Abstract.
The aim of this prospective study was to compare patient characteristics, clinical data, and evolution of Legionella pneumophila pneumonia according to the duration of Legionella urinary antigen excretion. Urine samples from 61 patients with Legionella pneumonia diagnosed by detection of urinary antigen were obtained periodically until urinary antigen could no longer be detected. Cases were divided into two groups based on the duration of urinary antigen excretion: group I (46 patients, <60 days) and group II (15 patients, ≥60 days). Groups were compared for patient characteristics, clinical data, and evolution of pneumonia. Antigen excretion ≥60 days was observed significantly more frequently in immunosuppressed patients (P=0.001) in whom the time to apyrexia was >72 h (P=0.002), although only the time to apyrexia remained significant on multivariate analysis (P=0.006). In conclusion, the duration of Legionella urinary antigen excretion was <60 days in most patients but was longer in immunosuppressed patients with a longer time to defervescence of fever.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
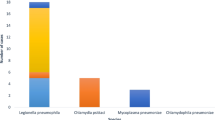
Legionella pneumophila has become an increasingly more common cause of community- and hospital-acquired pneumonia [1, 2]. The introduction into clinical practice of an assay to detect Legionella pneumophila antigen in urine has increased the rate of this etiological diagnosis in the last decade [3, 4, 5, 6, 7]. Moreover, at present, detection of urinary antigen is the diagnostic test used in more than 90% of the cases of Legionella pneumonia [8].
The Legionella urinary antigen assay is a highly sensitive and specific rapid test for diagnosis of Legionella pneumonia serogroup 1. Concentration of the urine by selective ultrafiltration may elevate the utility of this test because it increases sensitivity (nearly 20%) of the test without causing a decrease in specificity [9, 10, 11]. Excretion of urinary antigen may persist in some patients after specific antibiotic therapy [12, 13], although, to date, a prospective study using a validated commercial test has not been published.
The aim of this study was to determine the duration of excretion of Legionella pneumophila serogroup 1 antigen in urine in a large population of patients with Legionella pneumonia and to analyze the factors related to prolonged excretion of urinary antigen.
Patients and Methods
Patients
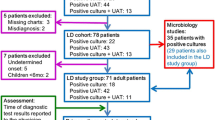
From September 1997 to September 2000, 106 patients were diagnosed with Legionella pneumonia on the basis of a positive urinary antigen assay (Legionella urinary antigen enzyme immunoassay; Binax, USA). Sixty-one of these patients were included in the study. The inclusion criteria were as follows: (i) diagnosis of Legionella pneumonia by the urinary antigen test, and (ii) the possibility to perform patient follow-up, including periodic collection of urine samples until negativity of the test, in the hospital's outpatient clinic. Patients with a previous episode of Legionella pneumonia were excluded.
Urine Samples
Urine samples from each patient were obtained monthly for the first 4 months after diagnosis of pneumonia and every 2 months thereafter until test negativity. A fresh urine specimen was concentrated 25 times by selective ultrafiltration (Minicon B15; Amicon, USA) and tested by enzyme immunoassay (Legionella urinary antigen enzyme immunoassay; Binax, USA) as described elsewhere [9, 10].
Variables Studied
In each case the following data were collected: (i) characteristics of the patients, i.e. age, sex, and risk factors (smoking; alcoholism; underlying diseases, including neoplasm, chronic obstructive pulmonary disease, diabetes, heart failure, HIV infection, chronic renal failure, renal transplantation, and liver disease; and pharmacological immunosuppression, including corticoids, chemotherapy, and other drugs); (ii) specific characteristics of pneumonia related to prognosis, i.e. nosocomial/community acquisition, delay in treatment, radiological extension, and treatment with quinolones versus macrolides; and (iii) data related to the evolution of pneumonia, i.e. time to apyrexia, local and systemic complications, and relapse of pneumonia.
Definitions of Variables
A patient was considered a smoker if he or she had smoked more than one pack per day within the last 5 years. Alcoholism was defined as consumption of ≥80 g of alcohol per day within the last 5 years. Immunosuppression (pharmacological) refers to treatment with chemotherapy, steroids, or other drugs. Steroid use refers to treatment with >60 mg of prednisone per day over a period of >2 weeks or treatment with >5 mg/day for more than 3 weeks in the last month or since the diagnosis of pneumonia. Chemotherapy refers to treatment with cytotoxic drugs, not including steroid therapy. Nosocomial pneumonia was defined as the onset of pneumonia more than 72 h after admission. Community-acquired pneumonia was defined as presentation to hospital with pneumonia or its development within 72 h of admission. Delay of treatment was defined as the number of days from the onset of illness (fever, if present) to administration of appropriate antibiotic therapy. Time to apyrexia was defined as the hours of fever following the initiation of appropriate antibiotic treatment. Relapse (possible) of Legionella pneumonia was defined as the reappearance of signs and symptoms of pneumonia accompanied by the persistence of urinary antigen after the course of antibiotic treatment had been completed, with no other demonstrated etiology.
Division of Patients into Groups
Patients were divided into two groups based on the duration of urinary antigen excretion. Group I comprised 46 patients with Legionella urinary antigen excretion of less than 60 days, and group II comprised 15 patients with antigen excretion of 60 days or more.
Statistical Analysis
The data collected from each patient were entered in a database (Dbase IV for Windows) and therewith analyzed by means of a statistical program for personal computers (SPSS, version 8.0). Categorical variables were analyzed by univariate analysis using the chi-square method or Fisher's exact test with or without Yates' correction, as appropriate. The Student's t test was used for comparison of continuous variables. Variables with statistical significance were examined in a multivariate logistic regression analysis. In all analyses, the level of significance was set at a P value of 0.05.
Results
Duration of Legionella Urinary Antigen Excretion
The test for detection of Legionella pneumophila serogroup 1 urinary antigen became negative in the first 2 months after the diagnosis of pneumonia in 46 (75.4%) cases; in 28 (45.9%) of these cases, it became negative within the first month after diagnosis. The remaining 15 (24.6%) patients were still positive for excretion of Legionella urinary antigen at 2 months post diagnosis; of these, 5 (8.1%) continued to test positive for 3 or more months (Fig. 1).
Demographics and Risk Factors of the Patients
We did not observe statistically significant differences in age, sex, smoking habits, alcohol intake, or underlying diseases between the two groups (Table 1). On the other hand, patients who excreted Legionella urinary antigen longer than 2 months had received immunosuppressive drugs significantly more frequently (P<0.001), including corticoids (P=0.003) and chemotherapy (P=0.008).
Characteristics of Pneumonia Related to Prognosis and Evolution of Illness
Bilateral pneumonia and a delay in treatment were more frequent in patients who excreted Legionella urinary antigen for more than 2 months (3/15, 20% vs. 5/46, 10.9% of the cases and 7/15, 46.7% vs. 25/46, 30.4%, respectively), although these differences were not statistically significant on univariate analysis. We did not find any differences between the groups regarding nosocomial acquisition (25/46, 54.3% vs. 4/15, 26.7%) or treatment with quinolones versus erythromycin (25/46, 54.3% vs. 8/15, 53.3%).
Time to apyrexia longer than 72 h after the initiation of treatment was significantly more frequent in patients who excreted Legionella urinary antigen for more than 2 months (6/13, 46.2% vs. 2/40, 5%; P=0.002). However, we did not observe differences between the two groups with regard to complications of pneumonia (7/15, 46.7% vs. 18/46, 39.1%). Possible relapses (2 cases) occurred only in patients who excreted Legionella urinary antigen for more than 2 months, and this variable was nearly significant on univariate analysis (13.3% vs. 0%; P=0.06). On multivariate analysis, only time to apyrexia >72 h remained significant (P=0.006).
Discussion
The Legionella urinary antigen test has become the most commonly used method for diagnosis of Legionella pneumonia because of its high sensitivity and specificity [1, 2, 3, 4, 5, 6, 7]. However, persistence of Legionella urinary antigen after resolution of pneumonia may limit its diagnostic value in patients with previous Legionella pneumonia. Knowledge of characteristics of patients with longer antigen excretion may be helpful in these cases.
Similar to previous observations [12, 13], antigenuria in our patients became negative within 2 months after the diagnosis of pneumonia in most cases (75%), and in the first month in nearly half (45.9%) of the patients. However, longer persistence was detected in 10% (15 cases) of the patients and in one case nearly 1 year after the diagnosis of pneumonia.
Pharmacological immunosuppression and the persistence of fever for more than 72 h after initiation of treatment were the only factors related to more prolonged excretion. Legionella is an intracellular pathogen that is able to persist in macrophages, particularly in immunosuppressed patients. Consequently, the evolution of Legionella pneumonia may be particularly influenced by the immune response of the patient. Thus, it may be speculated that the association between pharmacological immunosuppression and more prolonged excretion of Legionella urinary antigen may reflect the persistence of the microorganism at an intracellular level, even following resolution of the infection [14]. This hypothesis may explain the two possible relapses found in patients with prolonged urinary antigen excretion; however, this variable did not achieve statistical significance, probably due to the low number of cases.
The association between longer time to apyrexia and longer duration of Legionella urinary antigen excretion may indicate slow bacterial eradication, with longer persistence of the bacteria intracellularly [14]. This may occur particularly in immunosuppressed patients, in whom a longer duration of Legionella urinary antigen excretion was also observed.
Variables related to the severity of pneumonia, such as radiological extension and complications of pneumonia, or factors that may result in prolonged intracellular persistence of the microorganism, such as delay in treatment [15] and the use of bactericidal (quinolones) versus bacteriostatic (macrolides other than azithromycin) treatment [16], were not related to longer duration of Legionella urinary antigen excretion. These variables may influence antigen excretion in the acute phase (greater antigen excretion corresponds with a larger size of inoculum), but not after the resolution of pneumonia.
In conclusion, the duration of Legionella antigenuria following diagnosis of pneumonia was usually less than 2 months. However, almost 25% of the patients, most of whom were immunosuppressed and had a longer time to apyrexia, showed a longer duration of excretion. Further studies are required to determine whether the persistence of Legionella urinary antigen excretion can indicate early recurrence in immunosuppressed patients or the need to prolong treatment in such patients.
References
Ruf B, Schurmann D, Horbach I, Fehrenbach FJ, Pohle HD (1990) Prevalence and diagnosis of Legionella pneumonia: a 3-year prospective study with emphasis on application of urinary antigen detection. J Infect Dis 162:1341–1348
Yu VL (2000) Legionella pneumophila (Legionnaires' disease). In: Mandel GL, Bennett JE, Dolin R (eds) Principles and practice of infectious disease. Churchill Livingstone, Philadelphia, pp 2424–2435
Plouffe JF, File TM Jr, Breiman RF, Hackman BA, Salstrom SJ, Marston BJ, Fields BS, the Community-Based Pneumonia Incidence Study Group (1995) Reevaluation of the definition of Legionnaires' disease: use of the urinary antigen assay. Clin Infect Dis 20:1286–1291
Waterer GW, Baselski VS, Wunderink RG (2001) Legionella and community-acquired pneumonia: a review of current diagnostic tests from a clinician's viewpoint. Am J Med 110:41–48
Sopena N, Sabrià M, Pedro-Botet ML, Manterola JM, Matas L, Domínguez J, Modol JM, Tudela P, Ausina V, Foz M (1999) Prospective study of community-acquired pneumonia of bacterial etiology in adults. Eur J Clin Microbiol Infect Dis 18:852–858
Roson B, Carratala J, Verdaguer R, Dorca J, Manresa F, Gudiol F (2001) Prospective study of the usefulness of sputum Gram stain in the initial approach to community-acquired pneumonia requiring hospitalization. Clin Infect Dis 31:869–874
Modol JM, Pedro-Botet ML, Sabriá M, Gimeno JM, Prats R, Nieto J, Sopena N (1998) Environmental and clinical legionellosis in hospital in Catalonia, Spain. In: Program and abstracts, 38th Interscience Conference on Antimicrobial Agents and Chemotherapy, abstract no. K-49a
Alvarez J, Oyaga N, Escofet D, Codony F, Orcau A, Maria Oliva J (2001) Community-acquired legionellosis in the Barcelona (Spain) region between 1992 and 1999: epidemiological characteristics and diagnostic methods. Med Clin (Barc) 117:495–496
Domínguez JA, Materola JM, Blavia R, Sopena N, Belda FJ, Padilla E, Giménez M, Sabrià M, Morera J, Ausina V (1996) Detection of Legionella pneumophila serogroup 1 antigen in non-concentrated urine and concentrated by selective ultrafiltration. J Clin Microbiol 34:2334–2336
Domínguez JA, Matas L, Manterola JM, Blavia R, Sopena N, Belda FJ, Padilla E, Giménez M, Sabrià M, Morera J, Ausina V (1997) Comparison of radioimmunoassay and enzyme immunoassay kits for detection of Legionella pneumophila serogroup 1 antigen in both concentrated and non-concentrated urine samples. J Clin Microbiol 35:1627–1629
Dominguez JA, Gali N, Pedroso P, Fargas A, Padilla E, Manterola JM, Matas L (1998) Comparison of the Binax Legionella urinary antigen enzyme immunoassay (EIA) with the Biotest Legionella urine antigen EIA for detection of Legionella antigen in both concentrated and nonconcentrated urine samples. J Clin Microbiol 36:2718–2722
Stout JE, Yu VL (1997) Legionellosis. N Eng J Med 337:682–687
Kohler RB, Winn WC, Wheat LJ (1984) Onset and duration of urinary antigen excretion in Legionnaires disease. J Clin Microbiol 20:605–607
Morley JN, Smith LC, Baltch AL, Smith RP (1994) Recurrent infection due to Legionella pneumophila in a patient with AIDS. Clin Infect Dis 19:1130–1132
Health CH, Grove DI, Looke DFM (1996) Delay in appropriate therapy of Legionella pneumonia associated with increased mortality. Eur J Clin Microbiol Infect Dis 15:286–290
Edelstein PH (1999) Antimicrobial chemotherapy for Legionnaires' disease: a review. Clin Infect Dis 21 [Suppl 3]:265–276
Author information
Authors and Affiliations
Corresponding author
Additional information
This article was presented in part at the 39th Interscience Conference on Antimicrobial Agents and Chemotherapy, San Francisco, September 1999.
Rights and permissions
About this article
Cite this article
Sopena, N., Sabrià, M., Pedro-Botet, M.L. et al. Factors Related to Persistence of Legionella Urinary Antigen Excretion in Patients with Legionnaires' Disease. Eur J Clin Microbiol Infect Dis 21, 845–848 (2002). https://doi.org/10.1007/s10096-002-0839-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-002-0839-5