Abstract
In order to explore the clinical significance and risk factors for true bacteremia caused by coagulase-negative staphylococci (CNS) other than Staphylococcus epidermidis, a retrospective cohort study of 160 patients with at least one blood culture positive for non-epidermidis CNS was performed. True bacteremia was diagnosed in 32 (20%) of the patients. On multivariate analysis the following factors were associated with true bacteremia: (i) more than one positive blood culture, (ii) presence of a central venous catheter, and (iii) methicillin resistance. The results of this study indicate that non-epidermidis CNS can cause significant bloodstream infections.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Coagulase-negative staphylococci (CNS) are recognized as increasingly important causes of bloodstream infections among hospitalized patients and are associated with significant morbidity and mortality [1–3]. CNS constitute an important part of the human skin flora and frequently contaminate blood cultures. Therefore, clinicians often face the diagnostic dilemma of having to differentiate between true bloodstream infection and contamination in patients with CNS-positive blood cultures. Consequently, antibiotics are often overused. Several studies have previously identified risk factors for true CNS bacteremia [4–6], and Staphylococcus epidermidis was shown to be the predominant pathogenic species, causing up to 90% of true CNS bloodstream infections. However, recent data demonstrate the importance of other non-epidermidis staphylococci, like Staphylococcus haemolyticus, Staphylococcus hominis, Staphylococcus warneri, or Staphylococcus lugdunensis, as causes of bacteremia and infective endocarditis [5, 7–9].
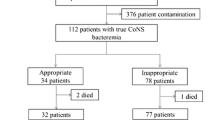
To our knowledge, no study to date has separately investigated the clinical importance of non-epidermidis staphylococcal blood isolates in a large patient cohort. We therefore conducted a retrospective cohort study of 160 patients with blood cultures positive for non-epidermidis, coagulase-negative staphylococci (NECNS) to further evaluate the clinical significance of these organisms.
Materials and methods
A retrospective cohort study of 160 adult patients (age≥18 years) with blood cultures positive for NECNS was conducted at Tulane University Hospital & Clinic in New Orleans, Louisiana, USA, between July 1997 and October 2001. Each blood culture set consisted of one aerobic and one anaerobic blood culture bottle. A blood culture set was considered positive if any one or both blood culture bottles grew NECNS. Species were identified using a MicroScan WalkAway 96 instrument (Dade MicroScan, Sacramento, CA, USA). Susceptibility to 12 different antibiotics was tested according to the guidelines of the National Committee for Clinical Laboratory Standards [10].
For each case included in the study, baseline was defined as the date of the first NECNS-positive blood culture set. All patients with one or more positive blood culture set(s) within 7 days were included and were counted as having one bacteremic episode. Any patient with blood cultures positive for more than two NECNS species or any other organism (bacterial, mycobacterial, or fungal) identified within 7 days before or after baseline was excluded from the cohort. Subsequent episodes of bacteremia with different NECNS species in the same patient and lack of complete medical records from the 3 months preceding the episode also led to exclusion. Relapse was defined as a blood culture positive for the same NECNS species more than 7 days after baseline despite appropriate antibiotic therapy.
The clinical outcome investigated was true bacteremia. A bacteremic event was defined as true bacteremia if (i) the patient had clinical symptoms as outlined in the Centers for Disease Control and Prevention’s definition of primary bloodstream infection, (ii) the blood culture results were considered and recorded as significant by the patient’s primary physician, and (iii) appropriate treatment was initiated within 24 h after the culture results were noted [11].
Demographic and clinical data at baseline were obtained for each patient by reviewing all inpatient, clinic, and emergency room records. A standardized data extraction instrument was used for recording the data. Comorbidity was assessed using the Charlson Comorbidity score [12]. The study was approved by the Tulane University Health Sciences Center Institutional Review Board.
Bivariate analysis was performed to detect a statistical association of variables with clinical outcome (P<0.05). The chi-square test and the Fisher exact test were used for categorical variables, and the Wilcoxon rank-sum test for continuous variables. Factors with P values of <0.1 on bivariate analysis were entered into a logistic regression model to detect factors independently associated with true bacteremia. All analyses were conducted using SPSS software, version 11.0 (SPSS, Chicago, USA).
Results and discussion
A total of 160 patients with 218 blood culture sets positive for NECNS species were included in our study. Patient characteristics are shown in Table 1. True bacteremia was diagnosed in 32 (20%) of the patients. Table 2 shows the different species of NECNS found in the cohort. Among the 32 episodes of true bacteremia, 29 were caused by either S. hominis or S. haemolyticus, two by S. lugdunensis, and one by S. warneri. Staphylococcus capitis and Staphylococcus auricularis were common contaminants (35%), but were not associated with true bacteremia.
Three patients with true bacteremia had more than three blood culture sets positive for the same organism (including subsequent relapses up to 15 months later), and all of these patients had long-term indwelling catheter devices. S. haemolyticus was the causative species in all three patients, and the sensitivity patterns of the isolates obtained between 3 weeks and up to 15 months after the first episode were identical. One of these patients was diagnosed with a right atrial thrombus seen on transesophageal echocardiogram (TEE) and cervical spine osteomyelitis (diagnosis confirmed by pathology, with bone cultures negative on concurrent vancomycin treatment) and was finally cured with antibiotic therapy and removal of all foreign bodies. Another patient was treated with vancomycin for suspected infective endocarditis but died of sepsis.
Clinical features that predicted true bacteremia on bivariate analysis included the following: stay in intensive care unit, prosthetic devices, history of previous antibiotic exposure, previous surgical procedure, nosocomial acquisition, more than one positive blood culture, methicillin resistance, growth in less than 36 h, resistance to more than six antibiotic classes, S. hominis or S. haemolyticus as the causative organism, and presence of a central venous catheter (P<0.05). Twenty-eight patients diagnosed with true bacteremia had central venous catheters in place at baseline. Culture of the catheter tip was subsequently performed in 19 of these patients; 10 of the cultures were negative, and 9 grew the same species as the blood cultures. Five central venous catheters were removed from patients in the contaminant group, but culture did not reveal the same NECNS organism as that obtained from the blood culture. Catheter malfunction or pericatheter signs of inflammation were documented in only four (3%) patients. The difference in the mean duration of catheter placement between the two groups was not statistically significant (P>0.2).
Resistance to methicillin was demonstrated by 39 (64%) S. hominis isolates, 27 (75%) S. haemolyticus isolates, 2 (7%) S. capitis isolates, and 2 (13%) S. auricularis isolates. Staphylococci causing true bacteremia were resistant to an average of 6.9 antibiotics and grew within 28.6 h, while staphylococci causing contamination were resistant to an average of 3.6 antibiotics and grew within 43.2 h (P<0.001).
A logistic model was created in order to determine risk factors that were independently related to outcome. More than one positive set of blood cultures (adjusted odds ratio [OR], 61.9; 95% confidence interval [95%CI], 10.0–381.6; P<0.001), presence of a central venous catheter (adjusted OR, 34.9; 95%CI, 5.6–219.3; P<0.001), and methicillin resistance (adjusted OR, 13.4; 95%CI, 2.3–78.5; P=0.004) were associated with true bacteremia.
To our knowledge, the study presented here is the first to specifically analyze risk factors for true bacteremia caused by NECNS. Thirty-two (20%) of the 160 bacteremic episodes investigated were considered to be significant. The presence of S. hominis or S. haemolyticus was a strong risk factor for true bacteremia on bivariate analysis (P<0.001). S. haemolyticus was associated with serious clinical complications including sepsis, endocarditis, and osteomyelitis in several patients.
Using logistic regression analysis, we identified three factors independently associated with the clinical outcome (P<0.01): (i) more than one positive blood culture, (ii) presence of a central venous catheter, and (iii) methicillin resistance. In our cohort, 28 of the 32 significant isolates were resistant to methicillin, compared to only 50 of the 128 contaminants. This could be explained by the highly preserved methicillin sensitivity found among the common contaminants S. capitis and S. auricularis (i.e., among 45 isolates only 4 were resistant to methicillin).
Another remarkable finding in our study was the high rate (38%) of true bloodstream infections with only one positive blood culture. This finding is consistent with results of previous studies suggesting that a single positive blood culture should not always be considered a contaminant [4–6]. No significant differences were found between patients in the true bacteremia group and patients in the contaminant group regarding their blood culture ratio. However, while 28 patients in the contaminant group had only one set of blood cultures drawn, all patients in the true bacteremia group had more than one set drawn.
Blood culture isolates from the study period were not frozen and were thus not available for pulsed-field gel electrophoresis or other methods of strain typing. Therefore, we cannot exclude that multiple positive blood cultures with the same species were the result of independent contamination or infection with different strains. However, Kim et al. [5] demonstrated a high level of clonal identity among clinically significant isolates from patients with more than one positive blood culture.
The main drawback of our study is the lack of a gold standard for the definition of CNS bacteremia. Similar to other investigators, we had to rely on clinical parameters and the evaluation by the treating physician, which could have introduced misclassification bias into our study [8]. By using strict inclusion criteria, however, we tried to reduce the risk of misinterpreting the physician’s treatment decisions. Although our strict inclusion criteria required us to exclude a large number of positive blood cultures (n=235), they also allowed us to derive a cohort whose clinical presentation could reliably be correlated to the variable of interest.
In summary, the study presented here represents the largest investigation to date of the clinical significance of and risk factors for bacteremia due to NECNS. Some members of this class, especially S. haemolyticus and S. hominis, are involved in clinically significant bacteremia with associated complications.
References
Kloos WE, Bannerman TL (1994) Update on clinical significance of coagulase-negative staphylococci. Clin Microbiol Rev 7:117–140
Rupp ME, Archer GL (1994) Coagulase-negative staphylococci: pathogens associated with medical progress. Clin Infect Dis 19:231–245
Martin MA, Pfaller MA, Wenzel RP (1989) Coagulase-negative staphylococcal bacteremia. Ann Intern Med 110:9–16
Kirchhoff LV, Sheagren JN (1985) Epidemiology and clinical significance of blood cultures positive for coagulase-negative staphylococcus. Infect Control 6:479–486
Kim SD, McDonald C, Jarvis WR et al (2000) Determining the significance of coagulase-negative staphylococci isolated from blood cultures at a community hospital: a role for species and strain identification. Infect Control Hosp Epidemiol 21:213–217
Herwaldt LA, Geiss M, Kao C et al (1996) The positive predictive value of isolating coagulase-negative staphylococci from blood cultures. Clin Infect Dis 22:14–20
Perl TM, Krüger WA, Houston A et al (1999) Investigation of suspected nosocomial clusters of Staphylococcus haemolyticus infections. Infect Control Hosp Epidemiol 20:128–131
Kamath U, Singer C, Isenberg HD (1992) Clinical significance of Staphylococcus warneri bacteremia. J Clin Microbiol 30:261–264
Patel R, Piper KE, Rouse MS (2000) Frequency of isolation of Staphylococcus lugdunensis among staphylococcal isolates causing endocarditis: a 20-year experience. J Clin Microbiol 38:4262–4263
National Committee for Clinical Laboratory Standards (2000) Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. Approved standard M7-A5. NCCLS, Wayne, PA
Garner JS, Jarvis WR, Emori TG et al (1988) CDC definitions for nosocomial infections. J Infect Control 16:128–140
Charlson ME, Pompei P, Ales KL et al (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Mirrett S, Weinstein MP, Reimer LG et al (2001) Relevance of the number of positive bottles in determining clinical significance of coagulase-negative staphylococci in blood cultures. J Clin Microbiol 39:3279–3281
Ponce de Leon S, Wenzel RP (1984) Hospital acquired-bloodstream infections with Staphylococcus epidermidis: review of 100 cases. Am J Med 77:639–644
Dominguez-de Villota E, Algora-Weber A, Millan I et al (1987) Early evaluation of coagulase-negative staphylococcus in blood samples of intensive care unit patients: a clinically uncertain judgment. Intensive Care Med 13:390–394
Acknowledgments
We would like to thank Megan O’Brien, for statistical advice. We are grateful to Chantelle Mitchell for her essential help in establishing the database.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ruhe, J., Menon, A., Mushatt, D. et al. Non-epidermidis coagulase-negative staphylococcal bacteremia: clinical predictors of true bacteremia. Eur J Clin Microbiol Infect Dis 23, 495–498 (2004). https://doi.org/10.1007/s10096-004-1134-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-004-1134-4