Abstract
To investigate the effects of mode of delivery and of necrotising enterocolitis on the faecal microflora, 140 infants born before 33 weeks of gestation were followed up for symptoms of necrotising enterocolitis. Stool samples for gas–liquid chromatography and culture were collected twice weekly, and, when necrotising enterocolitis was suspected, for 2 months. For each infant with necrotising enterocolitis (n=21), two control infants matched for birth weight and gestational age were selected from the remaining study population. In gas–liquid chromatography analysis, the faecal bacterial microflora of infants born via caesarean section differed significantly from the gut microflora of those born via the vaginal route. The intestinal microflora showed a significant alteration in the necrotising enterocolitis group at time of diagnosis. At the onset of necrotising enterocolitis, faecal colonisation with Enterococcus species and Candida albicans was significantly more frequent in symptomatic infants than in controls. In infants with positive blood cultures and positive intestinal biopsy cultures, concomitant stool samples revealed the same microbial pathogens. In conclusion, the intestinal microbial colonisation in preterm infants born by caesarean section differs from that in preterm infants born via the vaginal route. A significant change in faecal microbial colonisation seems to occur at the onset of necrotising enterocolitis. Pathogens detected in the stools at that time might have a causative role in the development of the disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
At birth, an infant’s gastrointestinal tract is sterile but rapidly becomes colonised with organisms from the mother and the local environment, with enterococci and members of the family Enterobacteriaceae being the predominant organisms in stools during the first days of life in full-term infants [1, 2]. Bifidobacteria then become predominant in the stools of most breast-fed infants, while Enterobacteriaceae, Bacteroides species, and clostridia remain at high levels in the stools of formula-fed infants [3, 4]. Faecal colonisation in full-term infants born by caesarean section is delayed, and infants born vaginally are more often colonised with bacteria of the Bacteroides fragilis group than those born by caesarean section [5]. It is not known whether such a difference also prevails in preterm infants.
Necrotising enterocolitis (NEC) accounts for significant morbidity and mortality among infants in neonatal intensive care units (NICUs). The role of infection in its pathogenesis is not known, but there is evidence to suggest that bacteria are involved to some degree in the process [6]. Although many organisms have been associated with NEC, most are those frequently found to colonise the intestine. Investigation by standard microbiological methods has not identified any single causative agent consistently associated with NEC [7].
In preterm infants fed mostly with formula, studies from the presurfactant era on faecal flora show a delayed colonisation with predominantly gram-negative aerobic flora and few anaerobes [8–10]. Infants who developed NEC were more likely to have faecal colonisation with aerobic gram-negative organisms than infants without NEC in the same NICU [11]. Whether this is true of preterm infants born after the introduction of surfactant treatment and fed with breast milk is not known.
The aims of this study were (i) to establish the effect of mode of delivery on the faecal microbial colonisation in preterm infants, (ii) to investigate the faecal microbial flora in preterm infants who develop or do not develop NEC, and (iii) to seek associations between findings in faecal bacterial and fungal cultures in preterm infants with NEC.
Subjects and methods
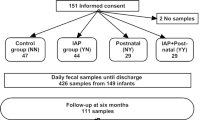
The Ethical Committee of Tampere University Hospital, Finland, approved the study protocol, and informed written consent was obtained from the parents. The original study population consisted of 140 infants born before 33 weeks of gestation. Infants were followed up prospectively for any gastrointestinal or infectious symptoms; the data collection is described in detail elsewhere [12]. Of these infants, 21 developed symptoms of NEC (the NEC group), which was diagnosed on the basis of clinical symptoms and radiographic findings in abdominal roentgenogram and classified (stages I–III) using Bell’s criteria [13]. Of these 21, 10 had NEC stage I, 5 stage II, and 6 stage III with intestinal perforation. For each infant with NEC, two control infants matched for gestational age, birth weight, and postgestational age were selected from the original study population (control group, n=42).
Stool samples for gas–liquid chromatography and for culture of dominant bacteria and fungi were collected just after the infants excreted their first stool and thereafter twice weekly on working days until discharge from the NICU or up to 2 months of age, whichever came first. Upon suspicion of NEC, abdominal roentgenograms and bacterial and fungal cultures from blood and stools were obtained. In infants with intestinal perforation, biopsy samples for cultures were obtained at laparotomy.
Management practices
In chorioamnionitis cases, the mothers received intravenous ampicillin, netilmycin, and metronidazole before delivery. Ampicillin plus netilmycin was the empiric antibiotic combination used in suspected cases of neonatal early onset sepsis. Enteral feeding was initiated on the first or second day of life, using the mother’s milk and/or banked pooled breast milk at a dosage of 20 ml/kg/day; thereafter, the same dosage was maintained. Partial parenteral nutrition was initiated on the second day of life, and its proportion was reduced daily concomitantly with the increasing proportion of breast-milk feedings. In infants of birth weights less than 1,500 g who had achieved full feedings, breast milk was fortified with PreSemp (0.8 g protein/bag, 7 kcal energy/bag; 2.15 g PreSemp/bag, 2.15 g PreSemp/100 ml breast milk) (Semper, Stockholm, Sweden) until a weight of 2,000 g was reached. Feedings were withheld at the discretion of the attending physician in infants who did not tolerate them and/or in infants who were receiving an inotropic infusion for haemodynamic instability.
In infants diagnosed as having NEC, oral feedings were discontinued and the stomach was decompressed via a nasogastric tube. Total parenteral nutrition was administered and treatment with intravenous antibiotics was initiated, with the empiric combination most frequently used being cefotaxime, metronidazole, and netilmycin. The antibiotic combination was then, if necessary, changed according to the susceptibility of the causative organism detected in the cultures obtained at the onset of NEC symptoms.
Gas–liquid chromatography of the stool samples
Stool samples were stored at −70°C and gas–liquid chromatography (GLC) analysis subsequently performed at the Department of Medical Microbiology at the University of Turku, Finland. GLC analysis was used to evaluate the bacterial fatty-acid profiles of the samples. The bacterial material was first separated from other components and from free fatty acids of the material. This is described in detail elsewhere [14].
GLC of the bacterial cellular fatty acids was performed as described previously [15]. The bacterial mass collected was saponified, methylated, and analysed as described previously [15]. In brief, the harvested bacteria were incubated for 30 min at 100°C in 15% (w/v) NaOH in 50% aqueous methanol and then acidified to pH 2 with 6N aqueous HCl in CH3OH. The methylated fatty acids were then extracted with ethyl ether and hexane. The GLC analysis was performed with an HP6890A gas chromatograph (Hewlett-Packard, Avondale, PA, USA) with an Ultra 2 (cross-linked 5% phenyl methyl silicone) 25 m × 0.2 mm column (HP19091 B) combined with HP ChemStation analysis software. Ultra-high-purity helium was used as the carrier gas.
Bacterial and fungal cultures of stool and biopsy samples
The dominant culturable bacteria and fungi recovered from cultures were studied in the Department of Clinical Microbiology of Tampere University Hospital, Finland. Stool samples were cultured semiquantitatively on selective and nonselective agars. One to three most dominant species detected in this semiquantitative assessment were determined as the dominant culturable flora, and different colonies were counted and identified. For culture of aerobic flora, blood agar, chocolate agar, MacConkey agar, Staphylococcus medium no. 110 agar (Oxoid, UK), and DIXO agar (for yeasts) were used. For culture of anaerobic flora, egg yolk agar, and Bacteroides bile esculin agar were used. Both aerobic and anaerobic bacteria were cultured for 48 h at 37°C. Anaerobic cultures were incubated in an anaerobic cabinet (Concept 300; Ruskinn Technology, UK), and aerobic cultures were grown in a 5% CO2 atmosphere.
Blood samples for culture were injected into Bactec blood culture bottles. Biopsy samples obtained at laparotomy were cultured for aerobic flora on blood and chocolate agar and for anaerobic flora on fastidious anaerobic agar and thioglycolate agar.
Data and statistical analysis
The differences between the NEC group and the control group, both groups comprised of infants born by caesarean section and by vaginal delivery, were tested by the chi-square test and Fisher’s exact test for categorical variables and by Student’s t-test and Mann–Whitney U-test for continuous variables. The Kruskall–Wallis test and one-way analysis of variance were used for multiple comparisons. P-values <0.05 were considered statistically significant.
Sufficient numbers of stool samples were available for GLC analysis in 18 of the NEC infants. For statistical comparison, two subgroups, each consisting of 18 infants, were created from the original control group, with control group 1 matching better with the NEC infants than control group 2 with respect to gestational age and birth weight. The analysis of GLC data was based on the computerised comparisons of bacterial cellular fatty-acid profiles. Each bacterial species has a typical cellular fatty-acid composition and chromatogram (Fig. 1). The cellular fatty-acid profile of a multibacterial sample consists of cellular fatty acids of all bacteria present in the sample. A bacterial identification program previously developed to analyse GLC data was used [15].
Computer analysis was carried out as described previously [15]. The analysis of the GLC chromatograms was based on the assumption that samples with similar bacterial composition would yield identical fatty-acid profiles. The samples were compared to each other and similarity indices calculated for each sample pair. These indices were presented as correlation matrices. To calculate the statistical significance of a difference between two groups, the variation in cellular fatty-acid profiles within each group was compared to that between these groups. The variation within a group was determined by calculating the mean ± standard deviation (SD) for all paired comparisons within a given group. The variation between two groups was calculated by comparing each cellular fatty-acid profile in one group to all profiles in the other group. The mean ± SD was calculated for all of these comparisons (Fig. 2). The samples obtained from the NEC and control groups were grouped according to group allocation. The samples were also further subdivided according to the day of sampling. Finally, the variation between the groups was compared to that within the groups by calculating a z-value in order to determine the P-value from the z table [15–17].
Differences in fatty-acid profiles of stool samples obtained on different days in the NEC group. Each square point represents the mean ± SD of similarity indices. The vertical axis represents the similarity index. D1 and D2 are samples obtained before the onset of NEC. D3 is a sample obtained on the day NEC was diagnosed. D4, D5, D6, and D7 are samples obtained after NEC was diagnosed. The difference between samples D2 and D3 is statistically significant (P=0.028; for statistical analysis, see text)
Results
Characteristics of the study group
NEC developed at a median of 6 days of age (range, 2–26 days). No statistically significant differences between the NEC and the control group were found in the mode of delivery or in the antimicrobial drugs administered to the mother during delivery (Table 1). The NEC infants were statistically significantly more frequently preterm and had lower birth weights than the controls. After birth, almost all infants received antibiotics, and the duration of use was similar in both groups. The commencement of breast-milk feeding, the time at which the full dose of breast milk was reached, and the initiation of breast-milk fortifier were all statistically significantly later in the NEC group than in the control groups. In addition, the NEC infants needed assisted ventilation and oxygen supplementation and suffered haemodynamic instability significantly longer than the controls.
Gas–liquid chromatography analysis
In the analysis of the whole group, the faecal fatty-acid profiles (for an example, see Fig. 1) of infants born via the vaginal route differed statistically significantly from those of infants born by caesarean section (P=0.001).
Figure 2 shows, for the NEC group, the differences in fatty-acid profiles of stool samples obtained on each sampling day compared with the profile of the first stool sample obtained. The graph shows the difference calculated as mean ± SD of the similarity indices between individual sample pairs. In the NEC group, an increased difference from baseline prior to the onset of NEC (D1, D2) was seen in the stool fatty-acid profiles on the day when NEC was diagnosed (D3) and thereafter (D4, D5, D6, D7) (Fig. 2), with the difference between samples obtained closest to the day before the onset of NEC (D2) and those collected on the day NEC was diagnosed (D3) being statistically significant in GLC analysis, P=0.028. No such alteration and no statistically significant difference were seen in either control group.
The intergroup comparisons between the NEC group and control group 1, as well as between control groups 1 and 2, brought out no statistically significant differences in the GLC analyses of the stool samples, whereas the difference between the NEC group and control group 2 was highly significant (P<0.001).
Dominant culturable organisms and mode of delivery
A comparison of the dominant bacterial and fungal organisms in the stool samples obtained from infants born vaginally with the dominant organisms from corresponding samples obtained from infants born via caesarean section at the age of 7 and 14 days (Table 2) revealed that, at the age of 7 days, Staphylococcus species dominated both in the caesarean section infants and in those born vaginally. At the same age, Escherichia coli was significantly more frequent in the stools of vaginally born infants.
Association between necrotising enterocolitis and organisms in faecal cultures
In the cultures of stool samples obtained when NEC was diagnosed, colonisation with Enterococcus species and Candida albicans was statistically significantly more frequent in the NEC infants than in the controls (Table 3).
Five NEC infants had positive blood cultures, and the same organisms cultured from blood were detected in the stool samples obtained concomitantly when NEC was diagnosed. Of these infants, three were colonised with C. albicans, one with Serratia marcescens, and one with Staphylococcus epidermidis, the last two isolates having the same antibiotic sensitivity as the ones detected in the stool samples.
Bacterial and fungal cultures from the intestine were obtained from six infants with NEC stage III who underwent abdominal surgery. Coagulase-negative Staphylococcus species were detected in the biopsy sample of one infant. The same organism was isolated from the concomitant stool sample of this infant, but the blood culture yielded Staphylococcus aureus. Coagulase-negative Staphylococcus species and C. albicans were cultured from the intestinal biopsy sample of one infant in whom C. albicans was isolated from stool and blood samples. In the third infant, coagulase-negative Staphylococcus species, Morganella morganii, and C. albicans were isolated in the intestinal biopsy, while the corresponding stool sample yielded Staphylococcus species and M. morganii and the blood culture yielded S. epidermidis, S. aureus, C. albicans, and M. morganii. The biopsy samples from the laparotomies of the remaining three infants were culture negative, but one of them had S. epidermidis in the blood culture. C. albicans was statistically significantly more frequent in the cultures of sequentially obtained stool samples in the NEC group on sampling days 5, 8, and 12 compared to controls (Table 4).
Discussion
Two methods were used in evaluating the differences in intestinal microbial flora between infants with NEC and controls. GLC analysis of faecal bacterial cellular fatty acids was used to assess differences in the microbial flora between the groups. In computer analysis of fatty-acid profiles, the amount and significance of the difference can be calculated, but a difference between fatty-acid profiles does not directly show which bacteria account for the difference. As a technical procedure, GLC is inexpensive and rapid. The whole analysis can be automated and used to study large numbers of samples [15]. Dominant bacterial and fungal organisms cultured from the stool were used to evaluate the possible microbial aetiology of NEC and its association with the faecal microbial colonisation in preterm infants at the onset of NEC. The culture of dominant bacterial and fungal organisms in stool samples is known to involve problems in sensitivity and reproducibility, and it is laborious and unsuitable for studying large numbers of samples. Culture can detect only viable bacteria in the faeces, while the bacterial cellular fatty-acid profile reveals all the bacteria present in the sample.
To our knowledge, GLC analysis to study faecal bacterial fatty acids has not previously been applied in preterm infants. Our results by this method show that the mode of the infant’s delivery seems to influence the intestinal microflora in preterm infants. In full-term infants, qualitative microbial cultures suggest that the primary gut flora in infants born by caesarean section may be disturbed for up to 6 months after birth [5]. Qualitative microbial cultures from the stools of our preterm infants born vaginally were also somewhat different from the corresponding findings in those born via caesarean section, but the dominating species differed from those previously reported in full-term infants [5]. The selection of the culture agars used in our study, however, differed from that used in the aforementioned study on term infants [5], which precludes comparison between the studies. It was not possible to establish the duration of the effect of mode of delivery on colonisation in preterm infants in our study because stool samples from our infants were collected for only 2 months. Several questions are raised for future research regarding the possible long-term consequences of abdominal delivery in preterm infants in terms of susceptibility to NEC, later gastrointestinal symptoms, or food allergy.
The second main finding in the present study using the GLC method was that, at the onset of NEC, the bacterial composition in the stool is changed significantly compared with the corresponding composition in the same infants when they were free of any NEC symptoms. Bacterial overgrowth by a limited number of virulent species in the intestine has been found to be related to the pathogenesis of NEC [18], and increased breath hydrogen levels have been measured in NEC infants compared to preterm NICU infants without NEC [19]. It can be speculated that the change seen in the bacterial fatty-acid profiles reflects the bacterial overgrowth that occurs in the gut upon development of NEC symptoms. Mucosal damage due to ischemia might be the primary phenomenon, which increases the vulnerability of the intestine of the preterm infant. This predisposes the gut to a change in faecal microbial colonisation, which leads to the development of NEC.
The GLC profiles of bacterial cellular fatty acids in the sequential stool samples of the NEC group differed significantly from the corresponding profiles in control group 2, but not from those in control group 1. The infants in the NEC group as well as in control group 1 were of lower gestational ages and birth weights than those in control group 2. Diet has a significant effect on the composition of the intestinal microbial colonisation in adults [14], in full-term newborn infants [2, 3], and in extremely low-birth-weight infants [20], although findings of the opposite in healthy infants are also on record [21]. Feeding was initiated later in both the NEC group and control group 1 than in control group 2, and, by reason of lower birth weights, the use of breast-milk fortifier was more frequent in the first two groups compared to control group 2. It can therefore be assumed that differences in feeding schedule and in composition of food are the most probable causes of the difference found between the NEC group and control group 2. The NEC group and control group 1 were significantly slower than control group 2 to establish feeding. This can be explained by the fact that the smallest and sickest infants tolerate milk poorly, often for a prolonged time, and the caretakers thus increase the feedings cautiously because such infants are at greatest risk of developing NEC. On the other hand, NEC causes an interruption of the feedings, which causes a further delay in the advancement of enteral nutrition.
A relationship between NEC and specific pathogens has been sought, and several species, including members of the family Enterobacteriaceae, Clostridia species, and coagulase-negative staphylococci have been proposed to be associated with NEC [22–27]. The gastrointestinal flora of infants with NEC appears to be different from that of similar but uninfected infants, and temporal variations seem to occur in the resident gastrointestinal microflora of infants in an NICU environment, with concomitant variations in the incidence of NEC [28]. A simultaneous increase in the numbers of infants with faecal colonisation by enterobacteria such as E. coli and Klebsiella pneumoniae and in the numbers of infants with NEC has raised suspicion of an aetiologic role of these pathogens in the development of NEC [28]. Staphylococcus species, Enterococcus faecalis, Enterococcus species, and C. albicans were the most dominant bacterial and fungal microbes cultured from the stools of our NEC infants at the onset of symptoms. Temporal variation, previous and present antibiotic therapy, and exposure of the infants to devices, as well as the antibiotic policy used in the unit, might all have had an effect on the dominance of the microbes found in the present population.
The same pathogenic organisms with identical antibiotic susceptibility patterns were detected in both stool and blood specimens from NEC infants with positive blood cultures, which confirms similar findings in an earlier work [29]. Problems with drawing a blood sample of a sufficient amount to ensure blood for microbial cultures in the case of tiny sick infants with poor peripheral perfusion are not uncommon, and the causative agent of a serious infection might thus often remain undetected. It seems that, in NEC infants, the causative organism might be among those detected in the stool; therefore, the results of the identification and the antibiotic susceptibility testing of the dominant bacterial and fungal organisms in faecal cultures can be utilised when an empiric antibiotic combination is considered. The identification of a dominant organism in stool culture that is resistant to the usual empiric antibiotic therapy may be a stimulus to broadening the antimicrobial coverage. In NEC infants with stage III disease, i.e. intestinal perforation, the causative agents of peritonitis can obviously also be detected in the stool of the infant. Because the organisms in blood cultures were detected during NEC stage III, they can be considered probable causes of bacteraemia. Whether continuous twice-weekly surveillance of faecal bacterial colonisation, as used here, would be cost-beneficial in predicting the causative agents of NEC and other serious nosocomial infections and would be useful for follow-up of temporal variations in resident gastrointestinal microflora in the NICU needs to established in future studies.
It may be concluded that, as in full-term newborn infants, the intestinal microbial colonisation in preterm infants born by caesarean section differs from the faecal colonisation of those born via vaginal route. A significant change in the faecal microbial colonisation, suggestive of a bacterial overgrowth, seems to occur in the gut of preterm infants at the onset of NEC. Pathogens detected in the stool samples obtained from NEC patients at the onset of the symptoms might have a causative role in the development of the disease.
References
Rotimi VO, Duerden BI (1981) The development of the bacterial flora in normal neonates. J Med Microbiol 14:51–62
Yoshioka H, Iseki K, Fujita K (1983) Development and differences of intestinal flora in the neonatal period in breast-fed and bottle-fed infants. Pediatrics 72:317–321
Balmer SE, Wharton BA (1989) Diet and faecal flora in the newborn: breast milk and infant formula. Arch Dis Child 64:1672–1677
Long SS, Swenson RM (1977) Development of anaerobic fecal flora in healthy newborn infants. J Pediatr 91:298–301
Grönlund MM, Lehtonen O-P, Eerola E, Kero P (1999) Fecal microflora in healthy infants born by different methods of delivery: permanent changes in intestinal flora after caesarean delivery. J Pediatr Gastroenterol Nutr 28:19–25
Willoughby RE, Pickering LK (1994) Necrotizing enterocolitis and infection. Clin Perinatol 21:307–315
Gupta S, Morris JG, Panigrahi P, Nataro JP, Glass RI, Gewolb IH (1994) Endemic necrotizing enterocolitis: lack of association with a specific infectious agent. Pediatr Infect Dis J 13:728–734
Bell MJ, Rudinsky M, Brotherton T, Schroder K, Boxerman SB (1984) Gastrointestinal microecology in the critically ill neonate. J Pediatr Surg 19:745–751
Blakey JL, Lubitz L, Barnes GL, Bishop RF, Campbell NT, Gillam GL (1982) Development of gut colonisation in pre-term neonates. J Med Microbiol 15:519–529
Goldmann DA, Leclair J, Macone A (1978) Bacterial colonization of neonates admitted to an intensive care environment. J Pediatr 93:288–293
Bell MJ, Feigin RD, Ternberg JL, Brotherton T (1978) Evaluation of gastrointestinal microflora in necrotizing enterocolitis. J Pediatr 187:1–7
Hällström M, Koivisto A-M, Janas M, Tammela O (2003) Frequency and risk factors of necrotising enterocolitis in infants born before 33 weeks’ gestation. Acta Paediatr 92:111–113
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, Brotherton T (1978) Neonatal necrotising enterocolitis: therapeutic decisions based upon clinical staging. Ann Surg 187:1–7
Vaahtovuo J, Toivanen P, Eerola E (2001) Study of murine fecal microflora by cellular fatty acid analysis; effect of age and mouse strain. Antonie Leeuwenhoek 80:35–42
Eerola E, Lehtonen O-P (1988) Optimal data processing procedure for automatic bacterial identification by gas–liquid chromatography of cellular fatty acids. J Clin Microbiol 26:1745–1753
Peltonen R (1994) Studies on faecal microetiology with reference to diet, medication and rheumatoid arthritis. Ann Univ Turku 143:1–96
Altman DG (1991) Practical statistics for medical research. Chapman & Hall, London
Claud EC, Walker WA (2001) Hypothesis: inappropriate colonization of the premature intestine can cause neonatal necrotizing enterocolitis. FASEB J 15:1398–1403
Cheu MD, Brown DR, Rowe MI (1989) Breath hydrogen excretion as a screening test for the early diagnosis of necrotizing enterocolitis. Am J Dis Child 143:156–159
Gewolb IH, Schwalbe RS, Taciak VK, Harrison TS, Panigrahi P (1999) Stool microflora in extremely low birthweight infants. Arch Dis Child Fetal Neonatal Ed 80:167–173
Lejeune C, Bourrillon A, Boussougant Y, de Paillerets F (1984) Sequential development of the intestinal flora in newborn infants: a quantitative differential analysis. Dev Pharmacol Ther 7:138–143
Cushing AH (1983) Necrotizing enterocolitis with Escherichia coli heat-labile enterotoxin. Pediatrics 71:626–630
Millar MR, MacKay P, Levene M, Langdale V, Martin C (1992) Enterobacteriaceae and neonatal necrotising enterocolitis. Arch Dis Child 67:53–56
Bell MJ, Feigin RD, Ternberg JL (1979) Changes in the incidence of necrotizing enterocolitis associated with variation of the gastrointestinal microflora in neonates. Am J Surg 138:629–631
Powell J, Bureau MA, Pare C, Gaildry M-L, Gabana D, Patriquin H (1980) Necrotizing enterocolitis: epidemic following an outbreak of Enterobacter cloacae type 3305573 in a neonatal intensive care unit. Am J Dis Child 134:1152–1154
Kosloske AM, Ball WS, Umland E, Skipper B (1985) Clostridial necrotizing enterocolitis. J Pediatr Surg 50:155–159
Scheifele DW (1990) Role of bacterial toxins in neonatal necrotizing enterocolitis. J Pediatr 117:S44–S46
Bell MJ, Shackelford P, Feigin RD, Ternberg JL, Brotherton T (1979) Epidemiologic and bacteriologic evaluation of neonatal necrotizing enterocolitis. J Pediatr Surg 14:1–4
Roback SA, Foker J, Frantz IF, Hunt CE, Engel RR, Leonard AS (1974) Necrotizing enterocolitis: an emerging entity in the regional infant intensive care facility. Arch Surg 109:314–319
Acknowledgements
The authors thank Ms Kirsti Tuomela for excellent technical assistance and Taina Arvola, MD, PhD, for valuable comments. This study was supported by the Foundation for Pediatric Research in Finland and by the Medical Research Fund of Tampere University Hospital.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hällström, M., Eerola, E., Vuento, R. et al. Effects of mode of delivery and necrotising enterocolitis on the intestinal microflora in preterm infants. Eur J Clin Microbiol Infect Dis 23, 463–470 (2004). https://doi.org/10.1007/s10096-004-1146-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-004-1146-0