Abstract
In order to evaluate the clinical significance of Aspergillus-positive culture results from the lower respiratory tract specimens of elderly hospitalized patients, and to identify the clinical variables that differentiate between colonization and infection with Aspergillus spp. in this patient population, a retrospective study was conducted. The records of 66 elderly patients whose lower respiratory tract specimens yielded Aspergillus spp. between January 1995 and July 2000 were examined. The majority of the patients (n=61) were determined to be colonized with Aspergillus spp., and serious lung infection due to Aspergillus spp. was rare. Clinical, radiological, and microbiological data did not help differentiate between infection and colonization.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Aspergillus is a ubiquitous fungus that causes a variety of clinical manifestations in humans. These manifestations range from colonization of the respiratory tract with no clinical consequences, to aspergilloma that is mainly seen in patients with chronic cavitary lung disease. Chronic necrotizing aspergillosis is a rare infection that is seen in those who are mildly immunocompromised or who have chronic lung disease. Allergic bronchopulmonary aspergillosis, on the other hand, is a hypersensitivity reaction to Aspergillus antigens that mainly affects patients with asthma. The most serious lung infection due to Aspergillus spp. is invasive pulmonary aspergillosis (IPA), which is seen in patients who are severely immunocompromised [1].
The diagnosis of lung infection due to Aspergillus spp. is difficult, and serological tests to detect Aspergillus antigens are not commercially available. The value of isolating Aspergillus spp. from lower respiratory tract (LRT) specimens is debatable. Several reports have shown that this finding is associated with colonization in 36–91% of cases, depending on the patient population studied [2–6]. In the case of IPA, the reported sensitivity of isolating Aspergillus spp. from LRT specimens ranges from 5 to 75% [1, 3, 7, 8]. As a result of this low sensitivity, invasive procedures are commonly necessary to diagnose this serious lung infection.
Elderly individuals comprise a growing segment of hospitalized patients. They commonly have a variety of medical problems including chronic lung diseases and underlying malignancies that may predispose them to serious lung infections with Aspergillus spp. When LRT cultures of elderly patients with pulmonary problems are positive for Aspergillus spp. concerns of IPA are generally raised and extensive work up is triggered. The study presented here was conducted to evaluate the clinical significance of Aspergillus-positive culture results of LRT specimens in elderly hospitalized patients, and to identify the clinical variables that differentiate between LRT colonization and infection with Aspergillus spp. in this patient population.
Materials and methods
The records of the Pathology Department of Detroit Medical Center from January 1995 to July 2000 were searched to identify all patients who had Aspergillus spp. isolated by culture from LRT specimens, including sputa, endotracheal aspirates, and bronchoalveolar lavage (BAL). Upper respiratory tract samples such as nasal or throat swabs were not included. Patients who had Aspergillus spp. isolated on more than one occasion were counted once. At the same time, the records were searched for all patients who had histologically proven IPA. From this pool of patients, the medical records of those patients aged 65 years or older were thoroughly reviewed for demographic data, underlying illnesses, reasons for hospitalization, clinical and radiological picture, leukocyte count, other respiratory isolates, final diagnosis, treatment, and hospitalization outcome. Neutropenia was defined as a neutrophil count lower than 1,000 cells/mm3. Corticosteroid therapy was recorded if the patient had received any dose of systemic corticosteroids for at least 48 h within the month prior to the first positive LRT culture result.
Patients were diagnosed as having airway colonization when Aspergillus spp. were isolated from LRT specimens (expectorated sputum, endotracheal aspirates, or BAL), without clinical or histological evidence of invasive disease. These patients were not treated with antifungal agents, and they remained free of Aspergillus-related disease during their hospitalization period. Patients were diagnosed as having IPA when they had a compatible clinical and radiological picture, characteristic histological evidence of lung tissue invasion by the fungus, and a culture result positive for Aspergillus spp. Aspergilloma was diagnosed when a characteristic fungal ball was detected within a lung cavity by chest radiograph or computed tomography (CT), and when Aspergillus spp. was isolated from culture of LRT specimens.
Results and discussion
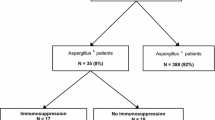
During the study period, Aspergillus spp. were isolated from the cultures of non-biopsy LRT samples of 66 elderly patients. Of these patients 61 were colonized with Aspergillus spp., 3 had IPA, and 2 had aspergilloma. None of the patients was diagnosed with chronic necrotizing aspergillosis or allergic bronchopulmonary aspergillosis. The most commonly isolated species was A. fumigatus (60%). Other Aspergillus spp. isolated included A. niger (20%), A. flavus (12%), A. terrus (2%), and unidentifiable Aspergillus spp. (6%). None of the culture specimens grew more than one Aspergillus spp. From the 66 LRT specimens examined, an Aspergillus sp. was isolated from sputum in 57 cases, BAL in 4, and both sputum and BAL in 5.
The clinical characteristics of the 61 patients who had LRT colonization by Aspergillus spp. are described in Table 1. The clinical symptoms were non-specific: 44 patients had cough, 29 had fever, 16 complained of chest pain, and none had hemoptysis. Radiological evaluation was based on chest radiograph, since CT of the chest was performed for only five of the 61 patients, and the findings were as follows: 27 patients had focal infiltrates, 12 had diffuse infiltrates, 3 had cavitary lesions, 1 had a mass, and for 18 patients the chest radiograph was normal. The final diagnoses for the patients with abnormal radiological findings were bacterial or aspiration pneumonia in 31 patients, pulmonary edema in 5, tuberculosis in 3, lung cancer in 3, and pulmonary fibrosis in 1. Aspergillus spp. were isolated from sputum in 57 patients, from BAL in 2 patients, and from both in 2 patients. Ten of the 61 patients had more than one positive sputum sample. Again, A. fumigatus was the most commonly isolated species (n=35 patients), followed by A. niger (n=13), A. flavus (n=8), A. terrus (n=1), and an unidentified Aspergillus spp. (n=4). Concomitant microorganisms were isolated from the LRT samples of 39 patients, i.e., bacteria in 23 patients, Candida spp. in 22, and mycobacteria in 3 patients (more than one microorganism was isolated from many of the patients).
Sixteen patients died during hospitalization because of conditions not related to Aspergillus infection. None of the patients with LRT colonization by Aspergillus spp. received antifungal treatment, and the treating physicians did not consider any of them to have Aspergillus lung infection. Follow-up medical records were available for 26 of the 45 patients who were discharged alive from the hospital. These patients were followed up for 1–97 months (mean ± SD, 31.2±24.4 months; median, 29 months); none had evidence of Aspergillus lung infection, and their chest radiograph findings were reported as either stable or improved.
Two patients were diagnosed with aspergilloma. Both had underlying chronic obstructive pulmonary disease and lung cancer. Chest radiograph showed a cavity with fungal ball in both cases. Aspergillus fumigatus was isolated from sputum and BAL in both cases. One of these two patients died in the hospital due to massive pulmonary hemorrhage, probably secondary to aspergilloma.
Of the 66 elderly hospitalized patients with an LRT culture positive for Aspergillus spp., three were diagnosed with IPA, based on histological confirmation of invasive disease. One patient had lung cancer, one had a hematological malignancy and was undergoing chemotherapy, and the third had HIV infection. None of these patients was neutropenic (mean leukocyte count, 6,210 cells/mm3). An Aspergillus sp. was cultured from BAL in two of these patients and from sputum and BAL in one patient. The diagnosis of IPA was confirmed by open lung biopsy in two, and pleural biopsy in one. All three patients had fever, two complained of chest pain, and one had hemoptysis. The radiological evaluation was based on CT of the chest that showed cavitary lesions in two patients and pleural effusion in one; none of the patients had a normal radiological result. The Aspergillus sp. isolated from all patients was A. fumigatus. Two patients had other organisms isolated from LRT secretions (1 Pneumocystis carinii, 1 Candida sp.). All three patients were treated with antifungal agents (1 with amphotericin B preparation alone, and 2 with amphotericin B and itraconazole). The total dose and duration of therapy could not be determined from this retrospective analysis. All three patients died in the hospital, probably as a direct result of IPA.
Patients who had lung infection due to Aspergillus spp. (aspergilloma or IPA) had higher in-hospital mortality compared to those who had LRT colonization (80 vs 26%, respectively; P=0.03, Fisher’s exact test). The number of patients with Aspergillus lung infection was too small to make a meaningful comparison between the clinical characteristics of the two groups.
The value of recovering Aspergillus spp. from culture of LRT secretions depends on the patient population. In non-immunocompromised patients, most studies have shown that this finding represents colonization or contamination. However, in immunocompromised patients, the value of LRT culture results positive for Aspergillus spp. varies significantly. Strimlan et al. [2] reported that 90% of 169 non-biopsy respiratory tract cultures positive for Aspergillus spp. were due to colonization, and most of these patients had chronic lung disease due to chronic obstructive pulmonary disease, asthma, or bronchiectasis. The remaining 10% had Aspergillus lung disease, including only 3.6% with IPA. Similar findings were reported by Treger et al. [4]. On the other hand, Nalesnik et al. [3] showed that only 36% of patients with positive LRT cultures had colonization, but 80% of the patients they studied had known risk factors for Aspergillus infection. Horvath et al. [6] also found that 49 of 78 cases with positive LRT cultures were associated with definite or probable IPA, even though the vast majority of the patients studied were at high risk for IPA. In a large prospective study of 108 consecutive patients, Yu et al. [5] found that none of the 57 non-immunocompromised patients (or patients with solid tumors or lymphoma) whose culture results were positive for Aspergillus spp. had IPA, while 21 of 54 immunocompromised patients (i.e., patients with corticosteroid therapy, transplantation, neutropenia, or leukemia) had IPA. To our knowledge, our study is the first to examine the significance of LRT cultures positive for Aspergillus spp. in elderly hospitalized patients. The results show that colonization is the most common etiology (92.5%) in this patient population. Additionally, we found that lung infection with Aspergillus spp. is rare (4.5% IPA and 3% aspergilloma).
The characteristics of patients who have LRT colonization by Aspergillus spp. are not clear from the existing literature. Yu et al. [5] reported that patients with chronic lung disease and a history of smoking were more likely to have colonization than serious Aspergillus infection. In the report by Strimlan et al. [2], 78% of patients with LRT Aspergillus colonization had chronic lung disease. Nalesnik et al. [3] observed that the frequency of cancer and other serious medical problems among patients with Aspergillus LRT colonization was significantly higher than in a non-selected population of hospitalized patients, and they attributed this to prolonged hospitalization and increased frequency of antibiotic usage. Elderly patients exhibit many of the factors that may increase their susceptibility to LRT colonization by Aspergillus spp. For example, they are more likely to have chronic lung disease, multiple medical problems, and prolonged hospitalization. In addition, the isolation of Aspergillus spp. from LRT samples may indicate that these patients are mildly immunocompromised, or it may be a marker of underlying critical illness. Indeed, more than half of our patients with LRT colonization had chronic lung disease, 26% had underlying malignancies, and almost half of them were in the intensive care unit and on mechanical ventilation when the Aspergillus spp. were isolated. Furthermore, the mortality rate in our patients with LRT colonization by Aspergillus spp. was 26%, which is much higher than the reported mortality in non-selected elderly hospitalized patients [9].
Specific radiological signs did not differentiate between LRT colonization and lung infection with Aspergillus spp. in our patient population. All patients with Aspergillus lung infection had an abnormal radiological result, while 70% of those with Aspergillus colonization of the LRT had an abnormal result; the difference between the two groups was not statistically significant. Radiological signs that are characteristic of IPA, such as the halo sign and air-crescent sign, could not be assessed in this retrospective study because in the majority of cases the radiological evaluation was based on a chest radiograph, which is insensitive and cannot detect such signs [10]. Several studies have shown that high resolution CT of the chest is the best radiological method to evaluate patients suspected of having IPA [11, 12]. Caillot et al. [12] showed that routine use of this method in the evaluation of febrile neutropenic patients suspected of having IPA, leads to earlier diagnosis and improved survival. In addition, a CT of the chest is better than chest radiograph for revealing the characteristic fungal ball present in patients with aspergilloma [13]. Therefore, it is recommended that a high resolution CT scan of the chest be performed as early as possible if there is clinical suspicion of Aspergillus lung infection.
The limitations of this study include the retrospective nature of the analysis, the fact that the majority of patients did not have a CT scan of the chest in the evaluation of their pulmonary disease, and only a small number of patients underwent histological examination of the lung. Furthermore, the study did not identify variables that could differentiate between patients with LRT colonization by Aspergillus spp. and those with more serious lung infection. A prospective study that systematically evaluates elderly patients with LRT culture results positive for Aspergillus spp., and that includes routine high resolution CT of the chest and further diagnostic studies for those with a suspicious clinical and radiological picture for IPA seems warranted.
In conclusion, the results of our study show that isolation of Aspergillus spp. by culture of LRT specimens in elderly patients is usually due to colonization. These patients commonly have underlying chronic lung disease, tend to be acutely ill, and have relatively high in-hospital mortality. Serious lung infection due to Aspergillus spp. is rare, and clinical, radiological, and microbiological data could not differentiate between infection and colonization. High clinical suspicion of IPA and further diagnostic studies are warranted in elderly hospitalized patients with an underlying immunocompromising condition who present with fever, abnormal chest radiograph, and an LRT sample yielding A. fumigatus.
References
Soubani AO, Chandrasekar PH (2002) The clinical spectrum of pulmonary aspergillosis. Chest 121:1988–1999
Strimlan CV, Dines DE, Rodgers-Sullivan RF et al (1980) Respiratory tract Aspergillus: clinical significance. Minn Med 63:25–29
Nalesnik MA, Myerowitz RL, Jenkins R et al (1980) Significance of Aspergillus species isolated from respiratory secretions in the diagnosis of invasive pulmonary aspergillosis. J Clin Microbiol 11:370–376
Treger TR, Visscher DW, Bartlett MS et al (1985) Diagnosis of pulmonary infection caused by Aspergillus: usefulness of respiratory cultures. J Infect Dis 152:572–576
Yu VL, Muder RR, Poorsattar A (1986) Significance of isolation of Aspergillus from the respiratory tract in diagnosis of invasive pulmonary aspergillosis. Results from a three-year prospective study. Am J Med 81:249–254
Horvath JA, Dummer S (1996) The use of respiratory-tract cultures in the diagnosis of invasive pulmonary aspergillosis. Am J Med 100:171–178
Soubani AO, Qureshi MA (2002) Invasive pulmonary aspergillosis following bone marrow transplantation: risk factors and diagnostic considerations. Haematologia 4:427–437
Young RC, Bennett JE, Vogel CL et al (1970) Aspergillosis: the spectrum of the disease in 98 patients. Medicine (Baltimore) 49:147–173
Landi F, Onder G, Gambassi G et al (2000) Body mass index and mortality among hospitalized patients. Arch Intern Med 160:2641–2644
Pagani JJ, Libshitz HI (1981) Opportunistic fungal pneumonias in cancer patients. Am J Roentgenol 137:1033–1039
Kuhlman JE, Fishman EK, Siegelman SS (1985) Invasive pulmonary aspergillosis in acute leukemia: characteristic findings on CT, the CT halo sign, and the role of CT in early diagnosis. Radiology 157:611–614
Caillot D, Casasnovas O, Bernard A et al (1997) Improved management of invasive pulmonary aspergillosis in neutropenic patients using early thoracic computed tomographic scan and surgery. J Clin Oncol 15:139–147
Roberts CM, Citron KM, Strickland B (1987) Intrathoracic aspergilloma: role of CT in diagnosis and treatment. Radiology 165:123–128
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Soubani, A.O., Khanchandani, G. & Ahmed, H.P. Clinical significance of lower respiratory tract Aspergillus culture in elderly hospitalized patients. Eur J Clin Microbiol Infect Dis 23, 491–494 (2004). https://doi.org/10.1007/s10096-004-1137-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-004-1137-1