pneumocystis jiroveci pneumonia in patients with malignancy receiving corticosteroid therapy at a cancer hospital. Br J Cancer 92:867–872
Cheng VC, Hung IF, Wu AK, Tang BS, Chu CM, Yuen KY (2004) Lymphocyte surge as a marker for immunorestitution disease due to Pneumocystis jiroveci pneumonia in HIV-negative immunosuppressed hosts. Eur J Clin Microbiol Infect Dis 23:512–514
McGuinness G, Gruden JF (1999) Viral and Pneumocystis carinii infections of the lung in the immunocompromised host. J Thorac Imaging 14:25–36
Glatt AE, Chirgwin K (1990) Pneumocystis carinii pneumonia in human immunodeficiency virus-infected patients. Arch Intern Med 150:271–279
Pareja JG, Garland R, Koziel H (1998) Use of adjunctive corticosteroids in severe adult non-HIV Pneumocystis carinii pneumonia. Chest 113:1215–1224
Bigby TD (1994) Diagnosis of Pneumocystis carinii pneumonia. How invasive? Chest 105:650–652
Mansharamani NG, Balachandran D, Vernovsky I, Garland R, Koziel H (2000) Peripheral blood CD4+ T-lymphocyte counts during Pneumocystis carinii pneumonia in immunocompromised patients without HIV infection. Chest 118:712–720
Barbounis V, Aperis G, Gambletsas E et al (2005) Pneumocystis carinii pneumonia in patients with solid tumors and lymphomas: predisposing factors and outcome. Anticancer Res 25:651–655
Varthalitis I, Aoun M, Daneau D, Meunier F (1993) Pneumocystis carinii pneumonia in patients with cancer. An increasing incidence. Cancer 71:481–485
Zahar JR, Robin M, Azoulay E, Fieux F, Nitenberg G, Schlemmer B (2002) Pneumocystis carinii pneumonia in critically ill patients with malignancy: a descriptive study. Clin Infect Dis 35:929–934
Denning DW (2003) Echinocandin antifungal drugs. Lancet 362:1142–1151
Powles MA, Liberator P, Anderson J et al (1998) Efficacy of MK-991 (L-743,872), a semisynthetic pneumocandin, in murine models of Pneumocystis carinii. Antimicrob Agents Chemother 42:1985–1989
Schmatz DM, Romancheck MA, Pittarelli LA et al (1990) Treatment of Pneumocystis carinii pneumonia with 1,3-beta-glucan synthesis inhibitors. Proc Natl Acad Sci USA 87:5950–5954
Ito M, Nozu R, Kuramochi T et al (2000) Prophylactic effect of FK463, a novel antifungal lipopeptide, against Pneumocystis carinii infection in mice. Antimicrob Agents Chemother 44:2259–2262
McNeil MM, Nash SL, Hajjeh RA et al (2001) Trends in mortality due to invasive mycotic diseases in the United States, 1980–1997. Clin Infect Dis 33:641–647
Acknowledgements
We wish to thank Stephanie Deming for editorial assistance. This work was supported in part by The University of Texas M.D. Anderson Faculty E. N. Cobb Scholar Award Research Endowment to D.P.K and a grant from the Puerto Rico Cancer Center (grant no. U54 CA96297) to G.N.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Torres, H.A., Chemaly, R.F., Storey, R. et al. Influence of type of cancer and hematopoietic stem cell transplantation on clinical presentation of Pneumocystis jiroveci pneumonia in cancer patients. Eur J Clin Microbiol Infect Dis 25, 382–388 (2006). https://doi.org/10.1007/s10096-006-0149-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-006-0149-4