Abstract
Levodopa is widely used to treat Parkinson’s disease (PD), and its long-term therapy may induce dyskinesia in a dose-dependent manner. However, the threshold dose with a relatively low risk for dyskinesia has not been determined. Demographic, clinical profiles and detailed information of dopaminergic drugs were recorded for 403 PD patients in treatment with levodopa. Variables were compared between dyskinesia and non-dyskinesia groups. Logistic regression analysis was used to assess the association between levodopa dose–related variables and dyskinesia. Receiver operating characteristic curve and decision tree classification model were used to investigate the cut-off value of levodopa dose to best separate the dyskinesia group from the non-dyskinesia group. Patients with dyskinesia tended to have a lower weight and age at onset, higher percentage of female and wearing-off, longer duration of disease and levodopa treatment, higher H-Y stage and MDS-UPDRS Part III score, and higher levodopa dose and levodopa equivalent dose than those without dyskinesia. After adjusted for demographical and clinical variables, levodopa dose–related factors (daily dose, cumulative dose, and weight-adjusted dose) were still associated with dyskinesia. Both the receiver operating characteristic and decision tree classification analysis indicated that patients who have taken levodopa dose ≤ 400 mg per day may be associated with a reduced risk for dyskinesia. In conclusion, we evaluated the thresholds of levodopa treatment with a relatively low risk for dyskinesia. These data should be considered for prevention and management of dyskinesia in patients with PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease (PD) is a neurodegenerative disorder that clinically manifests as a combination of motor and non-motor symptoms [1, 2]. To date, levodopa is the most widely used treatment for PD, but its long-term therapy may induce dyskinesia [3, 4]. Multiple studies have suggested that 8–45% of PD patients experienced dyskinesia after 4–6 years of treatment [5, 6]. In China, a multicenter study reported a 10.3% prevalence rate of dyskinesia among patients on levodopa therapy [3]. Dyskinesia requires complex medical management and may adversely affect patients’ quality of life. To prevent or delay the development of dyskinesia, a number of underlying risk factors have been identified, such as levodopa use, young age at onset, low body weight, long duration of PD, and female gender [6,7,8,9,10].
Recent studies have highlighted the association between levodopa treatment and dyskinesia [6, 7, 11]. Notably, besides the choice of initial dopaminergic therapy, levodopa dose represents an important risk factor for dyskinesia [7, 12]. Substantial evidence indicates that higher doses of levodopa could provide greater antiparkinsonian effects, but are also associated with an increased risk for dyskinesia [7, 13]. Thus, identification of the threshold dose for dyskinesia may significantly improve the safety of levodopa therapy. The STRIDE-PD study [7] suggested that the incidence of dyskinesia in the < 400 mg/day levodopa dose group was markedly lower than the three other groups (400 mg/day; 400–600 mg/day; > 600 mg/day). However, the underlying threshold doses of the groups were prospectively and artificially defined rather than statistically yielded. In classification and assessment methods, recent studies have introduced receiver operating characteristic (ROC) and data mining methodology into classification assessment [14,15,16]. ROC represent a useful and reliable approach to obtain reasonable risk thresholds in clinical practice. Additionally, decision tree classification (DTC) model was a type of data mining method, which was a computational process of discovering patterns or classifications. In our previous study, ROC and DTC were eligibly used to define risk thresholds for wearing-off phenomenon in patients with PD [17]. Furthermore, although cumulative levodopa dose has been proposed as an independent risk factor for dyskinesia [6], the threshold value of cumulative levodopa dose for dyskinesia has not been investigated.
Several measures of levodopa dose have been investigated in previous study, including the initial levodopa dose [18], levodopa dose at onset of dyskinesia, levodopa equivalent dose (LEED), and weight-adjusted levodopa dose [12]. But few study have access these levodopa dose–related measures together in one study. The aim of the present study was to (1) explore which definition of levodopa dose is most accurately predictive for dyskinesia among multiple parameters of levodopa dose; (2) identify the risk thresholds of these levodopa dose–related measures for Chinese patients with PD using ROC and DTC analysis.
Materials and methods
Participants
A total of 403 patients with PD were recruited from the Department of Neurology in Beijing Tiantan Hospital between January 2017 and October 2018. Inclusion criteria were as follows: (1) a diagnosis of PD according to the Movement Disorder Society (MDS) Clinical Diagnostic Criteria for PD [19]; (2) disease duration > 1 year; (3) patients who had regular levodopa intake for at least 6 months and could provide reliable information about their dopaminergic drug use. Exclusion criteria were as follows: (1) atypical or secondary parkinsonian syndromes; (2) a history of stroke, moderate to severe head trauma, hydrocephalus, brain tumor, or deep brain stimulation implantation.
Data collection and assessment of motor complications
Demographic profile (gender, age, and exposure to caffeine) and clinical profile [age at onset, disease duration, H-Y stage, Mini-Mental State Examination (MMSE), Hamilton Anxiety Rating Scale (HAMA), Hamilton Depression Rating Scale (HAMD), Rapid Eye Movement Sleep Behavior Disorder Screening Questionnaire (RBDSQ), and Movement Disorder Society-Unified Parkinson’s Disease Rating Scale (MDS-UPDRS)] were collected for each patient. The history of the antiparkinsonian drugs used since disease onset and prescriptions, including changes in dose and the schedule of all drugs, was obtained from medical records. Dyskinesia and wearing-off were assessed by two experienced neurologists using the MDS-UPDRS Part IV, who were blinded to patients’ levodopa intake [20].
According to the previous study and clinical significance, nine levodopa dose–related variables were defined: daily dose (levodopa, LEED, LEED excluding amantadine), cumulative dose (levodopa, LEED, LEED excluding amantadine), and levodopa dose adjusted to weight (levodopa, LEED, LEED excluding amantadine). Variables characterizing levodopa use include daily levodopa dose (the dose patients were receiving at the time of onset of dyskinesia or the last dose if there was no dyskinesia) and cumulative levodopa dose (daily levodopa dose in grams multiplied by the number of days of levodopa therapy). LEED was determined using the following calculation protocol: LEED = levodopa dose + levodopa dose × 1/3 if on entacapone + piribedil (mg) + pramipexole (mg) × 100 + selegiline (mg) × 10 + amantadine (mg) + controlled release levodopa (mg) × 0.75 [21, 22]. Due to the potential anti-dyskinetic effect of amantadine, we also calculated for LEED excluding amantadine as the equivalent dose of all antiparkinsonian drugs except amantadine.
Statistical analysis
Statistical analyses were performed using SPSS 17.0 software (SPSS Inc., Chicago, IL, USA). The t test and x2 test were used to compare clinical features and measures of levodopa doses between groups. The Mann-Whitney test was used to compare differences between groups when the data were not normally distributed. Multivariate logistic regression analysis was used to assess the association between levodopa administration and the occurrence of dyskinesia in PD patients after adjusting for important confounders. P < 0.05 was regarded as statistically significant.
The ROC curve was applied to determine cut-off value of levodopa dose for predicting dyskinesia. DTC analysis was based on the classification and regression tree (CRT) and Gini index. CRT stratified the data using the best binary predictor to create high-risk and low-risk subgroups to demonstrate the greatest gain in overall subgroup homogeneity with respect to the outcome. To ensure that the risk thresholds for levodopa treatment were clinically practical, the classification performance of the proposed doses were assessed in terms of sensitivity, specificity and accuracy. Sensitivity was defined as the percentage of dyskinesia cases who received levodopa dose above the threshold dose, while specificity was defined as the percentage of non-dyskinesia cases if the levodopa doses were below the threshold dose. In addition, accuracy was defined as the ratio of corrected predictions for both the dyskinesia and non-dyskinesia cases.
Results
Comparison of demographic and clinical features between the non-dyskinesia and dyskinesia groups
Four hundred and three patients (female:male = 171: 232) were included in our study, of whom 110(27%) patients were diagnosed with dyskinesia, 284(70%) patients with wearing-off. The demographic and clinical characteristics of the non-dyskinesia and dyskinesia groups were listed in Table 1. Compared with those without dyskinesia, patients with dyskinesia had significantly lower weight [60(51–70) VS. 70(60–75), P < 0.001] and age at onset [53(46–60) VS. 58(52–64), P < 0.001], longer duration of PD [8(6–11) VS. 5(4–8), P < 0.001] and levodopa treatment [7(4–10) VS. 3(2–6), P < 0.001], higher H-Y stage [3(3–4) VS. 3(2–3), P < 0.001], and MDS-UPDRS Part III score [41(31–54) VS. 38(28–49), P = 0.048]. In addition, patients with dyskinesia were more likely to be female and to experience wearing-off phenomenon compared with those without dyskinesia. There were no differences in age, exposure to caffeine and scores in MDS-UPDRS Part I, MDS-UPDRS Part II, MMSE, HAMA, HAMD, and RBDSQ between the non-dyskinesia and dyskinesia groups.
Comparison of levodopa dose between the non-dyskinesia and dyskinesia group
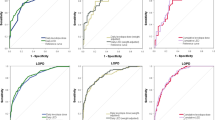
Patients with dyskinesia received significantly higher daily levodopa dose [600(450–800) mg/day VS. 300(200–450) mg/day, P < 0.001], cumulative levodopa dose [1013(601–1557) g VS. 324(131–648) g, P < 0.001], and daily levodopa dose adjusted to weight [10.0(7.6–13.3) mg/kg/day VS. 4.9(3.3–6.6) mg/kg/day, P < 0.001] than patients without dyskinesia. Similar results were obtained for LEED and LEED excluding amantadine. Details on the levodopa dose between non-dyskinesia and dyskinesia groups were shown in Table 2 and Fig. 1.
Scatter plots of levodopa dose distribution among the non-dyskinesia group and the dyskinesia group. Horizontal axis indicates levodopa dose. a Daily levodopa dose (mg/day). b Daily LEED (mg/day). c Daily levodopa dose adjusted to weight (mg/kg/day). d Daily LEED adjusted to weight (mg/kg/day). e Cumulative levodopa dose (g). f Cumulative LEED (g)
Relationship between levodopa dose and occurrence of dyskinesia
There were multiple levodopa-related variables involved in the multivariate model. According to the results of comparison between groups, six variables were selected to be included in the main logistic regression model: age at onset of PD, gender, weight, H-Y stage, MDS-UPDRS Part III score, and duration of PD. Additional analyses were performed to investigate the role of different treatment measures separately by creating models with the six basic variables together with the levodopa dose–related variable in turn. After adjusting for age at onset of PD, gender, weight, H-Y stage, MDS-UPDRS Part III score, and duration of PD, these levodopa dose-related variables remained associated with dyskinesia (Table 2).
Risk thresholds of levodopa treatment
Based on the ROC curve, a daily levodopa dose of 400 mg/day and 6.3 mg/kg/day was detected according to the largest Youden index. In addition, DTC model indicated that daily levodopa dose at 400 mg/day and 5.8 mg/kg/day were selected as the thresholds to best separate the dyskinesia group from the non-dyskinesia group (Fig.1). The risk thresholds and their classification performance were shown in Table 3.
Discussion
In the current study, we performed a detailed record of levodopa treatment–related variables and investigated their effects on the occurrence of dyskinesia.
After adjusted for demographical and clinical variables, daily levodopa dose, and cumulative levodopa dose as well as weight-adjusted levodopa dose were significantly associated with dyskinesia, suggesting that duration, daily dose, and weight-adjusted dose of levodopa use should be comprehensively considered in treatment of PD patients aiming to prevent and manage dyskinesia. Moreover, to our knowledge, this is the first study to investigate risk thresholds of levodopa for dyskinesia based on ROC and data mining approach. These results may help clinical practice and research design in the future.
Despite the previous studies revealed a significant positive relationship between levodopa dose and dyskinesia [6, 7, 12], the risk thresholds of levodopa for dyskinesia have been rarely explored. The threshold value of daily levodopa dose in our study is consistent with the previous study, which demonstrates that patients in the < 400 mg/day group experienced the lowest risk of developing dyskinesia [7]. In our study, the choice of the threshold dose was based on ROC analysis and DTC model [17]. It should be noted that, based on Chinese population, we reported exactly the same risk threshold of daily levodopa dose for dyskinesia using non-predefined data classification approach. However, in the high-risk groups such as early-onset PD patients, dyskinesia may still occur even with levodopa below the threshold dose, possibly due to the variability in genetic factors. For instance, a recent study showed that the polymorphisms of the dopamine transporter gene were associated with a risk of developing dyskinesia [23]. Further study should investigate these risk thresholds taking genetic factors into account.
In the present study, we also evaluated LEED of levodopa in combination with other dopaminergic drugs, as well as total dopaminergic drugs excluding amantadine. Our results suggest a higher risk thresholds of total dopaminergic drugs compared with the levodopa-only dose. Although this result is confounded by a significant difference in levodopa-only dose between the two groups, evidence suggests that the combined use of dopaminergic drugs may have protective effects against dyskinesia [24]. To date, the relationship between non-levodopa dopaminergic treatment and dyskinesia remains uncertain. A recent meta-analysis study showed a lower risk for dyskinesia in the dopamine agonist (DA) with adjunctive levodopa-treated group compared with levodopa-treated patients [24]. Further studies should explore the effect of non-levodopa dopaminergic treatments on dyskinesia separately in randomized controlled trials.
Beyond these observations, we recorded the full history of levodopa use and investigated the dose-effect relationship between accumulating levodopa exposure and dyskinesia. Our study indicated that Chinese PD patients taking cumulative levodopa dose > 536 g might be more likely to develop dyskinesia. Consistent with the previous study [25], these suggest that it is important to take a levodopa-sparing strategy in the early stage of PD, especially for early-onset patients. To date, the contribution of levodopa dose to the pathophysiology of dyskinesia is still poorly understood. Our results support the concept that the increased dopaminergic load on the receptors and the “threshold effect” according to plasma levodopa concentrations would likely contribute to the development of dyskinesia, which deserves further cellular and in vivo experiments.
There are some limitations to this study. Firstly, as a retrospective study, the results need to be further validated in prospective cohort. Secondly, dopamine transporter or monoamine oxidase type B gene polymorphism was not investigated in our study, while recent studies showed susceptibility of these gene polymorphism to the occurrence of dyskinesia [23]. Thirdly, subgroups based on different onset age or phenotypes are expected to be assessed separately as they may have different mechanism and may require different risk thresholds, which need larger PD cohort and is also our next step.
In conclusion, our study showed that taking a levodopa dose ≤400 mg per day could minimize the risk of dyskinesia in Chinese PD patients. Moreover, the potential threshold effect of levodopa dose for dyskinesia might help understand the pathophysiology of dyskinesia. Further prospective studies investigating levodopa-related factors in PD patients are needed to identify their risk thresholds for dyskinesia stratified by different clinical characteristics.
References
Kalia LV, Lang AE (2015) Parkinson’s disease. Lancet 386(9996):896–912
Aleksovski D, Miljkovic D, Bravi D, Antonini A (2018) Disease progression in Parkinson subtypes: the PPMI dataset. Neurol Sci 39(11):1971–1976
Chen W, Xiao Q, Shao M, Feng T, Liu WG, Luo XG, Chen XC, Xie AM, Liu CF, Liu ZG, Liu YM, Wang J, Chen SD (2014) Prevalence of wearing-off and dyskinesia among the patients with Parkinson’s disease on levodopa therapy: a multi-center registry survey in mainland China. Transl Neurodegener 3(1):26
Chen L, Duan WM, Mao GS (2015) Clinical neurorestorative progress in Parkinson’s disease. J Neurorestoratol 3(1):101–107
Ahlskog JE, Muenter MD (2001) Frequency of levodopa-related dyskinesias and motor fluctuations as estimated from the cumulative literature. Mov Disord 16(3):448–458
Scott NW, Macleod AD, Counsell CE (2016) Motor complications in an incident Parkinson’s disease cohort. Eur J Neurol 23(2):304–312
Warren Olanow C, Kieburtz K, Rascol O, Poewe W, Schapira AH, Emre M, Nissinen H, Leinonen M, Stocchi F, Stalevo Reduction in Dyskinesia Evaluation in Parkinson's Disease I (2013) Factors predictive of the development of Levodopa-induced dyskinesia and wearing-off in Parkinson’s disease. Mov Disord 28(8):1064–1071
Daneault JF, Carignan B, Sadikot AF, Panisset M, Duval C (2013) Drug-induced dyskinesia in Parkinson’s disease. Should success in clinical management be a function of improvement of motor repertoire rather than amplitude of dyskinesia? BMC Med 11:76
Ku S, Glass GA (2010) Age of Parkinson’s disease onset as a predictor for the development of dyskinesia. Mov Disord 25(9):1177–1182
Eusebi P, Romoli M, Paoletti FP, Tambasco N, Calabresi P, Parnetti L (2018) Risk factors of levodopa-induced dyskinesia in Parkinson’s disease: results from the PPMI cohort. NPJ Parkinsons Dis 4:33
Espay AJ, Morgante F, Merola A, Fasano A, Marsili L, Fox SH, Bezard E, Picconi B, Calabresi P, Lang AE (2018) Levodopa-induced dyskinesia in Parkinson disease: current and evolving concepts. Ann Neurol 84(6):797–811
Sharma JC, Ross IN, Rascol O, Brooks D (2008) Relationship between weight, levodopa and dyskinesia: the significance of levodopa dose per kilogram body weight. Eur J Neurol 15(5):493–496
Stocchi F, Rascol O, Kieburtz K, Poewe W, Jankovic J, Tolosa E, Barone P, Lang AE, Olanow CW (2010) Initiating levodopa/carbidopa therapy with and without entacapone in early Parkinson disease: the STRIDE-PD study. Ann Neurol 68(1):18–27
Aydemir O, Kayikcioglu T (2014) Decision tree structure based classification of EEG signals recorded during two dimensional cursor movement imagery. J Neurosci Methods 229:68–75
Stamp LK, Taylor WJ, Jones PB, Dockerty JL, Drake J, Frampton C, Dalbeth N (2012) Starting dose is a risk factor for allopurinol hypersensitivity syndrome: a proposed safe starting dose of allopurinol. Arthritis Rheum 64(8):2529–2536
Bellazzi R, Zupan B (2008) Predictive data mining in clinical medicine: current issues and guidelines. Int J Med Inform 77(2):81–97
Chen H, Fang J, Li F, Gao L, Feng T (2015) Risk factors and safe dosage of levodopa for wearing-off phenomenon in Chinese patients with Parkinson’s disease. Neurol Sci 36(7):1217–1223
Evans JR, Mason SL, Williams-Gray CH, Foltynie T, Brayne C, Robbins TW, Barker RA (2011) The natural history of treated Parkinson’s disease in an incident, community based cohort. J Neurol Neurosurg Psychiatry 82(10):1112–1118
Postuma RB, Berg D, Stern M, Poewe W, Olanow CW, Oertel W, Obeso J, Marek K, Litvan I, Lang AE, Halliday G, Goetz CG, Gasser T, Dubois B, Chan P, Bloem BR, Adler CH, Deuschl G (2015) MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord 30(12):1591–1601
Goetz CG, Tilley BC, Shaftman SR, Stebbins GT, Fahn S, Martinez-Martin P, Poewe W, Sampaio C, Stern MB, Dodel R, Dubois B, Holloway R, Jankovic J, Kulisevsky J, Lang AE, Lees A, Leurgans S, LeWitt PA, Nyenhuis D, Olanow CW, Rascol O, Schrag A, Teresi JA, van Hilten JJ, LaPelle N, Movement Disorder Society URTF (2008) Movement Disorder Society-sponsored revision of the unified Parkinson’s disease rating scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov Disord 23(15):2129–2170
Tomlinson CL, Stowe R, Patel S, Rick C, Gray R, Clarke CE (2010) Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov Disord 25(15):2649–2653
Mao CJ, Yang YP, Chen JP, Wang F, Chen J, Zhang JR, Zhang HJ, Zhuang S, Xiong YT, Gu CC, Yuan W, Huang JY, Fay A, Zhong CK, Liu CF (2018) Poor nighttime sleep is positively associated with dyskinesia in Parkinson’s disease patients. Parkinsonism Relat Disord 48:68–73
Purcaro C, Vanacore N, Moret F, Di Battista ME, Rubino A, Pierandrei S, Lucarelli M, Meco G, Fattapposta F, Pascale E (2018) DAT gene polymorphisms (rs28363170, rs393795) and levodopa-induced dyskinesias in Parkinson’s disease. Neurosci Lett 690:83–88
Chondrogiorgi M, Tatsioni A, Reichmann H, Konitsiotis S (2014) Dopamine agonist monotherapy in Parkinson’s disease and potential risk factors for dyskinesia: a meta-analysis of levodopa-controlled trials. Eur J Neurol 21(3):433–440
Cilia R, Akpalu A, Sarfo FS, Cham M, Amboni M, Cereda E, Fabbri M, Adjei P, Akassi J, Bonetti A, Pezzoli G (2014) The modern pre-levodopa era of Parkinson’s disease: insights into motor complications from sub-Saharan Africa. Brain 137 (Pt 10):2731–2742
Acknowledgments
This research was supported by the National Key R&D Program of China (no. 2016YFC1306501), the National Natural Science Foundation of China (no. 81571226, no. 81771367, and no. 31600724), Beijing Municipal Science and Technology Commission (no. z17110700100000, no. Z171100000117013). Beijing Nature Science Foundation (no. 7174297), and Beijing outstanding talents cultivation (no. 2016000021469G210).
Author information
Authors and Affiliations
Contributions
All authors have participated in the research and article preparation.
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the Ethics Committee of the Beijing Tiantan Hospital and was performed in accordance with the Declaration of Helsinki. Informed consent was obtained either from the participants or their closest relatives.
Conflict of interest
No conflict exist among authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, G., Chen, H., Su, D. et al. Risk thresholds of levodopa dose for dyskinesia in Chinese patients with Parkinson’s disease: a pilot study. Neurol Sci 41, 111–118 (2020). https://doi.org/10.1007/s10072-019-04043-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-019-04043-7