Abstract
In the study reported here, the diagnostic performance of two new rapid tests for the diagnosis of malaria was evaluated in symptomatic patients in a non-endemic area. Of 557 consecutive patients, 109 (19.6%) had documented malaria. For the NOW ICT MALARIA P.f./P.v. (Binax, Portland, ME, USA) and OptiMAL IT (Diamed, Cressier, Switzerland) tests, respectively, sensitivity values were 96.3% and 79.8% (P-value, 0.0001), and specificity values were 98.8% and 98.4%. The NOW ICT test did not detect two of 80 Plasmodium falciparum infections, and it generated false-positive results for five patients. The OptiMAL IT test failed to detect ten of the P. falciparum infections, and it generated seven false-positive results. The results suggest that these rapid diagnostic tests for malaria may be useful, but they cannot replace microscopic examination of blood films.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rapid diagnosis is required for the effective treatment of malaria. Currently, microscopic examination of thin or thick blood smears is widely used, but this method is time-consuming and requires an experienced microscopist for success. According to Moody [1], the mean prevalence of parasitemia among patients returning from endemic areas is between 0.1% and 0.001%. During the last decade, rapid diagnostic tests based on the detection of histidine-rich protein II (HRP-2), a soluble Plasmodium antigen, have been marketed [2, 3]. They are easy to use and self-contained, and the results are visible to the naked eye. New tests, such as NOW ICT MALARIA P.f./P.v. (Binax, Portland, ME, USA), which combines the detection of HRP-2 and aldolase [4], and OptiMAL IT (Diamed, Cressier, Switzerland), which is based on the detection of parasite-specific lactate dehydrogenase [5], have recently been developed. However, cross-reactions with rheumatoid factor [6] and other false-positive reactions of various origins, in addition to lack of sensitivity and cost considerations, have precluded widespread use of these rapid tests [3, 5]. In order to compare the diagnostic performance of these two rapid tests in a non-endemic setting, we conducted a prospective study of non-selected patients symptomatic for malaria seen in three centres in the Lyon area of France.
Patients and methods
The study was conducted from March to August 2002, and all subjects with symptoms of malaria were included. Information was collected on travel to malaria-endemic areas, chemoprophylaxis, recent episodes of fever, presenting signs and symptoms and treatment. In keeping with French Ministry of Health guidelines, outpatients were controlled on day 3 and day 7 after the onset of treatment. Standard microscopic examination of air-dried, methanol-fixed thin blood films stained with 10% buffered Giemsa was the reference method. Slides were examined with an oil-immersion lens at 1,000× magnification, for at least 20 min, by two expert microscopists in each centre. Parasite density was determined per 104 erythrocytes.
The NOW ICT test detects HRP-2, which is produced by Plasmodium falciparum trophozoites and young gametocytes, and aldolase, an enzyme of the glycolytic pathway of the four Plasmodium species, which is used as a panmalaria antigen. The appearance of both lines in the test points to infection by P. falciparum, either alone or in association with another species.
The Optimal IT test detects lactate dehydrogenase, an enzyme produced by sexual and asexual forms of Plasmodium species. The test is a new configuration of OptiMAL presented in a sealed cassette format as an individual test [5]. According to the manufacturer, the test can detect a parasite density as low as 100–200 per microliter of blood.
The two rapid tests were performed in a blinded manner and according to the manufacturer’s instructions by separate technicians at each centre after a short training period. If the results were borderline (i.e. faint or ambiguous lines), the technician was allowed to consult a third party for a consensual decision. Venous blood was collected in EDTA-coated tubes (Becton Dickinson, Franklin Lakes, NJ, USA), and the tests, which had been stored at room temperature, were performed either immediately or within 8 h, with samples being stored at 4°C.
Real-time PCR using LightCycler technology (Roche Molecular Biochemicals, Mannheim, Germany) was applied to specimens for which the two tests disagreed. The sequences used to identify the four species of Plasmodium that affect humans have been reported elsewhere [7]. Plasma from samples giving discordant results were assayed using high-pressure liquid chromatography (HPLC) for pyrimethamine, sulfadoxine, chloroquine, quinine, halofantrine and doxycycline.
All data were recorded using Excel 2000 software (Microsoft Corp., Redmond, WA, USA). Since the kinetics of target antigenemia differ between the two tests [1], the sensitivity, specificity, positive and negative predictive values of each test, and the likelihood ratios for positive and negative results were calculated using VassartStats software (http://faculty.vassar.edu/lowry/clin1.html) on patient data collected at the time of initial sampling. The MacNemar test was used to compare the sensitivity and specificity of the two rapid detection tests.
Results and discussion
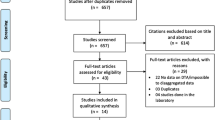
A total of 556 patients were enrolled in the study. Since positive cases were followed up and some negative patients were rechecked for malaria, a total of 685 assays were performed with both tests. The mean age of the patients was 34 years (range, 1 month to 90 years), and 57% of the patients were female. Three-quarters of the patients had visited Africa (mainly sub-Saharan Africa), 10% Asia and 6% South America. The rest of the patients had either never left Europe (7%) or provided no information on travel to malaria-endemic areas (2%). One hundred nine (19.6%) patients were diagnosed with malaria.
Table 1 shows the different species identified by thin film microscopy and the results obtained by the two commercial assays. All three methods were used on the first blood sample obtained from each patient. Table 2 shows the comparative performance of the two commercial assays. NOW ICT had a sensitivity of 96.3%, whereas OptiMAL IT had a significantly lower sensitivity of 79.8% (chi-square, 13.7; P-value, 0.0001). NOW ICT initially gave negative results for two patients infected with P. falciparum, but in one case the test became positive the following day (parasitemia <0.01%) thus ruling out the possibility of a mutation abrogating HRP-2 production [1]. Secondarily positive results have been reported previously for rapid detection tests based on HRP-2 detection [8]. With OptiMAL IT, ten false-negative results were recorded and nine of these patients had P. falciparum parasitemia above 0.01%. All ten patients reported they had not taken antimalarial drugs, and drug assays were negative for eight. OptiMAL IT was less efficient than NOW ICT for detecting sexual forms of P. falciparum and mixed infections (Table 1).
Five false-positive results were produced by NOW ICT. The corresponding patients had all returned from endemic areas, had a history of fever during the 3 weeks before admission, and had received antimalarial drugs. In three of these false-positive cases, PCR resulted positive for P. falciparum. In all cases antimalarial drug assays were negative. It is probable that these false-positive cases were due to the persistence of HRP-2, as has been reported previously [1, 3]. In contrast, OptiMAL IT gave seven false-positive results. In one case, PCR demonstrated the presence of P. vivax DNA. Five days before admission, the patient had returned from Indonesia and had started self-administered quinine therapy. In the other six cases, PCR and antimalarial assays were negative. Three of the patients had hepatic or infectious diseases. PCR negativity suggests that these false-positive results were due to interfering factors such as heterophilic antibodies [5].
Thirteen patients with P. falciparum infection were followed for at least 7 days after the onset of treatment. In 12 cases OptiMAL IT turned negative before NOW ICT, i.e. after an average of 3 days. NOW ICT remained positive longer than the reference method and was still positive on day 7 in ten patients. As parasitemia declined, the panmalaria antigen band faded and turned negative before the HRP-2 band. Our data support the view that HRP-2 leaves a trail of circulating antigens [9], while lactate dehydrogenase reflects the presence of viable parasites [10] and can be used to monitor efficacy of treatment [4, 11]. Both tests had a positive likelihood ratio greater than ten (Table 2). Thus, in a non-endemic area where the pretest probability of contracting malaria is generally low, a positive rapid test result implies a high probability of having the disease. A negative NOW ICT test result (negative likelihood ratio, 0.03) tends to rule out malaria, whereas a negative OptiMAL IT test result (negative likelihood ratio, 0.2) offers a lower degree of confidence. With regard to P. falciparum infections, our data are in keeping with previously reported results from studies conducted using the former versions of the two tests [11, 12]. For the diagnosis of P. vivax, our data support the results previously reported for NOW ICT [4] and OptiMAL IT [13]. In Australia, Playford and Walker [12] found that the former version of NOW ICT (ICT MALARIA P.f./P.v.) had a sensitivity of only 44% and did not detect cases of P. vivax parasitemia above 0.1%. One possible explanation could be a genotypic difference between P. vivax strains, since ten of our patients were infected in French Guyana.
In conclusion, the two rapid tests we evaluated should not be used as first-line methods for the diagnosis of malaria in returning travellers when microscopic examination of thick or thin blood films is an available alternative. However, they could be useful in settings where microscopists lack experience in the diagnosis of malaria.
References
Moody A (2002) Rapid diagnostic tests for malaria parasites. Clin Microbiol Rev 15:66–78
Beadle C, Long GW, Weiss WR et al (1994) Diagnosis of malaria by detection of Plasmodium falciparum HRP-2 antigen with a rapid dipstick antigen-capture assay. Lancet 343:564–568
Peyron F, Martet G, Vigier JP (1994) Dipstick antigen-capture assay for malaria detection. Lancet 343:1502–1503
Tjitra E, Suprianto S, Dyer M, Currie BJ, Anstey NM (1999) Field evaluation of the ICT malaria P.f/P.v immunochromatographic test for detection of Plasmodium falciparum and Plasmodium vivax in patients with a presumptive clinical diagnosis of malaria in eastern Indonesia. J Clin Microbiol 37:2412–2417
Moody AH, Chiodini PL (2002) Non-microscopic method for malaria diagnosis using OptiMAL®IT, a second generation dipstick for malaria pLDH antigen detection. Br J Biomed Sci 59:228–231
Jelinek T, Grobusch MP, Nothdurft HD (2000) Use of dipstick tests for the rapid diagnosis of malaria in nonimmune travelers. J Travel Med 7:175–179
De Montbrison F, Angei C, Staal A, Kaiser K, Picot S (2003) Simultaneous detection and quantification of P. falciparum in human blood samples by real time PCR. Trans R Soc Trop Med Hyg 97:387–390
Pieroni P, Mills CD, Ohrt C, Harrington MA, Kain KC (1998) Comparison of the ParaSightTM-F test and the ICT MalariaPfTM test with the polymerase chain reaction for the diagnosis of Plasmodium falciparum malaria in travellers. Trans R Soc Trop Med Hyg 92:166–169
Eisen DP, Saul A (2000) Disappearance of pan-malarial antigen reactivity using the ICT Malaria P.f/P.vTM kit parallels decline of patent parasitaemia shown by microscopy. Trans R Soc Trop Med Hyg 94:169–170
Piper R, Lebras J, Wentworth L et al (1999) Immuocapture diagnostic assays for malaria using plasmodium lactate dehydrogenase. Am J Trop Med Hyg 60:109–118
Moody A, Hunt-Cooke A, Gabbett E, Chiodini P (2000) Performance of the OptiMAL malaria antigen capture dipstick for malaria diagnosis and treatment monitoring at the Hospital for Tropical Diseases, London. Br J Haematol 109:891–894
Playford EG, Walker J (2002) Evaluation of the ICT Malaria P.f/P.v. and the OptiMAL rapid diagnostic tests for malaria in febrile returned travellers. J Clin Microbiol 40:4166–4171
Palmer CJ, Lindo JF, Klaskala WI et al (1998) Evaluation of the OptiMAL test for rapid diagnosis of Plasmodium vivax and Plasmodium falciparum malaria. J Clin Microbiol 36:203–206
Acknowledgements
We thank Laboratoires Fumouze (Levallois Perret, France) for providing the NOW ICT MALARIA P.f./P.v. reagents and Laboratoires Diamed (Cressier, Switzerland) for the OptiMAL IT reagents. All experiments conducted in the study comply with the current laws of France.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
De Monbrison, F., Gérome, P., Chaulet, J.F. et al. Comparative diagnostic performance of two commercial rapid tests for malaria in a non-endemic area. Eur J Clin Microbiol Infect Dis 23, 784–786 (2004). https://doi.org/10.1007/s10096-004-1202-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-004-1202-9