Abstract
Introduction
Seizure emergencies—status epilepticus and seizure clusters—require rapid evaluation and treatment. Several consensus-based guidelines support a prompt use of intravenous benzodiazepines as the first-line therapy in seizure emergencies. However, most seizure emergencies start outside the hospital settings. Until recently, approved prehospital rescue therapies were limited to rectal diazepam and buccal midazolam (Europe only).
Methods
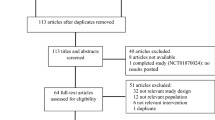
The author provides a narrative review of rescue therapies for seizure emergencies based on a comprehensive literature review (PubMed and OvidSP vendors with appropriate keywords to incorporate recent evidence) to highlight the changing landscape of seizure recue therapies.
Results
A commercial version of intranasal midazolam was approved by the FDA in 2019 for 12 ≥ years old with seizure clusters. In 2020, the FDA also approved a proprietary vitamin E solution–based diazepam nose spray to abort seizure clusters in ≥ 6 years old subjects. Other than these two new options, the author discussed two previously approved therapies: rectal diazepam and buccal midazolam. The review also includes the use of intramuscular diazepam and midazolam, clonazepam wafer, sublingual and intranasal lorazepam in seizure emergencies. Besides the availability of new therapies from successful trials in controlled settings, the real-world challenges of using rescue medicines in community settings are slowly emerging.
Discussion
With multiple options, a more robust and updated cost-effective analysis of different rescue medicines needs to be performed using effectiveness data from the literature and cost data from publicly available market prices. Further research is also ongoing to develop alternative non-intravenous treatment options for outpatient settings. Lastly, several other non-benzodiazepine drugs, such as allopregnanolone, propofol, and brivaracetam, are also currently under development for seizure emergencies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Seizure emergencies—status epilepticus (SE) and seizure clusters—require rapid evaluation and treatment. Although the definition of SE proposed by the International League Against Epilepsy (ILAE) Task Force is becoming well recognized and universally accepted, there is no standard definition for seizure clusters (Table 1). [2, 3] Impact and severity of seizure clusters can have significant inter- and individual-subject variability; however, in most situations, treatment of both these emergencies is time sensitive. Besides rapid assessment and supportive care, several consensus-based guidelines support prompt and early use of intravenous (IV) benzodiazepine (BZD) as the first-line therapy in seizure emergencies. [4,5,6] Delayed treatment of SE is associated with higher odds of death, prolonged seizure duration, greater need for continuous anesthetic infusion to abort seizures, and a higher incidence of hypotension. [7,8,9,10,11] Additionally, inadequate treatment of seizure clusters may be associated with further development of SE and an increased possibility of emergency room (ER) visits and hospitalization. Moreover, seizure clusters have a negative impact on the quality of life, predictability of daily routines, and productivity.
As most of these emergencies start outside of the medical facility, there has been significant research searching for an ideal prehospital non-IV rescue medicine that would be efficacious, safe, easy to use, inexpensive, and readily available (Table 2). By aborting a prolonged seizure promptly or preventing subsequent seizures, rescue medicines may obviate the need for further invasive interventions and minimize escalated medical care costs associated with ER visits and hospitalization. Having access to rescue medicines, patients and caregivers may experience an increased sense of control, security, and confidence in managing seizures at home. They may travel with less worry and have enhanced freedom to make long-range plans. [12] Although BZDs are universally regarded as the most appropriate first-line medicine, the preferred BZD with a particular route of administration in the out-of-hospital setting is currently open to debate. [13] Besides biological characteristics of patients, various pharmacokinetic (PK) and pharmacodynamics (PD) characteristics of different BZDs such as rapidity of action, half-life, bioavailability, efficacy in seizure suppression, and side effects, ease of preparation, and administration are vital attributes for selecting a BZD (with a specific route of administration) over others for a particular patient. This problem in selecting appropriate BZD has been worsened in recent time with the availability of two new commercial intranasal products containing midazolam (MDZ) and diazepam (DZP) besides the accessibility of rectal DZP gel in the US market since the 1990s (additionally, off-label or geographically restricted approved use of MDZ nose and oromucosal spray, clonazepam (CZP) wafer, sublingual, or IN lorazepam (LZP) has been rampant globally). A Class I evidence exists for rectal DZP and IM and IN MDZ based on results available from randomized controlled studies. On the other hand, the efficacy of IN DZP has not been directly evaluated yet, and there are no studies on CZP that meet Class I, II, or III criteria of evidence. The author followed a narrative review approach to allow comprehensive discussion of rescue therapies for seizure emergencies to highlight changing landscape of seizure rescue therapies: two previously approved therapies (rectal DZP and buccal MDZ) are introduced first, followed by two newly available treatment options—DZP and MDZ given by intramuscular (no commercially available options yet) and intranasal routes. After that, two other alternatives, clonazepam wafer and sublingual and IN LZP, are discussed.
Rectal diazepam
The presence of methyl group in the DZP contributes to its greater lipophilicity (compared to other BZDs) and the faster absorption across the tissue membranes, resulting in higher brain concentrations quickly. Before introducing commercial rectal DZP gel in the 1990s, physicians had used compounding preparations of parenteral DZP for rectal use (administered by a rubber tube). However, approval of commercially available rectal DZP gel made that practice obsolete for various reasons: difficulty with handling glass ampules containing DZP solution, long preparation time, injury risk to the patients and caregivers, potential dosing error, need to store the solution at a controlled temperature, and limited shelf life.
The rectal route has been explored since early in the research as thinner rectal epithelium can absorb DZP faster, and the rectum can handle larger volume than other transmucosal surfaces. DZP rectal gel provides the peak plasma concentration within 90 min with a bioavailability of 80–90% and compares favorably to the slow and erratic absorption of DZP suppositories. [14] Dreifuss et al. compared rectal DZP gel (2 doses in 4 h apart in children and three doses in adults 4–8 h apart to maintain target plasma concentration 150–300 ng/ml) with placebo in 91 subjects.[15]Seizure recurrence was significantly less in the DZP group (P < 0.001) both globally and separately in children and adults. The difference was apparent in 30 min after the 1st dose. The global assessment of treatment outcome (a combination of seizure frequency, seizure severity, and drug toxicity) by caregivers was significantly better in the DZP group (globally and in children but not in adults; it is unclear if an extra dose in adults caused more somnolence to minimize the benefits from seizure reduction). Cereghino et al. conducted a randomized, placebo-controlled, double-blind study of rectal DZP gel given by caregivers at home in 114 patients recruited from 29 centers. [16] DZP-treated patients had fewer seizures than the placebo group (P = 0.029), and more patients in the DZP group remained seizure-free for 12 h in the post-administration observation period. Kaplan–Meier survival curves further showed that DZP not only delayed the next seizure but prevented further seizures. Both caregiver and investigator global assessment scores showed better outcomes with DZP than placebo. The most common adverse effect was somnolence, and there was no observable effect on respiration. Furthermore, Mitchell et al. evaluated persistent efficacy and safety of recurrent use of rectal DZP at an interval of > 5 days for seizure clusters in patients with intractable epilepsy. [17] The study showed the efficacy of DZP did not decrease with recurrent administration. Approximately 77% of patients remained seizure-free for 12 h after the use of rectal DZP. There was also a significant reduction of the need for ER visits (only 3–6% patients evaluated in the ER after 1–3 doses of DZP) compared to a historical cohort of seizure cluster patients treated with placebo (13% patients required ER visit). Until recent times, rectal DZP was the only FDA-approved home medicine for seizure clusters in the USA. However, the use of rectal DZP is particularly troublesome if a seizure occurs in public places. In general, it is difficult to use, except in very young children, due to privacy issues. Administration can be specifically challenging in individuals who use wheelchairs. Though there are advantages of no need for refrigeration and IV access for administration of rectal DZP, care providers—almost universally—prefer alternative routes of medication administration. Moreover, rectal DZP can be erratically absorbed with variable plasma exposure and may take a relatively long time to reach peak concentration. DZP’s high lipid solubility results in rapid in vivo redistribution into peripheral tissues and may lead to a decrease in brain concentrations rapidly with a shorter duration of clinical effectiveness.
Buccal midazolam
Due to social and legal concerns of rectal administration, researchers continued to search for an alternative rescue medicine. MDZ has been evaluated extensively due to its comparable lipid solubility and efficacy to DZP with a faster onset of action. In 2011, the European Medicines Agency approved the prefilled MDZ oromucosal solution (2.5–10 mg) to stop prolong convulsive seizures in the age group of 3 months to 18 years of age. [18] Specific buccal formulations are available in Europe, but formulation intended primarily for injection is given buccally in most other countries.
Scott et al. reported a randomized study of 42 young patients in a residential facility with seizures > 5 min to compare the efficacy of buccal MDZ compared to rectal DZP. MDZ (75%) was noted to be at least as effective as DZP (59%, P = 0.16) in the cessation of seizures. [19] Ashrafi et al. reported an unblinded study from 2 hospitals in Tehran, Iran. [20] A total of 98 patients > 3 months old with > 5 min of seizure were exposed to either buccal MDZ or rectal DZP. In the MDZ group, the seizure was controlled in 42 out of 49 patients (82%) within 4 min, and all patients stopped seizing within 5 min. On the other hand, in the DZP group, only 24 (49%) and 40 (82%) patients had seizure cessation within 4 and 5 min, respectively. Whereas 94% of patients were satisfied with buccal dispensing, only 14% of parents were pleased with the rectal mode of administration. It was hypothesized that other than the potential difference in onset of action between MDZ and DZP, removing clothing and appropriate positioning necessary for rectal DZP might have caused an additional delay in the seizure control. Talukdar et al. reported a comparative unblinded study between buccal MDZ and IV DZP in 120 children with any seizure duration in a pediatric hospital in India. They detected no statistical difference in controlling seizures between these two groups within 5 min. [21] As expected, the MDZ group received faster administration of medicine, but after the agent’s administration, the IV DZP group had more immediate cessation of seizures. In a single-blind randomized placebo-controlled study, Mpimbaza et al. compared buccal MDZ and rectal DZP in 330 children (3 months–12 years) from Uganda with seizures longer than 5 min. [22] Malaria was the most common underlying etiology (67.3%). Treatment success (cessation of seizure activity within 10 min with no recurrence over the next 1 h) in the MDZ group was statistically superior only in a subset of patients without malaria. McIntyre et al. conducted a multicenter, randomized controlled trial to compare buccal MDZ and rectal DZP in 177 patients (> 6 months old) with active seizures in a UK hospital. [23] The positive response was attributed to the cessation of seizures within 10 min with no subsequent recurrence over the next hour. The responder rate in the MDZ group was 56% and only 27% in the DZP group.
Despite positive results in the research settings and approved indication, buccal administration can be complicated in patients with a clenched jaw (pushing the syringe’s nozzle between lips and gums may help), clonic jaw movements, or the presence of hypersalivation. Patients may also swallow a proportion of buccal medicine, causing variable PK effect and delayed onset of action. [24] Other disadvantages include unpleasant taste, risk of aspiration, caregiver injury potential (e.g., bitten finger), and the requirement for refrigeration of some liquid medicines.
Intramuscular (IM) BZD therapies
IM administration of BZDs has been researched due to the risk of blowing or spitting out of the active drug administered via other transmucosal routes and potential use in nerve agent mass casualty management. [25] Several BZDs can be given via the IM route to quickly achieve maximum concentration (Tmax). Many paramedics (emergency medical services (EMS)) prefer to use IM therapy over IV administration to leverage ease and speed of IM injection. Autoinjector (AI) can be further beneficial over conventional IM administration. IM DZP may provide higher average exposure than rectal administration. [26] Lamson et al. demonstrated in a phase I, randomized, open-label study that DZP AI produced higher plasma peaks and better absorption with less variability than DZP rectal gel in healthy adult volunteers. [27] Abou-Khalil et al. conducted a double-blind, randomized, placebo-control trial of DZP AI (administered over the mid-lateral anterior thigh) in 234 patients with acute repetitive seizures.[28]The time to the next seizure was significantly longer (P = 0.012), and the requirement of other rescue medicines was lower (P = 0.01) in the DZP group in the 12-h post-dose period. Absolute risk reduction of seizure or need of other rescue drugs was approximately 20% (55% in the placebo group vs. 35% in the DZP group). Adverse effects were similar between the two groups, with the most common being injection site pain and hemorrhage. A higher rate of accidental injection during the early trial period was improved later with further training and AI redesigning. Rogin et al. published part 2 of the study that demonstrated the long-term safety and effectiveness of DZP AI in an open-label continuation phase. [29] Out of 129 patients with refractory seizure clusters receiving 1380 AI treatments, 77.6% had no subsequent seizure or need of rescue therapy in the next 12-h period. AI was used over the bare skin but can be administered through clothes. However, the sponsor did not apply for FDA approval for an unknown reason. DZP IM injection, using a conventional syringe over the deltoid muscle, had not been that successful as it might be associated with slow and incomplete absorption. Similarly, DZP may absorb erratically following IM injection into the gluteus muscle.
A randomized, double-blind study (RAMPART (Rapid Anticonvulsant Medication Prior to Arrival Trial)) provided evidence of the non-inferiority of IM MDZ (administered by AI) to IV LZP. These rescue medicines were administered by paramedics for successful termination of clinically evident seizures at the arrival to the ER. [30, 31] Frequency of intubation, recurrent seizures, and safety outcomes were similar between the two groups, but fewer subjects in the MDZ group (P = 0.01) required hospital admission. As expected, the time needed for IM administration was shorter than the administration of IV medicine, and the onset of action was faster in the IV LZP group after the administration of medication. In a secondary analysis among pediatric patients, Welch et al. further showed similar safety and effectiveness of IM MDZ compared to IV LZP for prehospital treatment of seizure by paramedics. [32].
Intranasal midazolam (IN MDZ)
IN route is considered an attractive alternative to other BZD administration methods due to its non-invasiveness, the potential for a direct nose to brain delivery, high vascularity of the nose, relatively sizeable absorptive area, and avoidance of the first-pass metabolism. [33] However, the poor water solubility of BZDs limited the initial development of a commercial product. The solubility of MDZ, a 1, 4 BZD, is pH dependent: freely water-soluble if pH is < 4, but becomes lipid soluble with the closure of the BZD ring in physiological pH and capable of rapidly crossing the blood–brain barriers to exert its action promptly. As MDZ undergoes hydroxylation by hepatic microsomal oxidative system, IN administration has the advantage of bypassing portal circulation to accelerate systemic availability. Parenteral MDZ preparation has been used for IN administration with the atomization device to transform the liquid into tiny particle sizes. Large droplets without atomization pass through the nasopharynx and are swallowed. McMullan et al. performed a meta-analysis of 6 studies involving 774 individuals (mostly children with a maximum age of 22 years) to compare MDZ (administered by any routes) to DZP. [34] MDZ was noted to be superior to DZP (by any route) in terms of efficacy in seizure cessation. Thakker et al. conducted a RCT to compare IN MDZ (0.2 mg/kg) and IV DZP (0.3 mg/kg) in 50 children (1 month–12 years) with seizure duration > 10 min.[35]The administration of medication and seizure cessation since the arrival to the ER was significantly faster in the MDZ group; however, cessation of seizure since medication administration was faster in the DZP group. The overall efficacy of seizure cessation within 10 min was equivalent in both groups. A prehospital pediatric study of IN MDZ and rectal DZP demonstrated 19 min shorter median seizure time in the MDZ group than those who received rectal diazepam (P = 0.003). [36] Additionally, the DZP group patients had a higher risk of subsequent seizures or the need for intubation, hospitalization, or placement in the intensive care unit. Holsti et al. performed an RCT to compare IN MDZ and rectal DZP for home treatment of seizures longer than 5 min in a pediatric population.[37]The median time for seizure cessation after medication administration was faster in the MDZ group by 1.3 min. The study was underpowered to show statistical significance, and there was no detectable difference in efficacy and adverse effects between these groups.
Mahmoudian et al. conducted an RCT to compare IN MDZ (0.2 mg/kg; administered by dripping the medicine in the nostrils without the use of atomizer) with IV DZP (0.2 mg/kg) in 70 children (2 months–15 years) in a pediatric emergency department in Iran. [38] The time required to secure the IV line was not documented. IV DZP was faster to control seizure (2.94 min vs. 3.58 min; P = 0.007). Lahat et al. compared the safety and efficacy of IN MDZ (0.2 mg/kg) with IV DZP (0.3 mg/kg) in 47 children (6 months–5 years) with prolonged (> 10 min) febrile seizures. [39] As expected, children received MDZ faster than the DZP (mean 3.5 min vs. 5.5 min). The MDZ group had an overall shorter seizure duration since arrival at the hospital (6.1 min vs. 8 min). However, both medicines were effective for the cessation of seizures.
Due to the limited volume of the nasal cavity, there has been a strong interest in developing a highly concentrated IN MDZ product. Additional focus was to create a prefilled, easy to use, delivery device as the use of parenteral MDZ with atomization device can be complicated: drawing up the appropriate dose of medication from the IV vial, switching syringe tips, and preparing IN delivery with atomization device, all while one’s child continues to have ongoing seizure activity. Hardmeier et al. performed a PK/PD study using highly concentrated IN MDZ containing absorption-enhancer chitosan in 12 healthy adults and compared with IV MDZ. [40] Majority of the subjects attained maximum plasma drug concentration with increase beta band frequency changes in the EEG within 10 min of IN administration (median time to onset 5.5 and 6.9 min for 6 mg and 3 mg IN MDZ, respectively compared to 1.2 min for 5 mg IV MDZ).
A novel MDZ commercial, standardized formulation (USL261/Nayzilam) optimized for delivery as a single‐dose nasal spray had been developed in conjunction with its delivery device as a combination product. Rapid delivery of this product by IN route showed excellent absorption compared to IV MDZ in a pilot study. [41] Further phase I PK/PD, randomized, double-blind studies provided evidence of increasing exposure of MDZ with increasing IN dose from 2.5 to 7.5 mg. [42, 43] Another study demonstrated that doses up to 20 mg could be tolerated without significant adverse effects. [44] Berg et al. compared PK/PD data of USL261 (2.5 and 5 mg) between geriatric and non-geriatric adults. [45] MDZ was rapidly absorbed in both groups with a similar time to reach maximum plasma concentration; however, maximum plasma concentration is 20% higher in the geriatric population. Detyniecki et al. conducted a phase III, randomized, double-blind, placebo-controlled trial to compare 5 mg MDZ nose spray (prefilled atomizer) to placebo in 292 patients ≥ 12 years old. [46] During randomized phase, MDZ was associated with higher rate (53.7% vs. 34.4%, P = 0.0109) of treatment success (seizure termination within 10 min and no subsequent recurrence over the next 6 h). Moreover, fewer patients in the MDZ group had seizure recurrence (38.1% vs. 59.7%; P = 0.0043). Time to subsequent seizure analysis showed similar results to the pivotal rectal DZP study: early benefit evident within 30 min (as MDZ peaks in less than 10 min after IN administration) and the persistence of benefit until 24 h (perhaps due to effective termination of accelerated seizure progression phase rather than persistence of effective plasma concentration as MDZ has a short elimination half-life of 1.5–6 h). This commercial version of IN MDZ was approved by the FDA in 2019 for ≥ 12 years old with seizure clusters. [47].
Intranasal diazepam
Besides IN MDZ, DZP has been extensively investigated as a potentially good candidate for IN therapy. DZP has superior bioavailability and longer elimination half-life and duration of action compared to MDZ. Following IN administration, MDZ exhibits a faster but lower and more variable absorption compared to intranasal DZP. [48] Sperling et al. conducted an open-label, multicenter PK study of IN DZP (inactive ingredients were methyl laurate, diethylene glycol monoethyl ether, N-methyl-2-pyrrolidone, propylene glycol monocaprylate, ethanol, and water). [49] A total of 30 patients received DZP during or after a convulsive tonic–clonic seizure. Median Tmax was 45 min. Approximately 65% of patients were seizure-free during the post-dose 12-h period with good tolerance. However, this product subsequently failed to demonstrate bioequivalence with DZP rectal gel in patients with epilepsy. [50] A proprietary vitamin E (to improve solubility) solution–based DZP nose spray (Valtoco) was later evaluated. [51] Intravail technology—a patented alkylsaccharide transmucosal delivery enhancer—has been adopted for this nose spray to increase intranasal bioavailabilities with less risk of mucosal irritation. Adult bioavailability studies, PK studies, and open-label safety studies were performed to compare Valtoco with DZP rectal gel. Valtoco is 97% bioavailable, produces peak plasma concentration in 1.5 h, and elimination half time (10 mg DZP) of 49.2 h. [52] Moreover, the absorption of Valtoco was noted to be 2–fourfold less variable compared to the DZP rectal dose. Among 190 patients receiving Valtoco, the most commonly reported adverse effects were local, nasal discomfort, congestion, mild epistaxis, and dysgeusia. Other than an allergic reaction to BZDs, these nasal sprays are also contraindicated in the presence of acute angle-closure glaucoma. Valtoco has 10.5 mg benzyl alcohol as a preservative /0.1 ml and may cause the gasping syndrome in premature neonates and low birth-weight infants. Although there have not been any direct evaluation, the efficacy of IN DZP had been extrapolated from the rectal DZP experience in the clinical trial and open-label studies (Sect. 505(b)(2) of the FDA, which allows the application to use information from previous studies done by others). In 2020, the FDA approved Valtoco to terminate seizure clusters in ≥ 6 years old subjects.
There has been concern raised about nasal passage blockage by mucus and poor absorption of IN MDZ and DZP, particularly if the patient has upper respiratory tract infection or seasonal allergies. However, the infection can increase local blood flow and potentially accelerate absorption and counteract the diluting effect of nasal secretions. Although the two new FDA-approved IN formulations may mitigate privacy concern associated with rectal DZP, many children will not meet the required age criteria for these preparations. There is no head-to-head study to compare the efficacy between the 2 IN formulations. It is also unknown if one product would be better depending on the patient and/or seizure characteristics. The dose and administration protocol are different in these 2 IN products. The IN midazolam has a single 5 mg dose that can be repeated in 10 min, whereas intranasal DZP has an age- and weight-based dose (can be repeated in 4 h). The high cost and insurance approval of these two products may also be a significant barrier to afford these.
Clonazepam wafer (orally disintegrating tablet)
After oral administration, CZP is rapidly absorbed with a bioavailability of 90%. [53, 54] Maximum plasma concentration is achieved within 1–4 h. [53] CZP is highly metabolized with an elimination half-life of 30–40 h. [53] However, comparison PK data on transmucosal absorption from wafer versus absorption via the enteral route of CZP is lacking. CZP wafer can be administered between check and teeth to avoid the risk of any trauma to the individual administering the wafer. Troester et al. published an anonymous patient-survey report to evaluate the efficacy of the CZP wafer. [55] Only 56 responses were received among 381 questionnaires mailed to individuals treated with CZP over 6 years. A total of 38 of the 56 patients (68%) reported efficaciousness: the cessation of seizure within 10 min of wafer administration. Despite the lack of robust supportive studies, CZP is the preferred first-line treatment for seizure clusters (except in very young patients) among US pediatric neurologists, most likely due to its ease of administration and inexpensive cost. [56].
Sublingual and intranasal lorazepam
LZP has been extensively studied as rescue therapy with the potential for a more prolonged effect to reduce seizure recurrence due to its long half-life and slower redistribution from the brain because of lower lipid solubility. Arya et al. randomized 141 consecutive children (6–14 years old) with active convulsion in an emergency department of an Indian hospital to receive either IV or IN (without atomizer device) LZP (0.1 mg/kg, 4 mg max).[57]The primary outcome of this open-label trial was clinical seizure remission within 10 min of medication administration. The efficacy of IN LZP (83.1%) was noted to be non-inferior to IV LZP (80%). Continued seizure remission after 1 h of medication administration, the median time to achieve seizure cessation (3 min), and adverse effects were similar between these two groups. Yager et al. used sublingual LZP in 10 children with seizure clusters and noted intra- and inter-subject variability in the effective dose (0.05 to 0.15 mg/kg).[58]Ahmad et al. compared IN LZP with IM paraldehyde in 160 children (> 2 months) presented to the ED with seizures > 5 min. [59] Clinical seizure remission within 10 min of medication administration was present in 75% of the LZP group vs. 61.3% in the paraldehyde group. Approximately 10% of patients had seizure recurrence within 24 h in the LZP group and about 14% in the paraldehyde group. Malu et al. conducted an RCT to compare sublingual LZP (0.1 mg/kg) with rectal DZP (0.5 mg/kg) in 436 children (5 months–10 years) with seizures > 5 min. [60] Seizure cessation within 10 min was lower in the LZP group (56%) than the patients treated with rectal DZP (79%, P < 0.001).
It has been suggested that buccal absorption of LZP can be slower than the intake through the nasal mucosa. LZP plasma level necessary for seizure control (60–80 ng/ml) may not be achieved consistently with sublingual administration (reported to peak at 14–16 ng/ml). IN LZP is also assumed to be a less optimal candidate than IN DZP or MDZ due to its slower absorption and onset of action because of its lower lipid solubility. Some authors suggested a higher dose of non-IV LZP (8 mg irrespective of weight) to achieve the target plasma level and desired benefit. Finally, LZP has a short shelf life without refrigeration, limiting its use in the prehospital setting.
Current status and future directions
Real-world situation
The real-world benefits and challenges of rescue medicines in community settings by parents, teachers, and other caregivers are slowly emerging. Vigevano et al. reported a European retrospective observational survey–based study regarding home rescue medication use (mostly rectal DZP and buccal MDZ) for prolonged acute convulsive seizures > 5 min in non-institutionalized children (3–16 years). [61] Rescue medication use was associated with a significant reduction of seizure duration < 5 min. However, it was noted that one-third of patients did not receive rescue medicine within 5 min, and approximately one-quarter of patients did not receive rescue medication at the time of the most recent prolonged convulsion. Gainza-lein et al. conducted a cross-sectional, observational, survey-based study to understand the prehospital rescue medicine use in the pediatric population. [62] Patients with average seizures longer than 30 s and a history of SE were more likely to receive rescue medicines. However, some other specific categories associated with a high risk of seizure emergencies, such as epilepsy diagnosis at less than 2 years of age, polypharmacy with more than 3 AEDs, history of seizure clusters, or uncontrolled epilepsy, were not more likely to receive a prescription of rescue medicines. Approximately three-quarter of families preferred non-rectal medication, and even in a higher proportion in patients with typical development. Although > 85% of patients were prescribed rescue medicines, approximately two-third received training for medication administration and less than half had a seizure action plan. It was also noted that the underdosing of the rescue medicines for rectal DZP is common in pediatric patients due to the growing weight of the child, not consulting dosing chart during prescribing, and being apprehensive of adverse effects with a higher dose. In addition, traditional training (reading information sheet and/or watching online videos) is not enough to prepare patients and caregivers administering rescue medicines during an emergency with significant emotional disturbance. Practical and supervised hands-on training with targeted feedback about errors and spaced repetition may significantly reduce administration errors.[63].
Lastly, rescue medicine use outside the home, particularly in school, is more problematic for various reasons: nonavailability of the school nurse, complex legal issues, lack of written epilepsy policy in schools, lack of training for teachers to administer rescue medicines, and difficulty accessing medications in the school.
Cost-effective analysis
Cost-effective analysis of different rescue medicines in the USA was performed using effectiveness data from the literature and cost data from publicly available market prices. [64] In a study published in 2017 (not using the cost of the currently FDA-approved IN MDZ), MDZ (buccal and IN) was noted as more cost-effective than rectal DZP. Furthermore, one-way sensitivity analysis showed that only a dramatic reduction of rectal DZP price (from current > $300 to < $6) could make it the most cost-effective option. In the past, only injectable solution of MDZ had been used for buccal or IN administration (30–50 times cheaper than rectal DZP); however, now, with recent FDA approval, IN MDZ price is significantly higher (costs between $550 and $660 for a box of two 5-mg doses). The recently approved IN DZP is also similarly expensive (approximately $560 per box). One European study showed that buccal MDZ produced cost reduction with improved health-related quality of life despite the cost of buccal MDZ 10–20 times more than rectal DZP in Europe. [65] However, the estimation was limited by the subjective assessment of the real-world effectiveness by a limited number of experts and caregivers’ opinions. Despite the need for further research in cost-effectiveness, non-intravenous BZD as a group is a cost-effective option for seizure emergencies, and the choice of the agent may be dependent on several patient- and medicine-specific variables.
Future drug development
Rapidity and completeness of the absorption are governed by Fick’s law (parameters are absorptive surface area, blood flow, membrane thickness, and lipid solubility).[66]Although higher lipid solubility of small molecule drugs increases the absorption rate, the formulation of these molecules has been complicated due to their poor water solubility. Several approaches have been investigated to address this issue: co-administration of water-soluble prodrug with converting enzyme, utilization of organic co-solvents such as alcohol or glycol, use of absorption enhancers, and application of a lipid-based formula such as Vitamin E. [66] Further research is ongoing to allow a small, hand-held inhaler device to aerosolize and deliver drug deep in the lungs with a single normal breath. French et al. reported a proof of concept (phase 2A) study of this delivery technique using alprazolam, which suppressed photoparoxysmal responses in 5 white adult females. [67] Lastly, several other non-BZD drugs are currently under development for seizure emergencies, such as allopregnanolone, propofol, and brivaracetam. [68].
References
Jafarpour S, Hirsch LJ, Gaínza-Lein M, Kellinghaus C, Detyniecki K (2018) Seizure cluster: definition, prevalence, consequences, and management. Seizure
Trinka E, Cock H, Hesdorffer D et al (2015) A definition and classification of status epilepticus–report of the ILAE task force on classification of status epilepticus. Epilepsia 56(10):1515–1523
Samanta D, Garrity L, Arya R (2020) Refractory and super-refractory status epilepticus. Indian Pediatr 57(3):239–253
Glauser T, Shinnar S, Gloss D et al (2016) Evidence-based guideline: treatment of convulsive status epilepticus in children and adults: report of the guideline committee of the american epilepsy society. Epilepsy Curr 16(1):48–61
Brophy GM, Bell R, Claassen J et al (2012) Guidelines for the evaluation and management of status epilepticus. Neurocrit Care 17(1):3–23
Gaínza-Lein M, Fernández IS, Jackson M et al (2018) Association of time to treatment with short-term outcomes for pediatric patients with refractory convulsive status epilepticus. JAMA Neurol 75(4):410–418
Lambrechtsen FA, Buchhalter JR (2008) Aborted and refractory status epilepticus in children: a comparative analysis. Epilepsia 49(4):615–625
Hayashi K, Osawa M, Aihara M et al (2007) Efficacy of intravenous midazolam for status epilepticus in childhood. Pediatr Neurol 36(6):366–372
Eriksson K, Metsaranta P, Huhtala H, Auvinen A, Kuusela AL, Koivikko M (2005) Treatment delay and the risk of prolonged status epilepticus. Neurology 65(8):1316–1318
Lewena S, Young S (2006) When benzodiazepines fail: how effective is second line therapy for status epilepticus in children? Emerg Med Australas 18(1):45–50
Chin RF, Neville BG, Peckham C, Wade A, Bedford H, Scott RC (2008) Treatment of community-onset, childhood convulsive status epilepticus: a prospective, population-based study. Lancet Neurol 7(8):696–703
Seizure First Aid and Safety. https://www.epilepsy.com/learn/treating-seizures-and-epilepsy/seizure-rescue-therapies. Accessed 3/25/2021
Haut SR (2015) Seizure clusters: characteristics and treatment. Curr Opin Neurol 28(2):143–150
Diastat C-IV diastat AcuDial™ C-IV (diazepam rectal gel). https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/020648s014lbl.pdf. Accessed 2/16, 2021
Dreifuss FE, Rosman NP, Cloyd JC et al (1998) A comparison of rectal diazepam gel and placebo for acute repetitive seizures. N Engl J Med 338(26):1869–1875
Cereghino JJ, Mitchell WG, Murphy J, Kriel RL, Rosenfeld WE, Trevathan E (1998) Treating repetitive seizures with a rectal diazepam formulation: a randomized study. The North American diastat study group. Neurology 51(5):1274–1282. https://doi.org/10.1212/wnl.51.5.1274
Mitchell WG, Conry J, Crumrine P et al (1999) An open-label study of repeated use of diazepam rectal gel (diastat) for episodes of acute breakthrough seizures and clusters: safety, efficacy, and tolerance. Epilepsia 40(11):1610–1617
Tomlin S (2011) Medicines tailored for childrenâ€" the introduction of buccal midazolam. Pharm J 287(7665):161
Scott RC, Besag FM, Neville BG (1999) Buccal midazolam and rectal diazepam for treatment of prolonged seizures in childhood and adolescence: a randomised trial. Lancet 353(9153):623–626
Ashrafi MR, Khosroshahi N, Karimi P et al (2010) Efficacy and usability of buccal midazolam in controlling acute prolonged convulsive seizures in children. Eur J Paediatr Neurol 14(5):434–438
Talukdar B, Chakrabarty B (2009) Efficacy of buccal midazolam compared to intravenous diazepam in controlling convulsions in children: a randomized controlled trial. Brain Dev 31(10):744–749
Mpimbaza A, Ndeezi G, Staedke S, Rosenthal PJ, Byarugaba J (2008) Comparison of buccal midazolam with rectal diazepam in the treatment of prolonged seizures in ugandan children: a randomized clinical trial. Pediatrics 121(1):e58-64. https://doi.org/10.1542/peds.2007-0930
McIntyre J, Robertson S, Norris E et al (2005) Safety and efficacy of buccal midazolam versus rectal diazepam for emergency treatment of seizures in children: a randomised controlled trial. Lancet 366(9481):205–210
Schwagmeier R, Alincic S, Striebel H (1998) Midazolam pharmacokinetics following intravenous and buccal administration. Br J Clin Pharmacol 46(3):203–206
McDonough JH, Van Shura KE, LaMont JC, McMonagle JD, Shih T (2009) Comparison of the intramuscular, intranasal or sublingual routes of midazolam administration for the control of soman-induced seizures. Basic Clin Pharmacol Toxicol 104(1):27–34
Garnett WR, Barr WH, Edinboro LE, Karnes HT, Mesa M, Wannarka GL (2011) Diazepam autoinjector intramuscular delivery system versus diazepam rectal gel: a pharmacokinetic comparison. Epilepsy Res 93(1):11–16
Lamson MJ, Sitki-Green D, Wannarka GL, Mesa M, Andrews P, Pellock J (2011) Pharmacokinetics of diazepam administered intramuscularly by autoinjector versus rectal gel in healthy subjects. Clin Drug Investig 31(8):585–597
Abou-Khalil B, Wheless J, Rogin J et al (2013) A double-blind, randomized, placebo-controlled trial of a diazepam auto-injector administered by caregivers to patients with epilepsy who require intermittent intervention for acute repetitive seizures. Epilepsia 54(11):1968–1976
Rogin J, Wheless J, Abou-Khalil B et al (2014) Safety and effectiveness of long-term treatment with diazepam auto-injector administered by caregivers in an outpatient setting for the treatment of acute repetitive seizures. Epilepsia 55(9):1444–1451
Silbergleit R, Durkalski V, Lowenstein D et al (2012) Intramuscular versus intravenous therapy for prehospital status epilepticus. N Engl J Med 366(7):591–600
Silbergleit R, Lowenstein D, Durkalski V, Conwit R, NETT Investigators (2013) Lessons from the RAMPART study—and which is the best route of administration of benzodiazepines in status epilepticus. Epilepsia 54:74–77
Welch RD, Nicholas K, Durkalski-Mauldin VL et al (2015) Intramuscular midazolam versus intravenous lorazepam for the prehospital treatment of status epilepticus in the pediatric population. Epilepsia 56(2):254–262
Kapoor M, Cloyd JC, Siegel RA (2016) A review of intranasal formulations for the treatment of seizure emergencies. J Control Release 237:147–159
McMullan J, Sasson C, Pancioli A, Silbergleit R (2010) Midazolam versus diazepam for the treatment of status epilepticus in children and young adults: a meta-analysis. Acad Emerg Med 17(6):575–582
Thakker A, Shanbag P (2013) A randomized controlled trial of intranasal-midazolam versus intravenous-diazepam for acute childhood seizures. J Neurol 260(2):470–474
Holsti M, Sill BL, Firth SD, Filloux FM, Joyce SM, Furnival RA (2007) Prehospital intranasal midazolam for the treatment of pediatric seizures. Pediatr Emerg Care 23(3):148–153. https://doi.org/10.1097/PEC.0b013e3180328c92
Holsti M, Dudley N, Schunk J et al (2010) Intranasal midazolam vs rectal diazepam for the home treatment of acute seizures in pediatric patients with epilepsy. Arch Pediatr Adolesc Med 164(8):747–753
Mahmoudian T, Zadeh MM (2004) Comparison of intranasal midazolam with intravenous diazepam for treating acute seizures in children. Epilepsy Behav 5(2):253–255
Lahat E, Goldman M, Barr J, Bistritzer T, Berkovitch M (2000) Comparison of intranasal midazolam with intravenous diazepam for treating febrile seizures in children: prospective randomised study. BMJ 321(7253):83–86. https://doi.org/10.1136/bmj.321.7253.83
Hardmeier M, Zimmermann R, Rüegg S et al (2012) Intranasal midazolam: pharmacokinetics and pharmacodynamics assessed by quantitative EEG in healthy volunteers. Clin Pharmacol Ther 91(5):856–862
Bancke LL, Dworak HA, Rodvold KA, Halvorsen MB, Gidal BE (2015) Pharmacokinetics, pharmacodynamics, and safety of USL 261, a midazolam formulation optimized for intranasal delivery, in a randomized study with healthy volunteers. Epilepsia 56(11):1723–1731
Altman H, Dworak H, Halvorsen M (2013) Safety and pharmacodynamics of USL261, a novel formulation of midazolam optimized for intranasal administration, in subjects with epilepsy. Epilepsy Curr 13(Suppl. 1):164
Hayes R, Bancke L, Halvorsen M (2013) Pharmacokinetics of USL261, a novel formulation of intranasal midazolam optimized for intranasal administration, in subjects with epilepsy. Epilepsy Curr 13(Suppl. 1):167
Study to Evaluate the Safety and Efficacy of USL261(intranasal Midazolam) in Patients with Seizure Clusters. https://clinicaltrials.gov/ct2/show/NCT01390220. Accessed 2/16/21
Berg AK, Myrvik MJ, Van Ess PJ (2017) Pharmacokinetics, pharmacodynamics, and tolerability of USL261, midazolam nasal spray: randomized study in healthy geriatric and non-geriatric adults. Epilepsy Behav 71:51–59
Detyniecki K, Van Ess PJ, Sequeira DJ, Wheless JW, Meng T, Pullman WE (2019) Safety and efficacy of midazolam nasal spray in the outpatient treatment of patients with seizure clusters—a randomized, double-blind, placebo-controlled trial. Epilepsia 60(9):1797–1808
Prime B. UCB announces NAYZILAM®(midazolam) nasal spray now approved by FDA to treat intermittent, stereotypic episodes of frequent seizure activity in people living with epilepsy in the US.https://www.cureepilepsy.org/news/.Accessed 2/16/2021
Boddu SH, Kumari S (2020) A short review on the intranasal delivery of diazepam for treating acute repetitive seizures. Pharmaceutics 12(12):1167
Sperling MR, Haas KF, Krauss G et al (2014) Dosing feasibility and tolerability of intranasal diazepam in adults with epilepsy. Epilepsia 55(10):1544–1550
Acorda to discontinue development of PLUMIAZ for treatment of epilepsy seizure clusters. https://ir.acorda.com/investors/investor-news/investor-news-details/2016/Acorda-to-Discontinue-Development-of-PLUMIAZ-for-Treatment-of-Epilepsy-Seizure-Clusters/default.aspx. Accessed 2/16, 2021
Hogan RE, Tarquinio D, Sperling MR et al (2020) Pharmacokinetics and safety of VALTOCO (NRL-1; diazepam nasal spray) in patients with epilepsy during seizure (ictal/peri-ictal) and nonseizure (interictal) conditions: a phase 1, open-label study. Epilepsia 61(5):935–943
Valtoco prescribing data. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/211635s000lbl.pdf. Accessed 2/16, 2021
Crevoisier C, Delisle MC, Joseph I, Foletti G (2003) Comparative single-dose pharmacokinetics of clonazepam following intravenous, intramuscular and oral administration to healthy volunteers. Eur Neurol 49(3):173–177. https://doi.org/10.1159/000069089
Greenblatt DJ, Miller LG, Shader RI (1987) Clonazepam pharmacokinetics, brain uptake, and receptor interactions. J Clin Psychiatry 48(Suppl):4–11
Troester MM, Hastriter EV, Ng Y (2010) Dissolving oral clonazepam wafers in the acute treatment of prolonged seizures. J Child Neurol 25(12):1468–1472
Wallace A, Wirrell E, Payne E (2019) Seizure rescue medication use among US pediatric epilepsy providers: a survey of the pediatric epilepsy research consortium. J Pediatr 212:111–116
Arya R, Gulati S, Kabra M, Sahu JK, Kalra V (2011) Intranasal versus intravenous lorazepam for control of acute seizures in children: a randomized open-label study. Epilepsia 52(4):788–793
Yager JY, Seshia SS (1988) Sublingual lorazepam in childhood serial seizures. Am J Dis Child 142(9):931–932
Ahmad S, Ellis JC, Kamwendo H, Molyneux E (2006) Efficacy and safety of intranasal lorazepam versus intramuscular paraldehyde for protracted convulsions in children: an open randomised trial. Lancet 367(9522):1591–1597
Malu CKK, Kahamba DM, Walker TD et al (2014) Efficacy of sublingual lorazepam versus intrarectal diazepam for prolonged convulsions in sub-saharan africa. J Child Neurol 29(7):895–902
Vigevano F, Kirkham FJ, Wilken B et al (2018) Effect of rescue medication on seizure duration in non-institutionalized children with epilepsy. Eur J Paediatr Neurol 22(1):56–63
Gaínza-Lein M, Benjamin R, Stredny C, McGurl M, Kapur K, Loddenkemper T (2017) Rescue medications in epilepsy patients: a family perspective. Seizure 52:188–194
Schumacher PM, Kaune A, Merkenschlager A et al (2018) Optimizing parents’ performance in anticonvulsant rescue medication administration. Epilepsy Behav 84:37–43
Sánchez Fernández I, Gaínza-Lein M, Loddenkemper T (2017) Nonintravenous rescue medications for pediatric status epilepticus: a cost-effectiveness analysis. Epilepsia 58(8):1349–1359
Lee D, Gladwell D, Batty AJ, Brereton N, Tate E (2013) The cost effectiveness of licensed oromucosal midazolam (buccolam®) for the treatment of children experiencing acute epileptic seizures: an approach when trial evidence is limited. Pediatr Drugs 15(2):151–162
Maglalang PD, Rautiola D, Siegel RA et al (2018) Rescue therapies for seizure emergencies: new modes of administration. Epilepsia 59:207–215
French JA, Wechsler R, Gelfand MA et al (2019) Inhaled alprazolam rapidly suppresses epileptic activity in photosensitive participants. Epilepsia 60(8):1602–1609
Zolkowska, D., Wu, C. Y., & Rogawski, M. A. (2021). Intranasal Allopregnanolone Confers Rapid Seizure Protection: Evidence for Direct Nose-to-Brain Delivery. Neurotherapeutics, 18(1), 544–555.
Funding
Debopam Samanta is supported by the Translational Research Institute (TRI), grant UL1 TR003107 through the National Center for Advancing Translational Sciences of the National Institutes of Health (NIH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
None.
Informed consent
This article does not contain any studies involving human participants performed by the author.
Conflict of interest
The author declares no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Samanta, D. Rescue therapies for seizure emergencies: current and future landscape. Neurol Sci 42, 4017–4027 (2021). https://doi.org/10.1007/s10072-021-05468-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-021-05468-9